- Therapeutic Cataract & Refractive
- Lens Technology
- Glasses
- Ptosis
- Comprehensive Eye Exams
- AMD
- COVID-19
- DME
- Ocular Surface Disease
- Optic Relief
- Geographic Atrophy
- Cornea
- Conjunctivitis
- LASIK
- Myopia
- Presbyopia
- Allergy
- Nutrition
- Pediatrics
- Retina
- Cataract
- Contact Lenses
- Lid and Lash
- Dry Eye
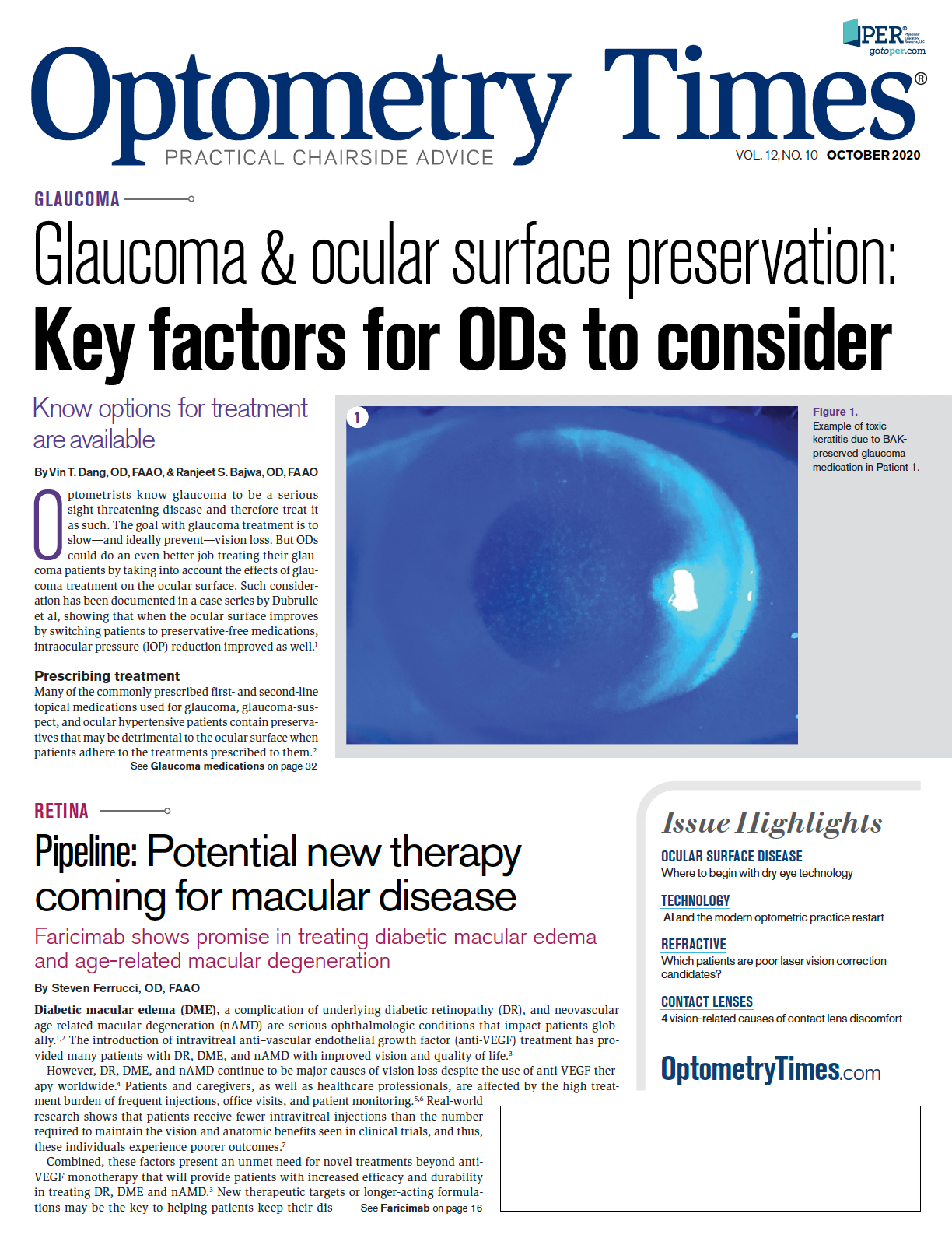
- Glaucoma
- Refractive Surgery
- Comanagement
- Blepharitis
- OCT
- Patient Care
- Diabetic Eye Disease
- Technology
Which patients are poor laser vision correction candidates?
LASIK deserves the hype, but it’s not for everyone
ODs should keep in mind the non-candidate list of patients who would experience dismal results with LASIK surgery. The plano presbyope, the young hyperope, the high hyperope and the under-25 myope all have one thing in common: LASIK is not for them.
Robert is a typical 48-year-old presbyope coming to your office because he is, in his words, “going blind.” All of us reading this have already, correctly, concluded he is a presbyope. Additionally, it is likely he has rarely been to an eye doctor and asks lengthy questions about each test you perform.
For such a simple patient, determining the best “solution” can be exhausting as there are many viable options, all with limitations. Therefore, it is most common to not mention the most unreasonable and least successful option, monovision laser in-situ keratomileusis (LASIK). Nevertheless, there are surgeons routinely treating Robert achieving dismal results, in part because no one told Robert, “LASIK is not for you.”
Related: When cataract outcomes are confounded by dry eye
Many of you are now chiming in, “The surgeon I use would never treat this type of patient,” and you are correct. Reputable LASIK surgeons are acutely aware of the 20/Happy goal and without it, either their practice or the practice of the referring doctor will suffer with the frustration of the unsatisfied patient.
Unfortunately, thousands of LASIK cases are performed each year where the most significant pre-operative test is the credit score. A surgeon who flies out is not impacted by the outcome of the patient. Below is a non-candidate list of patient types who could benefit from the quick mention of, “and if you are thinking of LASIK, don’t let anyone talk you into it without talking to me first.”
1.The plano presbyope
The plano presbyope is the patient I encounter most frequently. He is dissatisfied after LASIK, after about 2 years. To achieve a myopic refraction, you need to perform a hyperopic treatment. (I have seen careless surgeons program the “goal” manifest, resulting in +1.50 D refraction and a really unhappy patient but…).
Related: How the tear film affects IOL measurements
As ODs know, presbyopia progresses with age. Unfortunately, hyperopic treatments are far more likely to regress with time. A patient who needs a +1.50 D add at the time of surgery will need at least +1.75 D 2 years later and will have regressed at least 0.25 D. This leaves the patient with poor near vision and worse vision at distance than prior to surgery. This clinical course is common in all surgical monovision patients, but the most unhappy are those who started with good uncorrected distance vision. They often say things like, “If I would have known my distance would be so bad without any improvement in near, I would have never had the surgery.” Unfortunately, they are now your problem.
2.The young hyperope
The young hyperope is another type of patient who can be lured into the low-priced LASIK model. A 25-year-old +1.50 D hyperope may always wear her glasses or she may rarely wear glasses or contact lenses. Also, she might see 20/20 without any correction. Finally, she may cycloplege to +3.50 D.
As you can see, there is a lot going on with this “simple” patient. When the +1.50 D hyperope, who sees 20/20 uncorrected, has LASIK, she is rarely happy. How much better could the uncorrected visual acuity (UCVA) get?
Furthermore, hyperopes often have a large angle kappa—if the treatment is not properly centered, the quality of vision can be significantly reduced even when high contrast acuity is 20/20. This type of patient may do very well with laser vision correction, but it requires a thoughtful evaluation of the patient’s visual system along with the appropriate consultation. For these patients I would always mention, “and if you are thinking of LASIK, don’t let anyone talk you into it without talking to me first.”
More by Dr. Owen: How to differentiate CTK from DLK in post-surgical patients
3.The high hyperope
The high hyperope is a challenge for every eyecare modality. The glasses are thick and magnify the eyes. Contact lenses are thicker in the center, transmitting less oxygen which may create corneal health challenges, not to mention instability in trying to handle the lens. High hyperopes’ anterior chambers are usually shallow, which is why there is not an approved implantable contact lens for these patients. So too, with laser vision correction, I have found that the results are mediocre, at best. Even if the laser is approved up to +6.00 D, that doesn’t mean you should treat that much hyperopia. We have learned over the years that the cornea will get only so steep. Each surgeon has their own cut off, but they range from 47.00 D to 49.00 D.
There is a one-to-one relationship between refractive error and steepening of the cornea. For example, a +4.00 D patient with a 45.00 D cornea will end up with a 49.00 D cornea. Those who will operate on anyone often use the phrase: “Well, at least we can make the glasses thinner. The dilemma with this thinking is the patient’s quality of vision is often poor due to the shrunken optic zone and displaced apex to the cornea.
Also, the trough in the peripheral cornea can be filled in with a hypertrophy of epithelium leading to a reduced effect of the surgery. This gets further complicated when the surgeon wants to do a photorefractive keratectomy (PRK) enhancement 2 years down the road. The epithelium is removed, leaving a stroma, which is the correct curvature. After the PRK, the patient can be as much as 2.00 D myopic until the hypertrophy returns. This process can take up to a year. Your patients above +4.00 D or so are a challenge. Do them this favor: Mention, “and if you are thinking of LASIK, don’t let anyone talk you into it without talking to me first.”
More by Dr. Owen: Laser vision correction: Look backward to move forward
4.The under-25 myope
This last type of patient might seem the least “at risk,” but I have experienced too many ectasia cases with this type of patient to not review the concerns. This patient is the under 25-year-old myope who has a relatively mild myopic correction—specifically, the patient who is coming to you for the first time. It is not uncommon for this patient to not have an established eye doctor because he is done with college in one town and now working in a third town that is not where he grew up. While it is common to think of the “at-risk” corneas having high refractive errors and/ or thin corneas, that is not always the case. The metrics analyzed by the Belin-Ambrosio Display on the Pentacam (Oculus) seem to be more sensitive and specific for at risk corneas.1
In my opinion, a Pentacam is necessary in 2020 for laser vision correction, but interpretation of its results requires skill and experience that can be lacking in many LASIK centers. Having this patient establish stability with your practice, and if stable, referring him to a practice that has expertise in Pentacam interpretation will greatly reduce their risk of ectasia. Seeing the patient back in a year can make a meaningful difference in the success for his LASIK procedure.
In 2020, laser vision correction is a remarkable procedure that greatly benefits many patients. Unfortunately, there are surgeons who will operate on anyone. I have outlined a small group of patients who, in general, do not do well with laser vision correction. These types of patients are likely obvious to most ODs. By letting these patients know that they are not ideal candidates, you are doing them a huge favor and likely helping yourself avoid the agony of caring for them later.
REFERENCE
1. Duncan JK, et al. Assessing progression of keratoconus: novel tomographic determinants. Eye Vis (Lond). 2016 Mar 11;3:6.