- Therapeutic Cataract & Refractive
- Lens Technology
- Glasses
- Ptosis
- AMD
- COVID-19
- DME
- Ocular Surface Disease
- Optic Relief
- Geographic Atrophy
- Cornea
- Conjunctivitis
- LASIK
- Myopia
- Presbyopia
- Allergy
- Nutrition
- Pediatrics
- Retina
- Cataract
- Contact Lenses
- Lid and Lash
- Dry Eye
- Glaucoma
- Refractive Surgery
- Comanagement
- Blepharitis
- OCT
- Patient Care
- Diabetic Eye Disease
- Technology
Implementing a glaucoma screening program using the Laroche Glaucoma Risk Calculator
The Laroche Glaucoma Risk Calculator is a valuable tool for glaucoma screenings both in the community and in optometrist offices.
Optometrists and allied health care professionals play a pivotal role in the early detection of glaucoma. Glaucoma development and progression increases with age and is a leading cause of preventable blindness globally.1 Nearly half of patients who have glaucoma in the United States are unaware, increasing the likelihood of long-term poor visual outcomes.2,3 With advancing age, the prevalence of glaucoma increases, affecting Black Americans nearly 3 times more than white Americans.4,5 Additionally, given the shifting demographics in the country, the largest demographic group with primary open-angle glaucoma is expected to change to Hispanic men in the coming decades.6
A novel glaucoma risk calculator
Large clinical trials have extensively studied the risk factors associated with the onset and progression of glaucoma, including older age, increased IOP, larger vertical cup-to-disc ratio, thinner central corneal thickness (CCT), and decreased mean deviation of the visual field. In studies such as the Ocular Hypertension Treatment Study and the European Glaucoma Prevention Study, these factors were used to calculate the risk of ocular hypertension advancing to glaucoma.
Although prior calculators demonstrated success in estimating glaucoma risk, these tools were designed to be used by physicians with access to equipment needed to visualize the optic nerve and expertise in interpreting visual fields, eliminating the potential use of the calculator by nonphysicians in under-resourced areas. Nonphysician allied health personnel, particularly in under-resourced areas, can play an important role in preventing blindness through early glaucoma detection.
In response to these drawbacks, the Laroche Glaucoma Risk Calculator was created as a minimally invasive, low-cost method to predict the risk of glaucoma, educate patients, and reenforce adherence. With a timely, complete eye evaluation, the Laroche Glaucoma Risk Calculator uses 3 known risk factors for glaucoma: age, IOP, and CCT. There is no need for a fundus examination or visual field testing as a part of this screening.
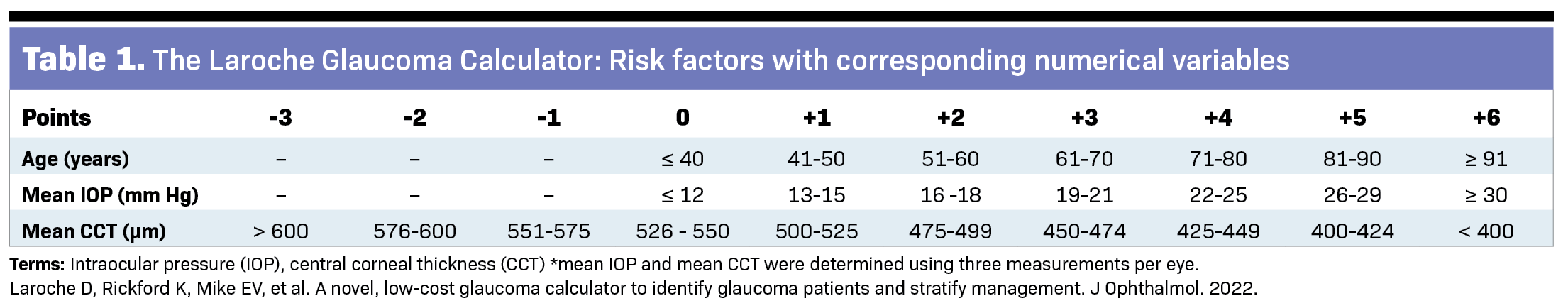
Each risk factor was designated a numerical variable between –3 and +6 (Table 1) to create a composite score that effectively stratifies patients based on their risk of developing glaucoma (Table 2).
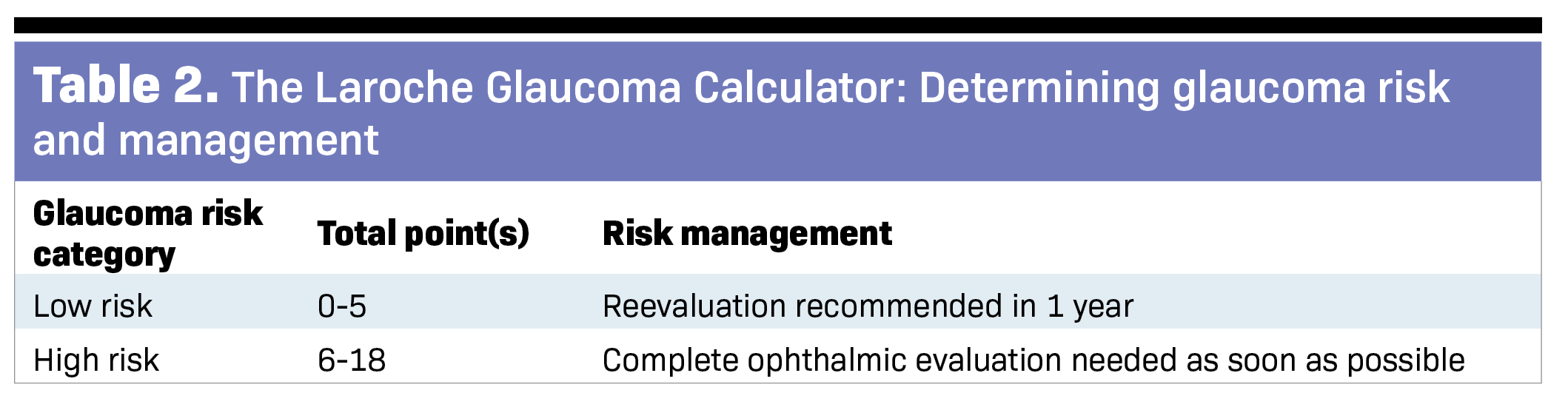
Findings from the preliminary study examining the effectiveness of the Laroche Glaucoma Risk Calculator in detecting glaucoma in 54 of 104 eyes revealed a high sensitivity (90.74%), specificity (64.00%), and correct classification (77.88%), with a cutoff composite score of greater than or equal to 6.7 Therefore, those with a composite score of greater than or equal to 6 using this tool are considered high risk for glaucoma.
Current uses of the Laroche Glaucoma Risk Calculator
Use of the Laroche Glaucoma Risk Calculator is currently taking place in medical offices and higher-risk New York communities by trained medical students and allied health technicians.
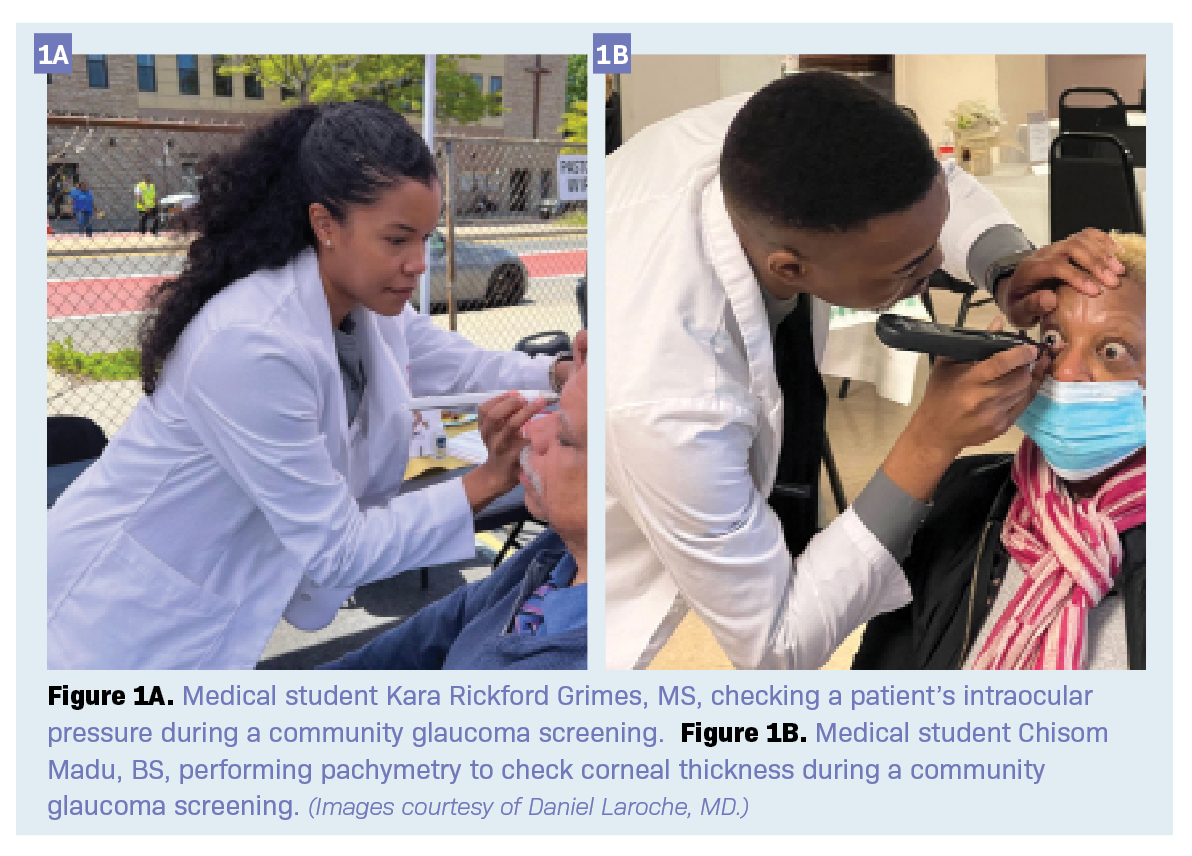
The target population for screening include individuals older than 40 years in under-resourced areas who can benefit greatly from early glaucoma testing. Medical personnel conducting the glaucoma screenings in this study are medical students trained to administer eye drops (eg, proparacaine) and operate a handheld Pachmate 2 pachymeter (DGH Technology; Figure 1a) and a Tono-Pen XL Tonometer (Medtronic; Figure 1b). These portable devices make glaucoma screenings more affordable and accessible to communities both inside and outside medical offices. Optometrists can add this to their in-office glaucoma screening and community glaucoma screening programs.
Current data analyzed from a glaucoma screening in Southeast Queens, New York, have shown promising findings. Of the 44 participants screened, nearly 30% were identified as being high risk by the Laroche Glaucoma Calculator in at least 1 eye. Those considered high risk for glaucoma presented at an older age (74 years, high risk; 60 years, low risk), with higher IOP (11.42 mm Hg, low risk; 28.75 mm Hg, high risk) and lower CCT (550.00 µm, low risk; 540.57 µm, high risk).
Participants in our community screenings who are considered high risk are referred for a free comprehensive eye examination with an optometrist or ophthalmologist at a participating medical office to encourage follow-up and reduce barriers in access to care. Results from the ongoing community glaucoma screenings have supported the findings in the initial study, demonstrating effectiveness of this screening tool in identifying patients with glaucoma and education about annual eye care.
Creating a glaucoma community screening
The purpose of community screenings is not only to detect early glaucoma but also to educate members of the community on glaucoma and encourage annual eye examinations. The following steps were taken to implement a community glaucoma screening and can be used nationwide:
- Identify high population areas (eg, places of worship, community centers) in remote locations with limited resources.
- Schedule and advertise glaucoma screening within this community. This can be done with local community organizations or groups that have fairs or gatherings planned.
- Gather nonphysician medical personnel trained (by an optometrist or ophthalmologist) to operate a pachymeter and tonometer and insert numbing eye drops to the patient’s eyes.
- Complete the glaucoma screening (including signed consent forms) and gather contact/demographic data.
- Record screening results and calculate glaucoma risk using the Laroche Glaucoma Risk Calculator. (Please note, the calculator must be downloaded to calculate risk.)
- Inform the patient of low or high glaucoma risk.
- Provide all participants with a handout detailing glaucoma risk and recommended follow-up for complete eye examination.
- Inform the patient that the screening does not replace a full ophthalmic examination, which is recommended once a year.
- Individuals identified as high risk for glaucoma should immediately be referred to an ophthalmologist or optometrist to complete a full eye examination.
Increasing community awareness of glaucoma and follow-up care
Although glaucoma is a leading cause of preventable blindness, many individuals are unaware of the risk factors associated with glaucoma and may also be unaware of their diagnosis, and these numbers are far greater in under-resourced areas. When completing a glaucoma screening, it is important to empower participants with the knowledge of this condition through verbal explanation and handout material. Interactions of nonphysician medical personnel in glaucoma community screenings can be a very useful resource in building patient trust and education.
Many glaucoma screening programs may benefit most from improved follow-up care. It is important to exchange contact information with participants to ensure they are provided with the details of where to complete a comprehensive eye examination. Additionally, collecting contact information from participants with their consent can help encourage high-risk patients to seek treatment. Conversations with participants may assist in identifying and addressing barriers in access to care.
Conclusion

The Laroche Glaucoma Risk Calculator is a valuable tool for glaucoma screenings both in the community and in optometrist offices by allied health technicians and students under optometrist and physician supervision. Please contact Daniel Laroche, MD, for more information on glaucoma screenings using the Laroche Glaucoma Risk Calculator.
Dr. Laroche would like to thank Black EyeCare Perspective for the introduction to Optometry Times. To learn more about Black EyeCare Perspective, please visit their website.
References
1. GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the right to sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health.2021;9(2):e144-e160. doi:10.1016/S2214-109X(20)30489-7
2. Nayak BK, Maskati QB, Parikh R. The unique problem of glaucoma: under-diagnosis and over-treatment. Indian J Ophthalmol.2011;59(suppl 1):S1-S2. doi:10.4103/0301-4738.73677
3. Varma R, Ying-Lai M, Francis BA, et al. Prevalence of open-angle glaucoma and ocular hypertension in Latinos: the Los Angeles Latino Eye Study. Ophthalmology.2004;111(8):1439-1448. doi:10.1016/j.ophtha.2004.01.025
4. Salowe R, Salinas J, Farbman NH, et al. Primary open-angle glaucoma in individuals of African descent: areview of risk factors. J Clin Exp Ophthalmol.2015;6(4):450. doi:10.4172/2155-9570.1000450
5. Friedman DS, Jampel HD, Muñoz B, West SK. The prevalence of open-angle glaucoma among blacks and whites 73 years and older: the Salisbury Eye Evaluation Glaucoma Study. Arch Ophthalmol.2006;124(11):1625-1630. doi:10.1001/archopht.124.11.1625
6. Vajaranant TS, Wu S, Torres M, Varma R. The changing face of primary open-angle glaucoma in the United States: demographic and geographic changes from 2011 to 2050. Am J Ophthalmol.2012;154(2):303-314.e3. doi:10.1016/j.ajo.2012.02.024
7. Laroche D, Rickford K, Mike EV, et al. A novel, low-cost glaucoma calculator to identify glaucoma patients and stratify management. J Ophthalmol.2022;2022:5288726. doi:10.1155/2022/5288726