- Therapeutic Cataract & Refractive
- Lens Technology
- Glasses
- Ptosis
- AMD
- COVID-19
- DME
- Ocular Surface Disease
- Optic Relief
- Geographic Atrophy
- Cornea
- Conjunctivitis
- LASIK
- Myopia
- Presbyopia
- Allergy
- Nutrition
- Pediatrics
- Retina
- Cataract
- Contact Lenses
- Lid and Lash
- Dry Eye
- Glaucoma
- Refractive Surgery
- Comanagement
- Blepharitis
- OCT
- Patient Care
- Diabetic Eye Disease
- Technology
Helping Dry Eye Associated with Sjögren's Syndrome: A Case Study
With a diverse array of tools at our disposal to address ocular surface diseases we as optometrists possess the ability to tailor treatments to the unique needs of each patient. Regener-Eyes® has proven to be an asset in my practice. I have one case to share with you that reignited my enthusiasm for the comprehensive solutions that we provide in our exam rooms. After enduring years of persistent dry eye symptoms and ocular discomfort my patient finally found relief.
Initial Visit
A 75-year-old-female presented as a walk-in with bilateral symptoms, that have been ongoing for the past two days with no signs of improvement, of conjunctival injection, intense itching, mild ocular pain, purulent discharge, foreign body sensation, and blurred vision. Her previous ocular history included years of keratoconjunctivitis sicca, superior limbic keratoconjunctivitis and meibomian gland dysfunction. She has Rheumatoid Arthritis, controlled by hydroxychloroquine and methotrexate for more than twenty years, and has been on adalimumab and celecoxib for two years. Her ocular medications at this time were cyclosporine 0.05%, cromolyn sodium, and artificial tears. Her last screening for hydroxychloroquine retinopathy was completed a few months prior to this encounter. Entering best corrected visual acuity was OD 20/200 and OS 20/80. Intraocular pressures were within normal limits. There was no preauricular lymphadenopathy. Slit lamp examination revealed an equal presentation in both eyes of mattering of the eyelashes with purulent discharge, toothpaste expression of the meibomian glands, 1+ conjunctival injection, instant tear break-up time with a decreased lacrimal lake and grade 2+ superficial punctate keratitis 360. No signs of any dendrites were seen. Corneal sensitivity was normal in all quadrants, and she reported complete relief of pain after instillation of 1 gtt proparacaine 0.5% The signs and symptoms seen at this first visit indicated that she had bacterial conjunctivitis1. I had her discontinue all previous eyedrops. I prescribed moxifloxacin TID OU, eyelid hygiene wipes as needed for the ocular discharge and to change all bedding to prevent re-infection with instructions to return to clinic in 3 days due to her discomfort.
Follow-Up #1
At her follow-up visit all her signs and symptoms were improving, except for her SPK. A review of her charts revealed that she has had a pattern of cyclical superficial punctate keratitis, about once every 6 months since 2015. To continue to quiet everything down I took her off the moxifloxacin and started her on neomycin-polymyxin-dexamethasone gtts QHS OU to stabilize her ocular surface and had her back in one week.
Follow-Up #2
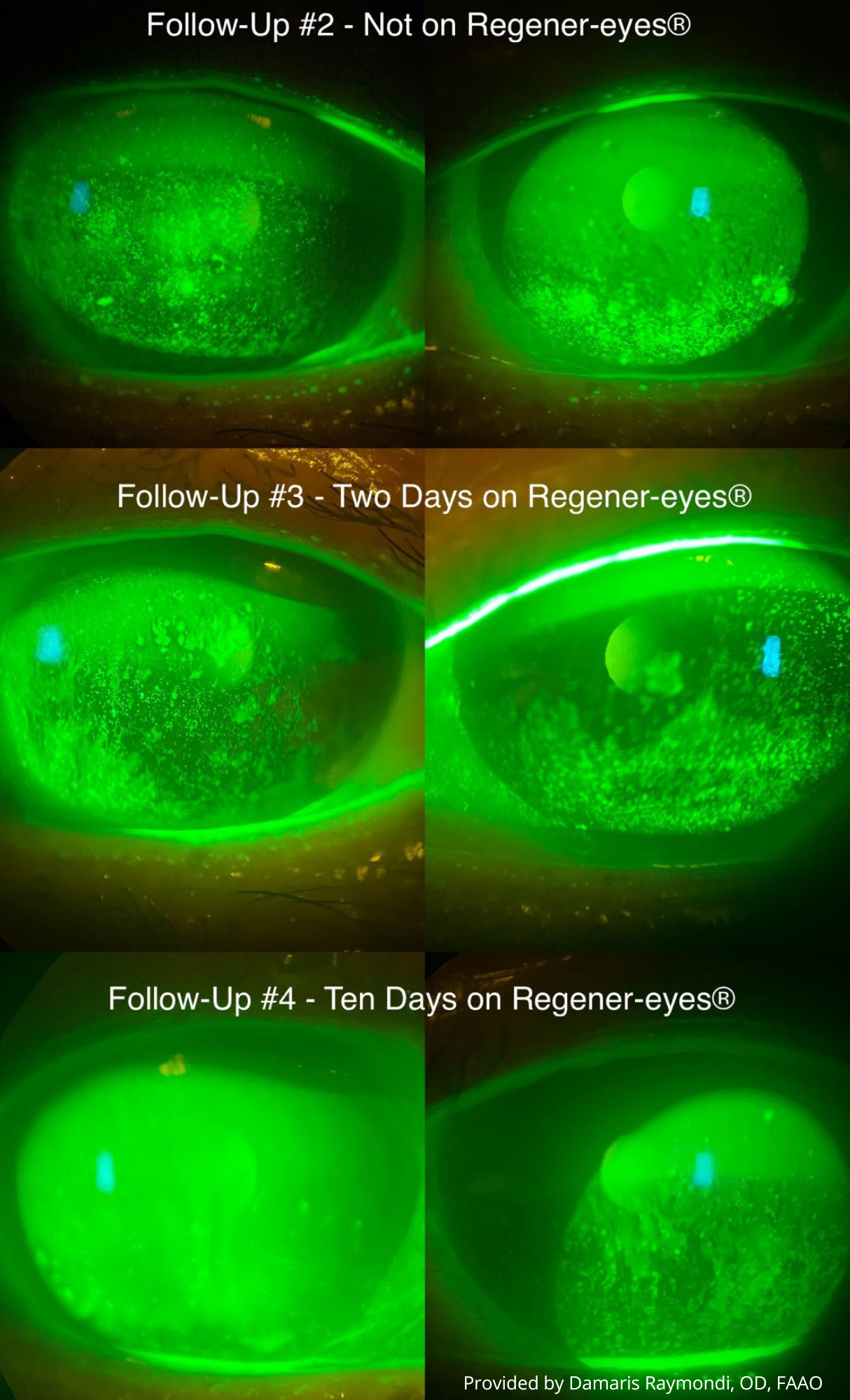
Given the cyclical destabilization of her ocular surface and the well-established challenges posed by the pathophysiological mechanisms of dry eye and meibomian gland dysfunction in treating ocular surface diseases, it became apparent that a comprehensive approach targeting multiple areas within this double-vicious circle2 was necessary. Consequently, my initial focus was on reducing my patient's bacterial load. I used a heat pack to melt her meibum, instilled proparacaine 0.5%, used meibomian gland compressor forceps on all her eyelids, removing significant turbid meibum, and cleaned up the lid margins before and after with a corneal spud. These recurrences, difficulty controlling her SPK, scant tear film and a diagnosis of rheumatoid arthritis3 prompted me to order bloodwork to test for Sjögren’s. The plan was to discontinue all drops for one week, to remove the effect of any topical preservatives/additives, and to only then start Regener-Eyes® LITE 1 gtt twice a day OU.
Follow-Up #3
At this visit the patient has been on Regener-Eyes® LITE for two days. Her bloodwork came back positive for anti-Ro and anti-La antibodies. The diagnosis of secondary Sjögren’s was communicated to her rheumatologist. In just these two days she reported significant relief in all her symptoms. The SPK was still present but with improvement, as seen in the figure. I repeated the meibomian gland expression procedure with the use of a heat pack, forceps, and corneal spud. I had her continue Regener-Eyes® LITE gtts twice a day OU, and no other gtts, for another week.
Follow-Up #4
The photos in the figure are taken after the patient was on Regener-Eyes® LITE for ten days. Significant improvement was achieved in signs and symptoms and dramatic improvement was seen in her SPK. She was no longer in pain, no itching, no discharge, no injection, no foreign body sensation. Most impressive of all, her best corrected visual acuity was at OD 20/0 and OS 20/20. She reported instant relief upon instillation of Regener-Eyes® gtts and I had her continue it, still twice a day in both eyes, with a follow-up in one month.
Follow-Up #5
After more than one month of being on Regener-Eyes® LITE there was complete resolution of all signs and symptoms with no recurrences. Her ocular surface was pristine and stable with a tear break-up time of 10 seconds. It was at this point that punctal plug insertion was considered, as there were no signs of inflammatory markers present, and I prescribed cyclosporine 0.05% along with Regener-Eyes® LITE. Patient is doing so well, seeing clearly, and feeling relief.
Regener-Eyes® played a crucial role in stabilizing her ocular surface. It also enabled me to provide relief sooner, avoiding the wait for insurance approval. The ability of the tears to create a stable surface as well as the composition of the tears is what we need to make sure that a patient’s eyes feel happy and comfortable. Regener-Eyes® was able to quickly achieve that for my patient and that is something the two of us will always be thankful for.
References
- Friedman, N. J., Kaiser, P. K., & Pineda, R. (2021). Conjunctivitis. In The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology (pp. 145–152). Elsevier.
- Baudouin C, Messmer EM, Aragona P, Geerling G, Akova YA, Benítez-del-Castillo J, Boboridis KG, Merayo-Lloves J, Rolando M, Labetoulle M. Revisiting the vicious circle of dry eye disease: a focus on the pathophysiology of meibomian gland dysfunction. Br J Ophthalmol. 2016 Mar;100(3):300-6. doi: 10.1136/bjophthalmol-2015-307415. Epub 2016 Jan 18. PMID: 26781133; PMCID: PMC4789719.
- Caffery, Barbara; Simpson, Trefford†; Wang, Sunny‡; Bailey, Denis; McComb, John; Rutka, John; Slomovic, Allan; Bookman, Arthur. Factor Analysis of the Clinical Characteristics of Primary Sjögren Syndrome. Optometry and Vision Science 87(10):p 742-750, October 2010. | DOI: 10.1097/OPX.0b013e3181f32196
