- Therapeutic Cataract & Refractive
- Lens Technology
- Glasses
- Ptosis
- AMD
- COVID-19
- DME
- Ocular Surface Disease
- Optic Relief
- Geographic Atrophy
- Cornea
- Conjunctivitis
- LASIK
- Myopia
- Presbyopia
- Allergy
- Nutrition
- Pediatrics
- Retina
- Cataract
- Contact Lenses
- Lid and Lash
- Dry Eye
- Glaucoma
- Refractive Surgery
- Comanagement
- Blepharitis
- OCT
- Patient Care
- Diabetic Eye Disease
- Technology
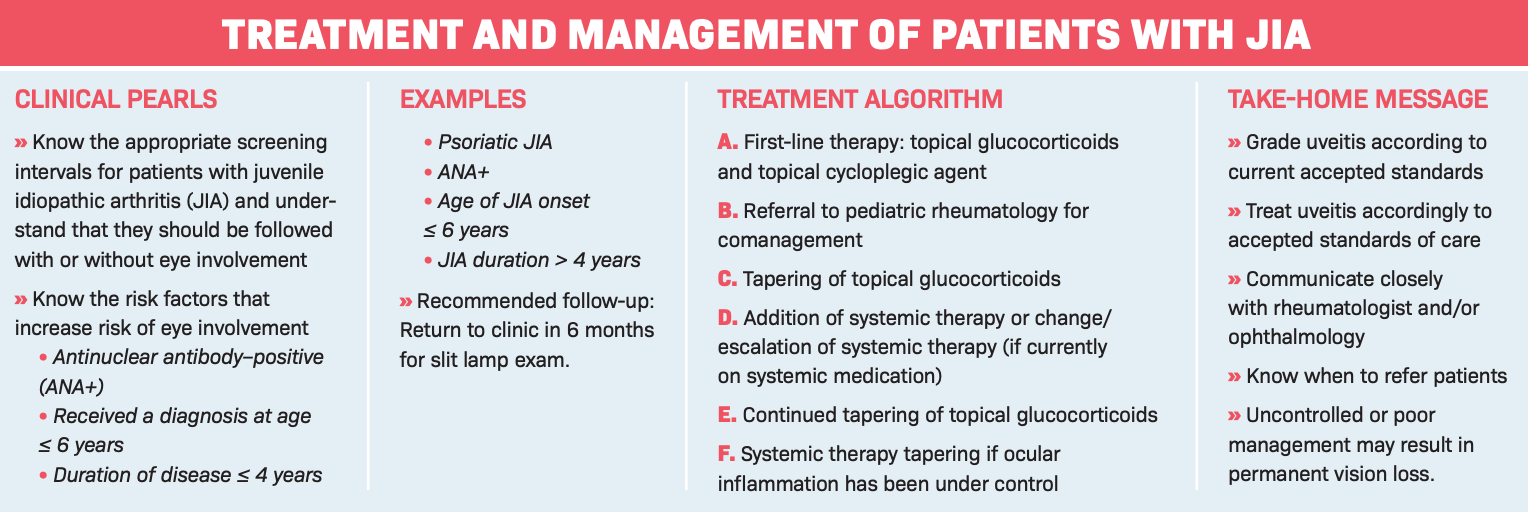
Classifying the challenges of juvenile idiopathic arthritis and pediatric uveitis
A review of monitoring guidelines, risk assessment, and treatment algorithms.
Pediatric uveitis, which accounts for approximately 5% to 10% of all uveitis cases, can present diagnostic and therapeutic challenges. Children may be asymptomatic despite severe inflammation. Pediatric uveitis is commonly bilateral, chronic, recurrent, and resistant to treatment.1
Examining a child can be difficult, particularly the evaluation of cell and flare with a slit lamp. Uveitis and its management pose a high risk of vision-threatening complications, including amblyopia, cataracts, glaucoma, synechiae, and band keratopathy.2 Additionally, there is the risk of visual loss and its impact on the child and family.
Classification
Classification of uveitis is typically based on anatomical location and onset, duration, course of uveitis, and grading of disease activity for reproducible assessment and monitoring of disease.
Anatomically, it is classified as anterior (iris and ciliary body), intermediate (vitreous and pars plana), or posterior (choroid and/or retina) uveitis; or panuveitis, which is all 3—anterior, intermediate, and posterior uveitis.
Course of uveitis is defined as acute (sudden onset, lasting for less than 3 months), recurrent (repetitive episodes separated by quiescent periods lasting more than 3 months), and chronic (persistent uveitis for more than 3 months).
Grading of disease activity is broken down into the number of cells seen in a 1×1 mm slit beam in the slit lamp.3Additionally, uveitis can be granulomatous or nongranulomatous.
JIA
Juvenile idiopathic arthritis (JIA) is the most common type of arthritis in children, affecting approximately 294,000 pediatric patients in the United States. JIA is defined as arthritis of unknown etiology that begins before the patient turns 16 years old and persists for at least 6 weeks.4
The common subtypes of JIA are oligoarticular/pauciarticular (50%-70%), where the arthritis affects 4 or fewer joints (knees); polyarticular (30%), where the arthritis affects more than 4 joints (usually 10-20 joints); and systemic (1%-5%), where patients have a characteristic rash and fever.5
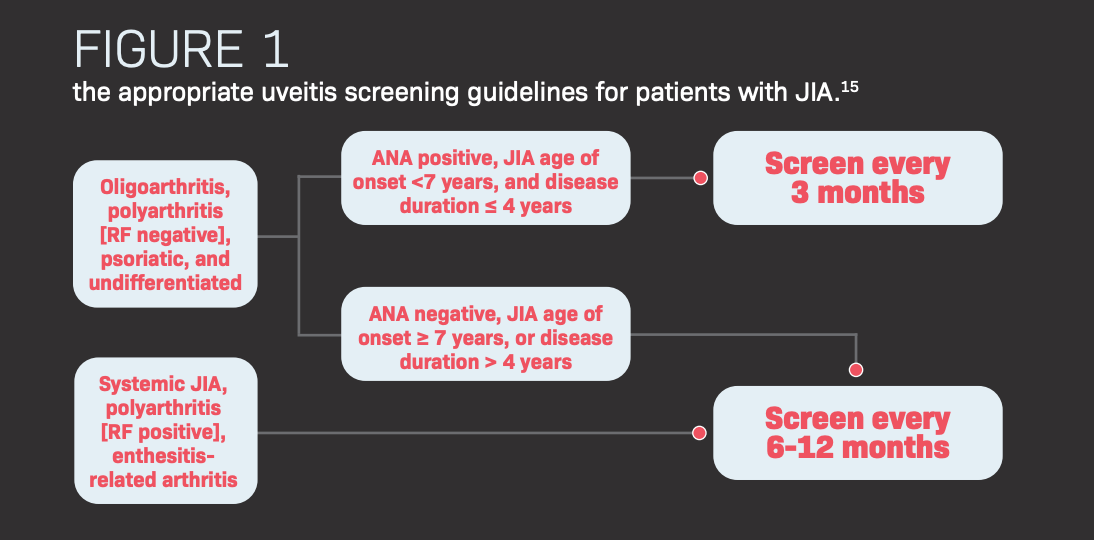
Studies report that 10% to 25% of children with JIA also will develop uveitis.6 Patients with JIA are at the highest risk of developing uveitis within the first 4 years of onset.6
Only in 5% of cases does the uveitis precedes the arthritis.7 Although JIA affects females more than males (3:2),8,9 uveitis associated with patients with JIA who are antinuclear antibody–positive (ANA+) does not have a gender predilection.10,8
Predictive values for uveitis
There are 3 positive predictive values for patients with JIA in developing uveitis. Patients who tested positive on the ANA test are more likely to develop uveitis.11 Studies found that 60% to 90% of patients who develop uveitis are ANA+.7 Patients who receive a diagnosis for JIA at an early age are more likely to develop uveitis.
Secondly, the closer the time from onset of receiving the JIA diagnosis, the more likely the patient will develop uveitis.12,7 Studies found that 35.5% of patients developed uveitis within the first 2 months, 73% of patients developed uveitis within the first year, and 88.7% of patients developed uveitis within the first 4 years.13
Finally, patients who were younger than the age of 4 were at the highest risks of developing uveitis.12,14 Therefore, the recommendation for regular screening is <7 years of age is due to the higher risk of uveitis in patients who are at a younger age and the closer the time from onset of their JIA.
Treatment and complications of uveitis
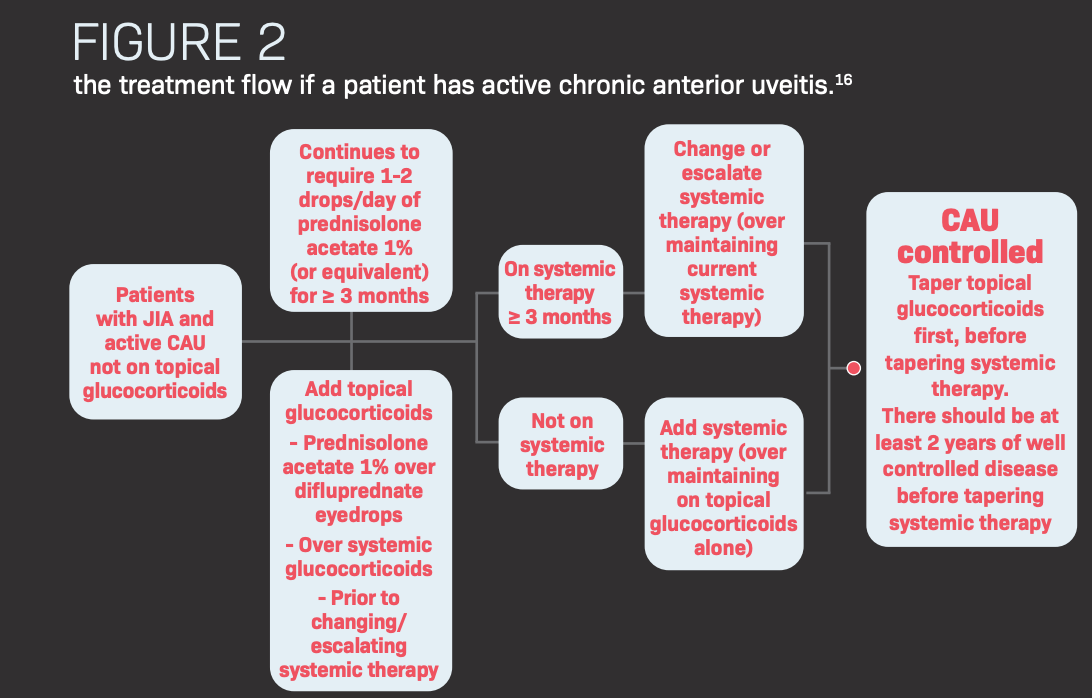
Approximately 80% of uveitis cases in children are associated with JIA.16 Uveitis associated with JIA is bilateral in 70% to 80% of cases, typically anterior involving the iris and ciliary body. The initial approach to managing JIA uveitis in children is with topical corticosteroids (eg, prednisolone acetate 1%).
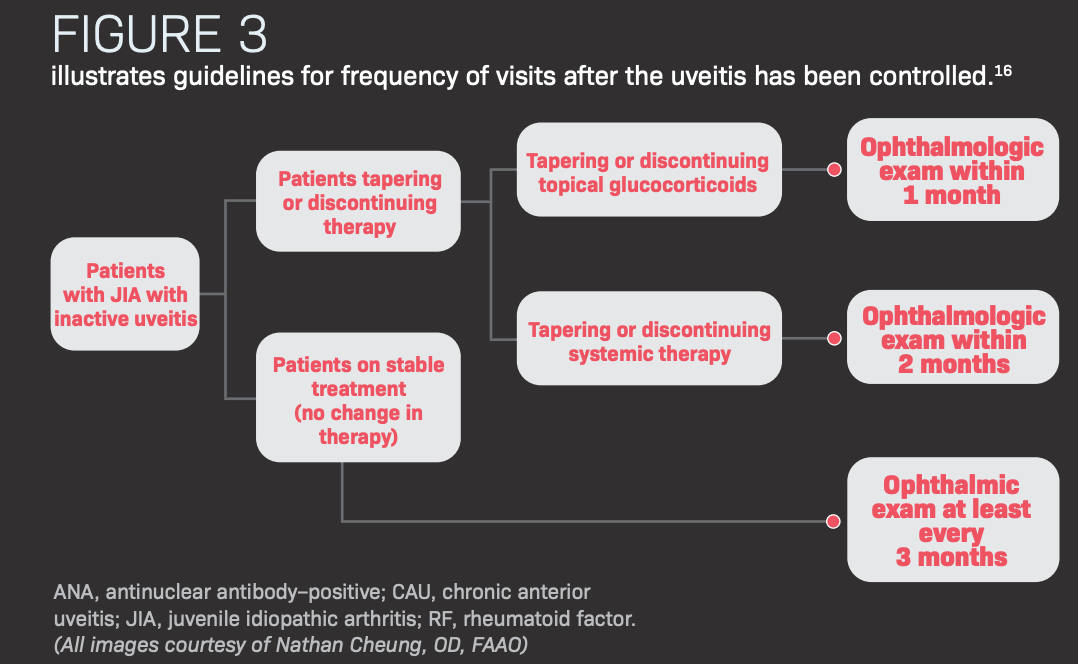
Patients with JIA and uveitis should be followed regularly; those with more severe conditions will require more frequent follow-up. As with any prolonged steroid treatment, consideration must be given for a slow/systematic taper.
Monitoring for a steroid response should be part of every follow-up visit, and the practitioner should be prepared to use IOP-lowering agents in conjunction if indicated.
Very often the patient will be on systemic medications to control the JIA: nonsteroidal anti-inflammatory drugs (NSAIDs) such as tolmetin (Tolectin), naproxen (Aflaxen), or ibuprofen; corticosteroids, intravenous or intraarticular; disease-modifying antirheumatic drugs such as methotrexate (Otrexup, Rasuvo) and sulfasalazine (Azulfidine); or anti–tumor necrosis factor (TNF) inhibitors and monoclonal antibodies such as etanercept (Enbrel), adalimumab (Humira), or infliximab (Remicade).
Generally, NSAIDs and corticosteroids are used for short periods of time and long-term use is discouraged. All systemic medications other than NSAIDs can aid in the treatment of uveitis.
Common complications of uncontrolled JIA uveitis include cataracts, glaucoma, band keratopathy, posterior synechiae, and ocular hypotony. Patients with more severe disease and requiring cataract extraction typically have an earlier mean onset of uveitis.
A multidisciplinary team approach is necessary to treat patients with JIA. Open communication and close management with rheumatology and/or ophthalmology are important.
References
- Chan NSW, Choi J, Cheung CMG. Pediatric uveitis. Asia Pac J Ophthalmol. May-Jun 2018; 7(3):192-199. doi:10.22608/APO.2018116
- Angeles-Han S, Yeh S. Prevention and management of cataracts in children with juvenile idiopathic arthritis-associated uveitis. Curr Rheumatol Rep. 2012;14(2):142-149. doi:10.1007/s11926-011-0229-z
- Jabs DA, Nussenblatt RB, Rosenbaum JT; Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the first international workshop. Am J Ophthalmol. 2005; 140(3):509-516. doi:10.1016/j.ajo.2005.03.057
- Oberle EJ, Harris JG, Verbsky JW. Polyarticular juvenile idiopathic arthritis- epidemiology and management approaches. Clin Epidemiol. 2014;6:379-393. doi:10.2147/CLEP.S53168
- Petty RE, Southwood TR, Manners P, et al; International League of Associations for Rheumatology. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol. 2004;31(2): 390-392.
- Constantin T, Foeldvari I, Anton J, et al. Consensus-based recommendations for the management of uveitis associated with juvenile idiopathic arthritis: the SHARE initiative. Ann Rheum Dis. 2018;77(8):1107-1117. doi:10.1136/annrheumdis-2018-213131
- Cassidy J, Kivlin J, Lindsley C, Nocton J; Section on Rheumatology; Section on Ophthalmology. Ophthalmologic examinations in children with juvenile rheumatoid arthritis. Pediatrics. 2006;117(5):1843-1845. doi:10.1542/peds.2006-0421
- Heinz C, Mingles A, Goebel C, Fuchsluger T, Heiligenhaus A. Chronic uveitis in children with and without juvenile idiopathic arthritis: differences in patient characteristics and clinical course. J Rheumatol. 2008;35(7):1403-1407.
- Kotaniemi K, Savolainen A, Karma A, Aho K. Recent advances in uveitis of juvenile idiopathic arthritis. Surv Ophthalmology. 2003;48(5):489-502. doi:10.1016/s0039-6257(03)00084-5
- Heiligenhaus A, Klotsche J, Tappeiner C, et al. Predictive factors and biomarkers for the 2-year outcome of uveitis in juvenile idiopathic arthritis: data from the Inception Cohort of Newly Diagnosed Patients With Juvenile Idiopathic Arthritis (ICON-JIA) study. Rheumatology (Oxford). 2019 Jun 1; 58(6):975-986. doi:10.1093/rheumatology/key406
- Bolet IB, Cannizzaro E, Seger R, Saurenmann RK. Risk factors and longterm outcome of juvenile idiopathic arthritis-associated uveitis in Switzerland. J Rheumatol. 2008;35(4):703-706
- Angeles-Han ST, McCracken C, Yeh S, etc. Characteristics of a cohort of children with juvenile idiopathic arthritis and JIA-associated uveitis. Pediatr Rheumatol Online J. Published online June 2, 2015. doi:10.1186/s12969-015-0018-8
- Grassi A, Corona F, Casellato A, Carnelli V, Bardare M. Prevalence and outcome of juvenile idiopathic arthritis-associated uveitis and relation to articular disease. J Rheumatol. 2007;34(5):1139-1145.
- Heligenhaus, A. Niewerth M, Ganser G, Heinz C, Minden K; German Uveitis in Childhood Study Group. Prevalence and complications of uveitis in juvenile idiopathic arthritis in a population-based nation-wide study in Germany: suggested modification of the current screening guidelines. Rheumatology (Oxford). 2007;46(6):1015-1019. doi:10.1093/rheumatology/kem053
- Angeles-Han ST, Ringold S, Beukelman T, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Screening, Monitoring, and Treatment of Juvenile Idiopathic Arthritis-Associated Uveitis. Arthritis Care & Research 2019;71(6):703-716. doi:10.1002/acr.23871
- Wentworth BA, Freitas-Neto CA, Foster CS. Management of pediatric uveitis. F1000 Prime Rep. 2014;6:41.

