- Therapeutic Cataract & Refractive
- Lens Technology
- Glasses
- Ptosis
- AMD
- COVID-19
- DME
- Ocular Surface Disease
- Optic Relief
- Geographic Atrophy
- Cornea
- Conjunctivitis
- LASIK
- Myopia
- Presbyopia
- Allergy
- Nutrition
- Pediatrics
- Retina
- Cataract
- Contact Lenses
- Lid and Lash
- Dry Eye
- Glaucoma
- Refractive Surgery
- Comanagement
- Blepharitis
- OCT
- Patient Care
- Diabetic Eye Disease
- Technology
PDR: public health considerations
Proper screenings, treatment, management needed for this increasingly prevalent disease.
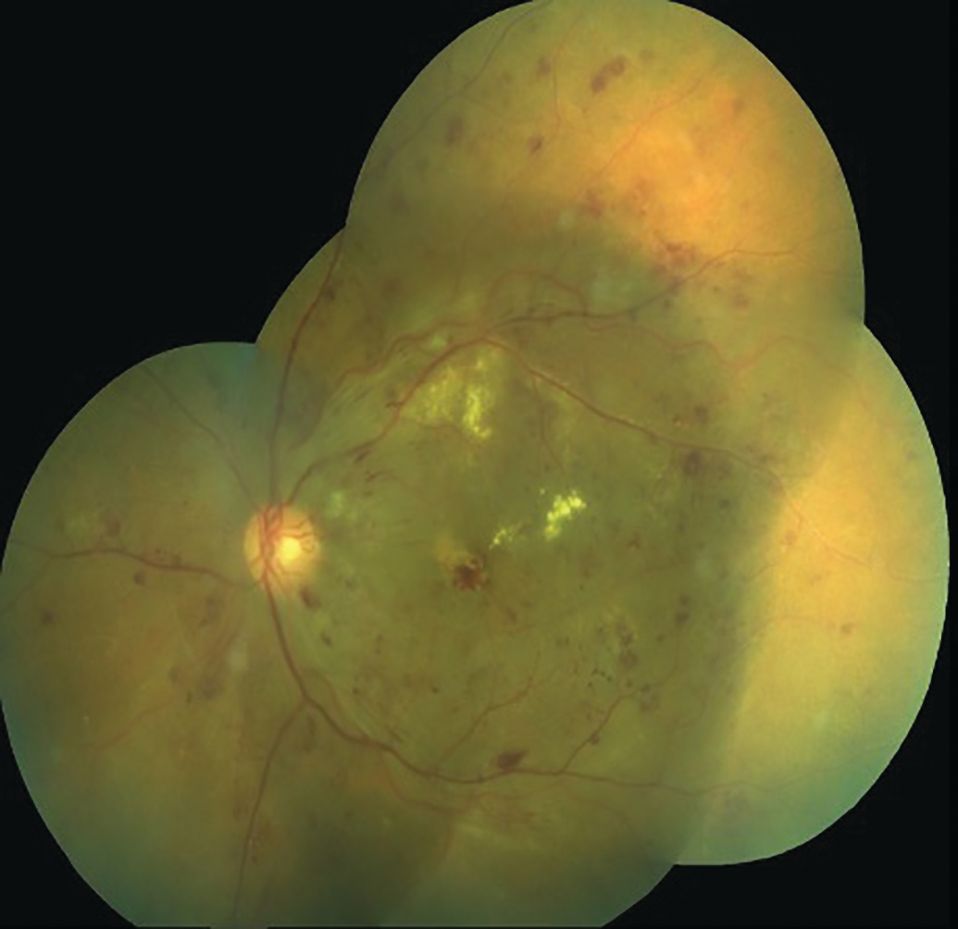
Diabetic retinopathy (DR) is one of the leading causes of morbidity and vision loss worldwide, and its diagnosis is based on vascular irregularities found in the retina upon clinical examination. The disease is divided into nonproliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR).1
PDR occurs in less than 2% of patients with type 2 diabetes within 5 years of diagnosis.2 The incidence of diabetes and related complications is disproportionately higher in minority populations.
NPDR is further categorized into 4 stages: mild, moderate, severe, and very severe. Diabetic macular edema (DME), a complication characterized by abnormal leakage and accumulation of fluid affecting central vision, can occur in any stage.
There is a strong correlation between chronic hyperglycemia and the development of DR. The pathophysiology of microvascular damage is unclear, with many biochemical processes cited as the cause.3
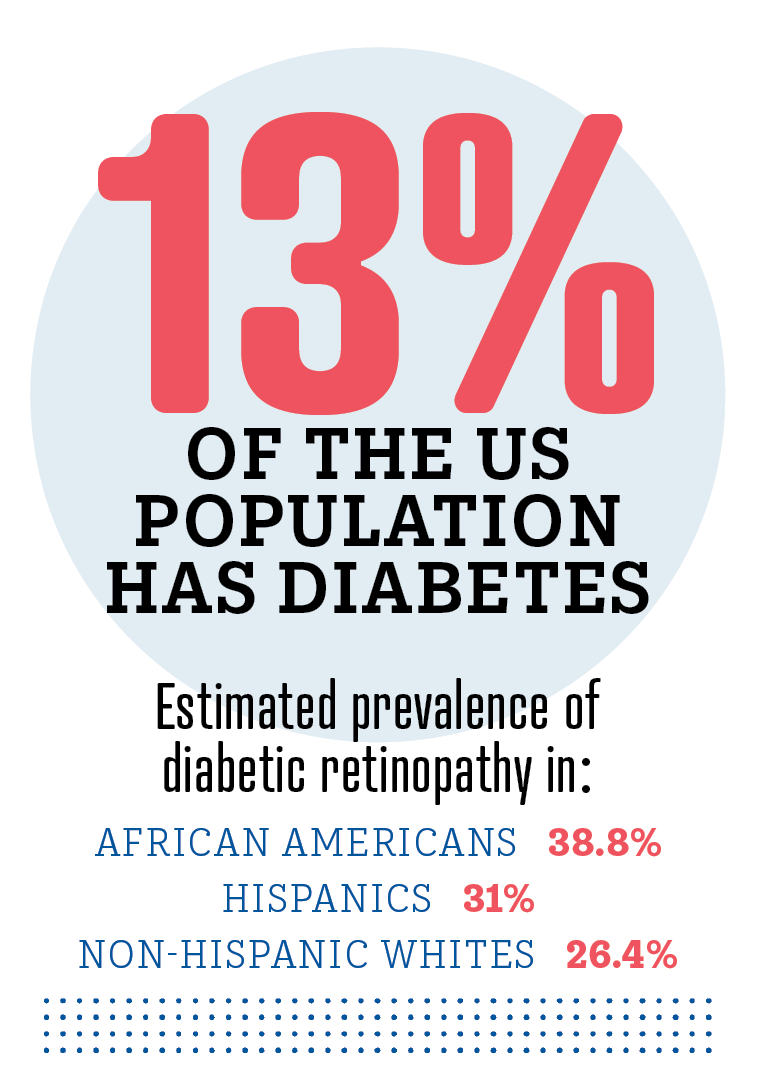
Minority populations experience higher rates of microvascular complications compared to Caucasian adults. The estimated prevalence of DR is 38.8% in African Americans, 31% in Hispanics, and 26.4% in non-Hispanic Whites.4 The incidence of such complications as cardiovascular and cerebrovascular diseases is also higher in ethnic and minority populations.
DR is managed with anti-vascular endothelial growth factor (anti-VEGF), panretinal photocoagulation (PRP), and vitrectomy. These treatments aim to reduce new vessel growth (neovascularization), decrease swelling (ie, macular edema), and eliminate vitreous hemorrhages, respectively.5 Patient education about blood sugar control is also extremely important in preventing recurrence of retinopathy.
The global prevalence of DR is 22.27%: 6.17% of these cases threaten vision and 4.07% involve clinically significant macular edema (CSME).6 South Asian, African, Latin American, and individuals of Indigenous descent have a higher incidence of DR, vision-threatening DR, and CSME than Caucasian individuals.7
In mild cases of DR, patients may be asymptomatic, and signs are only noted upon fundus examination. In more severe cases, symptoms include blurry vision, central metamorphopsia, floaters, and acute vision loss.
DR is a microvascular disease primarily caused by the metabolic impact of chronic hyperglycemia, and theories abound as to its pathophysiology. Severity depends on the type of diabetes mellitus, time since onset, glycemic control status, and presence of smoking and comorbidities like hypertension, chronic kidney disease, and hyperlipidemia.
Type I DM is a genetic disorder in which insulin is not produced. In type II DM, the pancreas cannot produce enough insulin, or the insulin does not function optimally.8 The blood-retinal barrier is disrupted in DR, which leads to leakage and degradation of the neurovascular unit in the retina.
Vascular endothelial growth factor (VEGF) also plays a role in blood vessel leakage. The molecular processes involved include the polyol pathway, advanced glycation end-product formation, protein kinase C activation, renin-angiotensin aldosterone system activation, oxidative stress, and loss of pericyte function.2,9,10
Pericytes are specialized mesenchymal cells within capillaries that regulate vascular tone and perfusion pressure. The connection between pericytes and endothelial cells may be disrupted by a thickening of the basement membrane, hyperglycemia, advanced glycation end-product formation, and hypoxia leading to pericyte apoptosis and neovascularization.10
Table
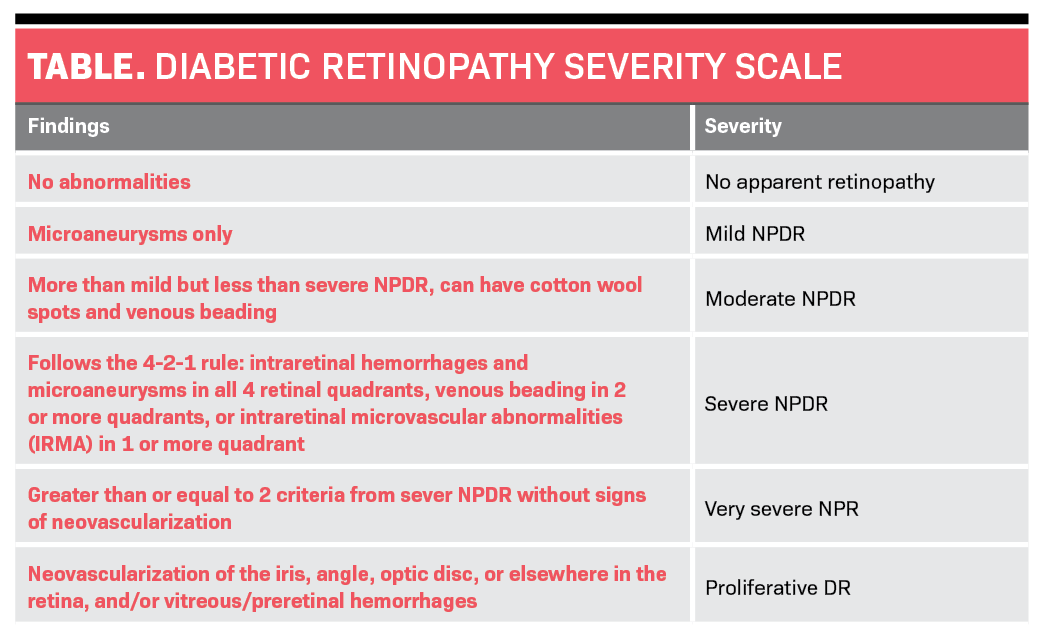
DR can occur unilaterally or bilaterally and presents with any HbA1c level. Clinical findings in NPDR include microaneurysms, retinal hemorrhages, venous caliber changes, cotton wool spots, and microvascular abnormalities. According to the Modified Airlie House Classification, DR can be proliferative and nonproliferative (Table).
Categorization
Within nonproliferative retinopathy, there are mild, moderate, severe, and very severe categories. Mild NPDR consists of microaneurysms only. Moderate involves more than microaneurysms but is less than severe NPDR; eyes will show an increase in IRH, microaneurysms, hard exudates, and cotton wool spots (CWS).
Severe NPDR follows the 4-2-1 rule: IRH and microaneurysms in all 4 retinal quadrants, venous beading in 2 or more quadrants, and intraretinal microvascular abnormalities (IRMA) in 1 or more quadrants. Very severe NPDR is greater than or equal to 2 criteria from severe NPDR without signs of neovascularization.
PDR is characterized by neovascularization of the iris angle (rubeosis iridis), optic disc, or elsewhere and preretinal and vitreous hemorrhages.11 PDR may also involve vitreous or preretinal hemorrhages. High risk characteristics are the presence of neovascularization elsewhere (NVE), neovascularization of the disc (NVD), and vitreous or preretinal hemorrhage.12
CSME develops owing to a breakdown in the blood-retinal barrier and can present at any stage of DR.13
The Early Treatment Diabetic Retinopathy Study (ETDRS) classified CSME as retinal thickening within 500 μm of the foveal center, retinal exudates within 500 μm of the foveal center with adjacent thickening, and retinal thickening greater than 1 disc diameter in size within 1 disc diameter of the foveal center.14
Given the prevalent use of OCT to investigate macular edema, many practitioners no longer adhere to a strict ETDRS criteria for CSME but opt to describe DME as central and noncentral.
Depending on the location of the edema and its effect on visual acuity, the clinician decides whether it is best to treat promptly or to monitor closely.
Differential diagnosis
Differentials of PDR include hypertensive retinopathy, sickle cell retinopathy, central retinal artery or vein occlusions, and branch retinal vein occlusions.
Hypertensive retinopathy is associated with high blood pressure and ocular signs such as flame hemorrhages, artery tortuosity, arteriovenous nicking, and papilledema.
Sickle cell retinopathy can occur in patients affected by sickle cell and includes “sea fans” of neovascularization. Left untreated, sea fans can lead to retinal detachment.
Retinal vein and artery occlusions are caused by blockages like thrombus and emboli and may be associated with both diabetic and hypertensive retinopathy.15
Treatment and management
Diabetic macular edema
Treatment of vision-threatening DME includes anti-VEGF agents, FDA-approved ranibizumab (Lucentis, Roche), and aflibercept (Eylea, Regeneron). Bevacizumab (Avastin, Roche) is used off-label as another treatment option. Anti-VEGF is the first-line treatment for DME involving the fovea.16 Other treatment options are focal/grid laser photocoagulation and intraocular steroids.
Dexamethasone (Ozurdex, Allergan) is a vitreous implant that slowly releases steroids to reduce inflammation associated with macular edema. Its side effects include cataract progression and IOP elevation.17 Depending on visual acuity, observation is an appropriate management for noncentral DME.15,16
Proliferative diabetic retinopathy
PRP has been proven to be an effective PDR treatment that decreases the risk of severe vision loss. PRP is theorized to improve retinal oxygenation by eliminating areas of hypoxic retina. Anti-VEGF can be used in combination with PRP, with or without pars plana vitrectomy (PPV). PPV is indicated in cases of dense vitreous hemorrhage, traction, and severe retinal neovascularization.18
Systemic blood sugar control
Blood sugar control is extremely important in reducing the risk of diabetic complications and comorbidities such as kidney disease, retinopathy, stroke, and heart failure. It is vital to communicate these risks to patients and coordinate care with their primary care providers and endocrinologists.
Current research suggests that rapid decreases in blood glucose can lead to early worsening of DR. Rapid decrease in blood glucose can be induced with blood pressure control, changes in osmotic pressure, and diabetic treatment like insulin therapy.
The osmotic pressure hypothesis states that water moves from high to low pressure levels, such as small vessels within the eye, with rapid drops in HbA1c, thereby exacerbating retinopathy.
One retrospective study of retinal images in patients with type 2 diabetes who participated in the Diabetes Program at Harbor-UCLA Medical Center in West Carson, California, demonstrated that a decrease in HbA1c of 4% over a 13-month period resulted in worsening of retinopathy by 23% as compared to the control group.
Table 1
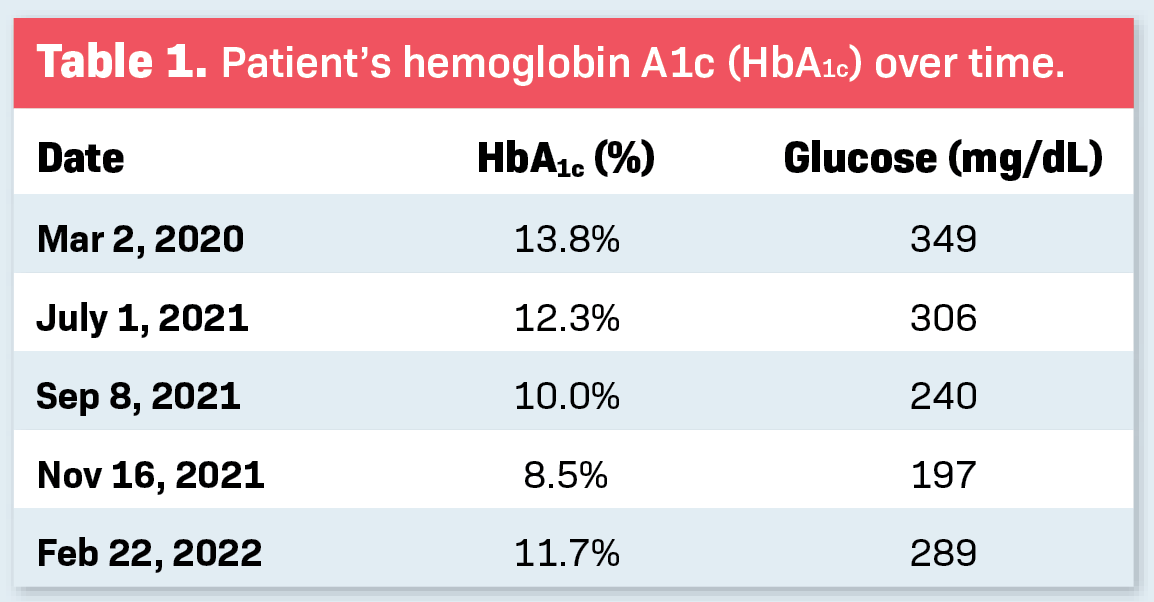
The patient discussed in the case report had a 3.8% decrease in HbA1c level over a 5-month period, from July 2021 to November 2021 (Table 1). It is hypothesized that intensive HbA1c control over a short time period can worsen DR. Worsening, in these cases, is defined as the appearance of cotton wool spots, soft exudates, hemes, and intraretinal microvascular abnormalities. The mechanism behind worsening includes microvascular perfusion abnormalities, insufficient blood supply to arteriosclerotic vessels, and impaired autoregulation.19
The Diabetes Control and Complications Trial (DCCT) states that vigorous glycemic control reduces the incidence and progression of diabetic complications in type 1 diabetes. There is uncertainty about whether this is true for type 2 diabetes, as research has shown intensive control can lead to hyperinsulinemia, increased hypoglycemia, and weight gain.20
Research conducted by the United Kingdom Prospective Diabetes Study (UKDPS) provided guidelines for the management of type 2 diabetes. It found that lowering blood sugar reduces the incidence of microvascular complications in type 2 diabetes and that blood pressure control helps reduce rates of cardiovascular complications.21
The Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial showed that intensive therapy to reduced HbA1c levels for 3.5 years increased mortality rates and did not reduce cardiovascular events in patients with type 2 diabetes. However, it did delay albuminuria onset and some eye complications. ACCORD also showed that targeted blood pressure control of less than 120 mm Hg versus less than 140 mm Hg did not reduce the rate of fatal and nonfatal cardiovascular events.22
Systemic comorbidities impacting DR progression
A variety of diabetic comorbidities exist, including retinopathy, obesity, cardiovascular disease, kidney disease, neuropathy, nephropathy, metabolic syndrome, neovascular glaucoma, and cataracts.
The patient in this case had retinopathy, early cataracts, chronic kidney disease, hypertension, and hyperlipidemia. Impaired glucose tolerance is shown to be associated with increased risk of cardiovascular complications. Treatment of both high blood glucose and blood pressure in patients with glomerular hyperfiltration can decrease the risk of kidney damage.23
Public health outreach and education
In the US, DR disproportionately affects racial and ethnic minorities and people of lower socioeconomic status. About 13% of the US population has diabetes; of that group, 14.7% are Indian Americans/Alaska Natives, 12.5% are Hispanic, 11.7% are African Americans, 9.2% are non-Hispanic Asians, and 7.5% are non-Hispanic Whites.14
African Americans and Hispanic adults also have higher rates of retinopathy and poor glycemic control than non-Hispanic Whites. Microvascular complications like retinopathy, nephropathy, and lower extremity amputations also occur more frequently in minorities.
Studies show that minority patients are less likely to obtain preventive diabetic care like annual exams and screenings.15 Current research aims to better understand the differences in incidence rates between different ethnic groups.
Social and economic issues, transportation difficulties, and lack of health literacy can be barriers to health care for minorities. And patients of lower socioeconomic status are less likely to access prevention services owing to language barriers, rejection of care, and distrust of the medical system.
In one study by Walter et al, only 36% of African American patients had heard of retinopathy, and only 8% described it accurately. Patient education is of great importance in order to decrease rates of diabetes and diabetic complications.24
Conclusion
The prevalence of diabetes continues to increase at an exponential rate around the world. To prevent vision loss, eye-care providers must advocate for annual exams to monitor diabetic changes and initiate proper treatment and management.
