- Therapeutic Cataract & Refractive
- Lens Technology
- Glasses
- Ptosis
- AMD
- COVID-19
- DME
- Ocular Surface Disease
- Optic Relief
- Geographic Atrophy
- Cornea
- Conjunctivitis
- LASIK
- Myopia
- Presbyopia
- Allergy
- Nutrition
- Pediatrics
- Retina
- Cataract
- Contact Lenses
- Lid and Lash
- Dry Eye
- Glaucoma
- Refractive Surgery
- Comanagement
- Blepharitis
- OCT
- Patient Care
- Diabetic Eye Disease
- Technology
Know 4 types of allergic eye disease
Flip the eyelids to uncover the clinical features of allergic conjunctivitis
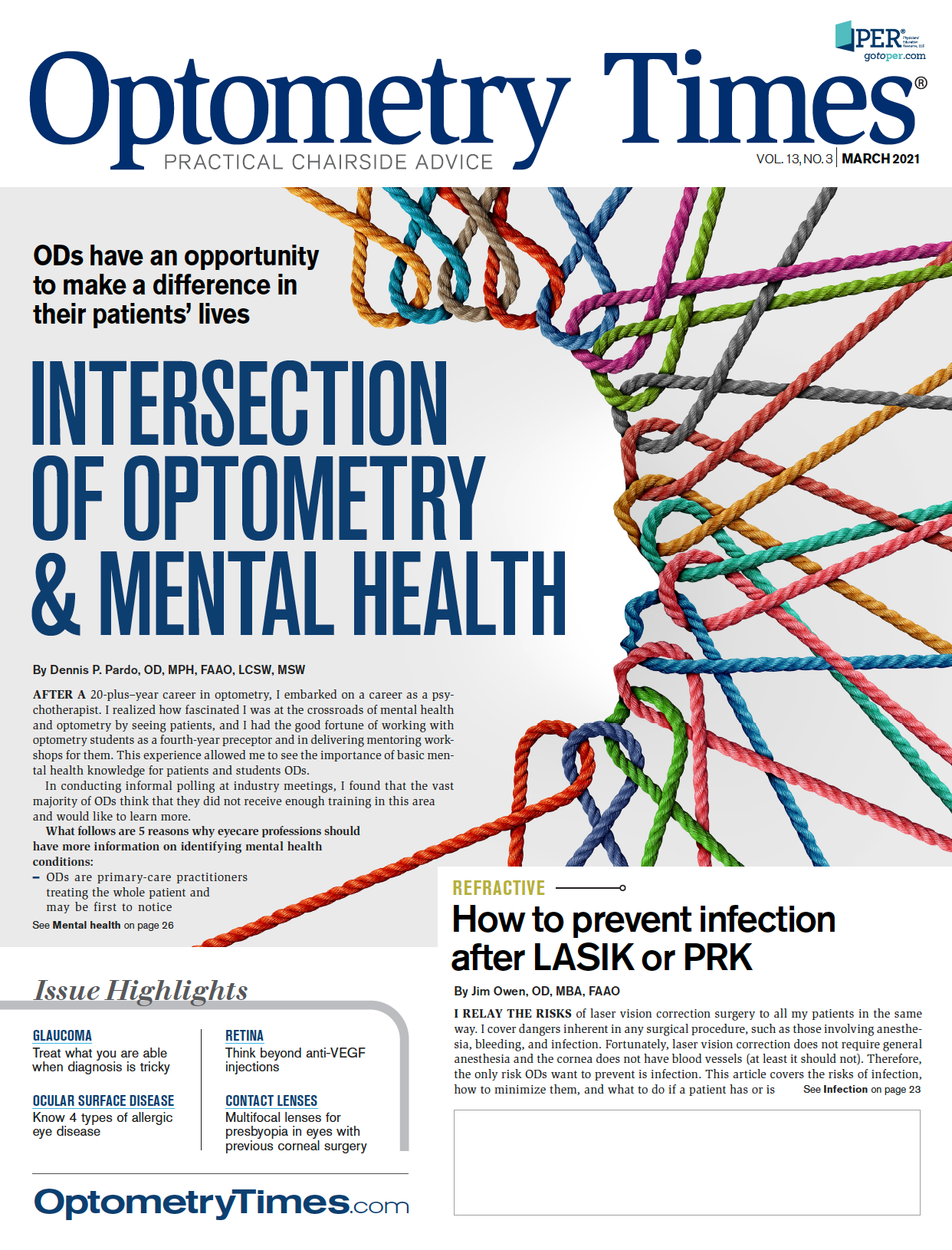
Allergies are the sixth leading cause of chronic illness in the United States with an annual cost exceeding $18 billion.1 Within ocular allergy, allergic conjunctivitis is an all-inclusive term that encompasses seasonal allergic conjunctivitis (SAC), perennial allergic conjunctivitis (PAC), vernal keratoconjunctivitis (VKC), and atopic keratoconjunctivitis (AKC).2
Many phenotypes of allergic eye disease exist; however, it is important to remember the treatment plan is not one size fits all. The ability to identify clinical features, pathophysiology and ideal treatment options for each type is crucial to delivering appropriate clinical care.
SAC and PAC
CLINICAL PRESENTATION
Often undiagnosed and undertreated, SAC and PAC represent 2 of the most common acute forms of allergic conjunctivitis and affects approximately 15% to 20% of the global population.2 SAC is more common and usually caused by seasonal allergens (ie, grass, tree pollen), with worsened symptoms in the spring and summer months.3 PAC symptoms can occur throughout the year and are caused by exposure to non-seasonal allergens (ie, cigarette smoke, dust mites, animal dander).3
Affecting people of all ages, both SAC and PAC typically present with itching, redness, and a clear, watery discharge. Complaints of intermittent blurry vision, burning, and photophobia may indicate allergies; however, these symptoms are consistent with other ocular surface diseases as well. It is important to flip the eyelids to check for the presence of allergic papillae.
Conjunctival papillae are classic findings in allergic eye disease and are comprised of elevated clusters of eosinophils. They contribute to the foreign body sensation often described by patient as “gritty,” “sandy,” and “scratchy.”2 In contrast to other inflammatory allergic eye conditions that can cause permanent vision loss, SAC and PAC rarely exhibit significant corneal involvement.2
PATHOPHYSIOLOGY
SAC and PAC involve an immediate (type 1) hypersensitivity reaction in response to an immunoglobulin E-mediated cell (IgE) activation.2 The infiltration of eosinophils and neutrophils results in mast cell degranulation and release of histamine and other pro-inflammatory cytokines that further amplify the inflammatory response.2 This rapid secretion of histamine causes the hallmark symptom of itching.
The presence of specific IgE antibodies can be documented in almost all cases of SAC and PAC.2 Patients who suffer from these conditions are at higher risk for atopy, a genetic predisposition to develop an allergic hypersensitivity reaction upon exposure to a specific environmental allergen.2
TREATMENT
In addition to preservative-free artificial tears and cold compresses, it is important that allergy patients avoid eye rubbing. With mild or acute itching symptoms, OTC antihistamines can help provide immediate relief. Topical mast-cell stabilizers are beneficial long term for patients with chronic symptoms. Dual-action drugs (that combine antihistamines with mast-cell stabilizers) are available and helpful to improve patient compliance due to reduced frequency of application.
Topical steroids are occasionally prescribed for short-term treatment of moderate to severe SAC and PAC. Oral antihistamines and nasal corticosteroids have also been effective for patients experiencing concomitant allergic rhinoconjunctivitis. These patients would benefit from consultation with an allergist or immunologist.
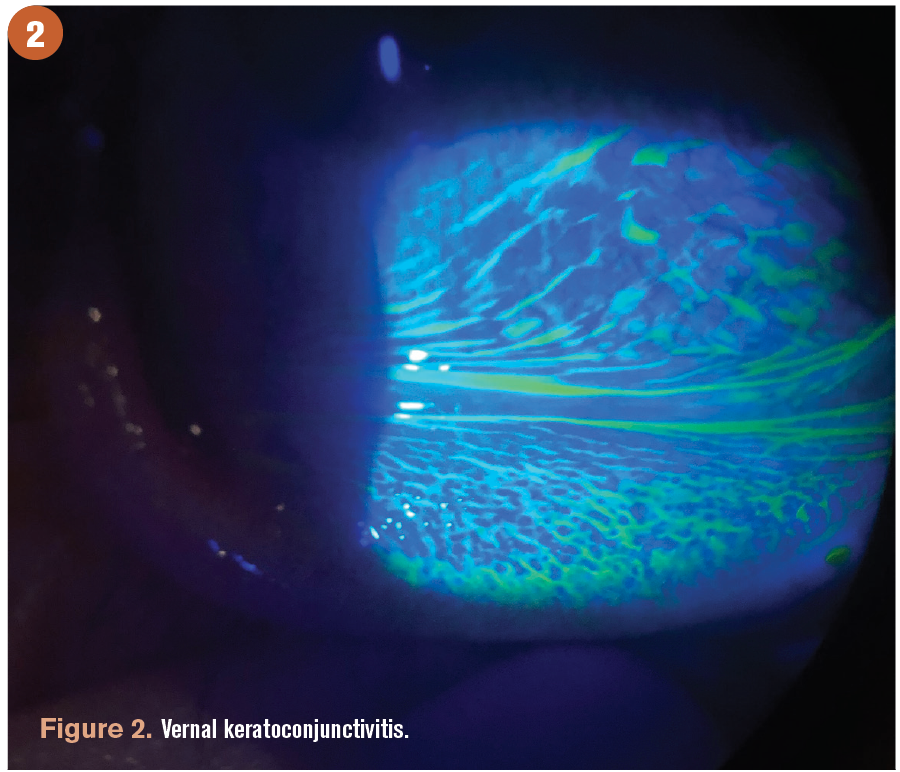
VKC
CLINICAL PRESENTATION
VKC can be unilateral or bilateral and most commonly affects boys aged 4 to 12 years.3
Different from seasonal and perennial allergies, VKC often resolves after puberty and presents during the warm weather months and in dry, arid climates.3 Classic signs of VKC include giant cobblestone papillae and Horner-Trantas dots.
There are 2 types of VKC; each is characterized by the location of ocular signs. The limbal form of VKC is more common in tropical environments and characterized by Horner-Trantas dots and papillae along the limbal area.4 The palpebral form of VKC presents with large cobblestone papillae on the upper tarsal plate and is more commonly seen in western locations.4 Patients can also be affected by a mixture of both limbal and palpebral forms of VKC.
Peri-limbal Horner-Trantas dots consist of clumps of necrotic eosinophils, neutrophils, and epithelial cells; therefore, patients with active VKC often present with significant discomfort due to intense itching, foreign body sensation, tearing, pain, and photophobia.3 Corneal involvement is not uncommon and ranges from mild (punctate epithelial erosions) to severe (macroerosions and shield ulcers).4
PATHOPHYSIOLOGY
The exact mechanism of VKC is not entirely known; however, it is thought to be a combination of both IgE and non-IgE mechanisms.3 VKC is thought to involve an IgE mediated hypersensitivity as well as T-cell involvement in the reaction, which may explain the increase in severity, corneal involvement, and duration of disease compared to more common ocular allergy types.4 This massive eosinophil infiltration in the conjunctiva of patients with VKC is likely responsible for the chronic corneal complications.3 The fact that patients “outgrow” the condition after puberty may also suggest a hormonal component.3
The tears of VKC patients have been found to contain high levels of IgE and mast-cell mediators in addition to histamine, leukotrienes, prostaglandins, and kinase.3 In contrast to seasonal and perennial allergies, skin tests and/or serum IgE antibody tests to common allergens are often negative in patients with VKC.2
TREATMENT
Given the level of inflammation associated with VKC, antihistamine therapy alone is often unsuccessful. A short course of topical corticosteroid may be indicated in the acute phase to control ocular inflammation. Once controlled, calcineurin inhibitors and other immunomodulators such as cyclosporine (off label) have proven effective in preventing exacerbations.5 Nonpharmacologic treatment recommendations such as wind and sun avoidance with sunglasses and hats are also encouraged.
VKC is a complicated condition and multiple specialties are often required to determine an etiology and appropriate long term management.
AKC
CLINICAL PRESENTATION
AKC is a rare, chronic inflammatory allergic condition and is considered an ocular manifestation of atopic dermatitis. Given its root of atopy, AKC almost always presents bilaterally, although one eye may be worse than the other. Symptoms typically persist throughout life, and there is no specific seasonal correlation, although flare-ups are more common in winter months.
Similar to VKC, there is a male-to-female predominance (2:1 to 3:1), and AKC may also be associated with giant papillae and Trantas dots.2 Although there is a lot of overlap between VKC and AKC, one significant difference is that AKC most often occurs in adults aged 20 to 50 years and is not usually seen in adolescence.2
Ocular signs of AKC include conjunctival hyperemia, corneal neovascularization, and micropapillae typically located in the lower portion of the eye and eyelid. Symptoms include chronic irritation, ocular itching, and mucoid discharge with an almost exclusive history of eyelid dermatitis. A hallmark differentiation in the diagnosis of AKC is eyelid dermatitis, primarily eczematous, which can carry concomitant Staphylococcal aureus colonization and meibomian gland dysfunction.6
Because AKC is typically associated with chronic inflammation, patients with AKC may develop atopic cataracts that require extraction at a younger age.2
PATHOPHYSIOLOGY
AKC is thought to be a combination of immediate (type 1) and delayed (type 4) hypersensitivity to an ocular allergen exposure. Conjunctival epithelial cells and inflammatory cells infiltrate the ocular tissues that produce morphological changes including mucous metaplasia, conjunctival thickening, neovascularization, and scarring.6 Although precise pathophysiology of AKC has not been explained, the ocular inflammatory response is known to be present in those with predispositions to asthma, eczema, and atopic dermatitis.
TREATMENT
The goal of managing AKC is aimed toward controlling inflammation and symptoms. Comanagement with an allergist and dermatologist is encouraged. Acute stage treatment includes topical corticosteroids to both the ocular surface and periocular skin. Long-term management often includes calcineurin inhibitors like cyclosporine (off label) and tacrolimus to maintain remission.2
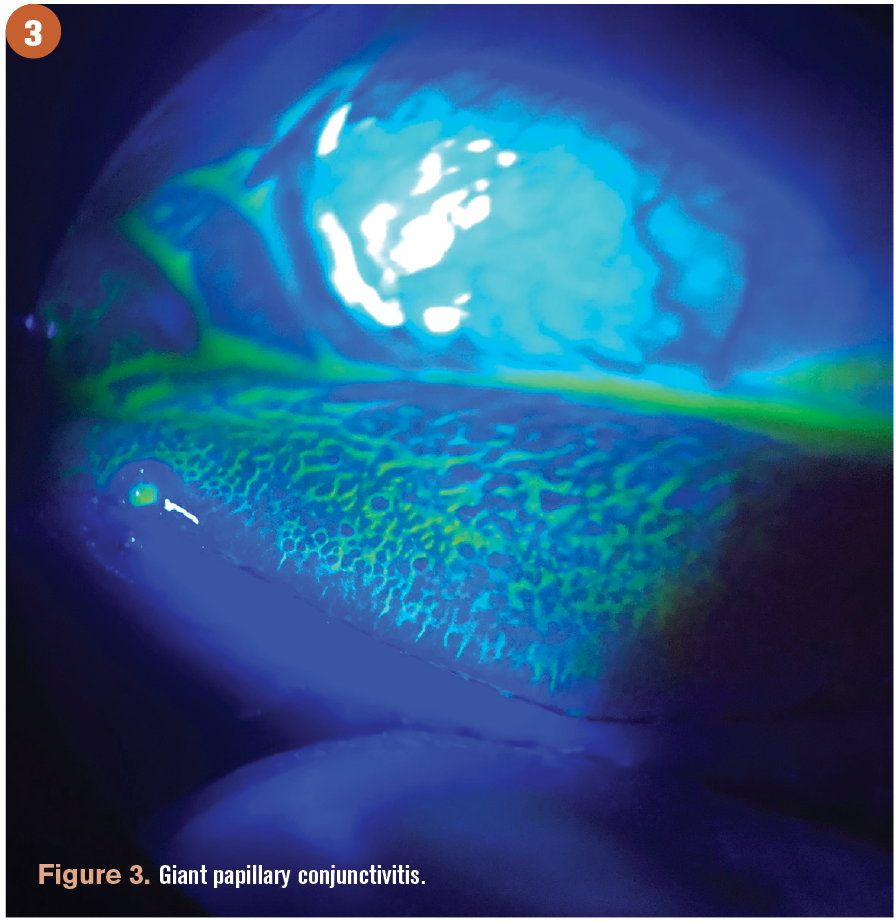
Giant papillary conjunctivitis
CLINICAL PRESENTATION
Giant papillary conjunctivitis (GPC) is not considered a “real” allergic disease but rather an inflammatory disease characterized by papillary hypertrophy of the superior tarsal conjunctiva.2 Although GPC is similar in appearance to VKC, there is typically no significant corneal involvement with GPC. Most often, the root cause of GPC is chronic ocular micro-trauma associated with contact lens wear, ocular prosthetics, limbal sutures, and limbal dermoids.2
PATHOPHYSIOLOGY
GPC is not an IgE-mediated allergy. Instead, it is a delayed (type 4) hypersensitivity and can involve the ocular surface, eyelids, and periocular skin.2 It is believed that protein build-up on contact lens surfaces contributes to irregular edges and mechanical trauma, which are both contributing factors to chronic inflammation associated with GPC. There is no evidence of an increase in IgE or histamine in the tears of patients with GPC.2
TREATMENT
GPC often resolves once the irritative stimuli is removed. For patients with a history of GPC who are still interested in wearing contact lenses, switching to a daily disposable lens may be beneficial.
Wrapping up
There are many different phenotypes of allergic eye disease with a wide range of characteristics. Knowing the clinical features of these different types of allergic conjunctivitis may prompt earlier diagnosis.
In addition, it is helpful to understand pathophysiology to determine the most effective treatment plan for a patient suffering from allergic conjunctivitis. Don’t forget to flip those lids.
REFERENCES
1. Allergy facts. American College of Allergy, Asthma, and Immunology. Updated January 9, 2018. Accessed February 16, 2021. http://acaai. org/news/facts-statistics/allergies
2. La Rosa M, Lionetti E, Reibaldi M, et al. Allergic conjunctivitis: a comprehensive review of the literature. Ital J Pediatr. 2013;39:18. doi:10.1186/1824-7288-39-18
3. Leonardi A, Bogacka E, Fauquert JL, et al. Ocular allergy: recognizing and diagnosing hypersensitivity disorders of the ocular surface. Allergy. 2012;67(11):1327-1337. doi:10.1111/ all.12009
4. Kraus, CL. Vernal keratoconjunctivitis. American Academy of Ophthalmology. April 28, 2016. Accessed February 16, 2021. https://www.aao. org/disease-review/vernal-keratoconjunctivitis-5
5. Leonardi A. Management of vernal keratoconjunctivitis. Ophthalmol Ther. 2013;2(2):73-88. doi:10.1007/s40123-013- 0019-y
6. Li A, Li S, Ruan F, Jie Y. Atopic keratoconjunctivitis: a diagnostic dilemma-a case report. Medicine (Baltimore). 2018;97(16):e0372. doi:10.1097/MD.0000000000010372