3 tips to better fit keratocones with sclerals
You may have heard success stories with patients fit in scleral lenses and seen discussion in literature regarding the finer points of fitting these contact lenses. If you are not currently fitting scleral contact lenses but are interested in working with them, we recommend three things to prepare yourself and your practice to fit scleral lenses.
The views expressed here belong to the author. They do not necessarily represent the views of Optometry Times or UBM Medica.
Keratoconus is one of the more challenging yet more rewarding conditions that we treat in our offices. Individuals with keratoconus have a thinning of their corneas that causes a protrusion and irregular steepening. This creates an irregular surface that inappropriately focuses light on the retina even with the best refractive correction.
Although corneal crosslinking is a treatment to prevent progression, often these individuals will still be left with irregular astigmatism that needs to be corrected.
Starting points of treatment
In milder cases of keratoconus, simply correcting the refractive error with a standard soft toric contact lens may correct vision to levels that are adequate for the patient. Standard soft contact lenses are often prism ballasted and thus have a thicker profile than a standard spherical lens.
Previously from Dr. Brujic and Dr. Kading:
Soft contact lenses help improve some of these patients’ vision better than what can be obtained through a standard spectacle lens. As keratoconus progresses, there are other options to correct vision. Soft contact lenses specifically designed to correct keratoconus and the higher order aberrations associated with them are available in both hydrogel and silicone hydrogel options.
When a soft contact lens doesn't improve vision to adequate levels, we consider a corneal gas permeable (GP) contact lens. Theses lenses create a more regular surface by masking many of the irregularities that the keratoconic cornea naturally contains.
Because of their small diameter, GP lenses are relatively easy to place on the eye-even for neophyte wearers. Additionally, there is adequate tear exchange for appropriate corneal support with corneal GP lenses, but there may be initial lens awareness.
Contemporary corneal GP lenses, which are slightly larger than traditional corneal GP lenses, have helped alleviate initial symptoms of keratoconus. Hybrid lenses with a gas permeable center and scleral lenses can introduce GP optics without the initial awareness associated with corneal GP lenses.
Related:
Hybrid lenses now have designs that are specifically made for keratoconus patients. They have a central GP material that has a high Dk and a soft skirt that is created out of silicone hydrogel material.
Scleral lenses may be the answer
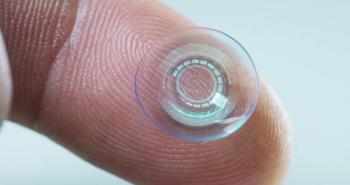
Scleral lenses and improved designs and materials have changed the way that keratoconus is managed. Scleral lenses, as their name implies, are fit so that the lens rests on the conjunctiva and underlying sclera. Although we categorize this as a contact lens, the scleral lens never actually touches the cornea when fit appropriately.
You may have heard success stories with patients fit in scleral lenses and seen discussion in literature regarding the finer points of fitting these contact lenses. If you are not currently fitting scleral contact lenses but are interested in working with them, we recommend three things to prepare yourself and your practice to fit scleral lenses.
1. Educate yourself on the lenses and the fitting process
Scleral lenses follow a completely different fitting philosophy compared to standard soft or even corneal GP lenses. Normally, we discuss the parameters of contact lenses in terms of the diameter and base curve. Scleral lenses are different and change the fitting philosophy because a scleral lens is based on appropriate clearance of the lens over the cornea.
Instead of discussing base curve to modify the lens parameters, we discuss sagittal depth. Sagittal depth describes the depth of the bowl of the lens. Manipulating the sagittal depth will have direct consequences on the level of clearance the lens has over the cornea.
In most cases, both soft and corneal GP lenses can be placed by using a single finger to place the lens on the eye. Although it is important for these lenses to settle appropriately on the eye, it is not critical that the lens is placed on the eye in the exact position that it needs to be.
With scleral lenses, the bowl of the lens needs to be filled with a preservative-free solution. It is critical that these lenses maintain much of the fluid in the bowl when placed on the eye. It is difficult to place the lens with one finger, so often times this is done by balancing the lens on either two or three fingers.
Additionally, specialized tools such as large DMV lens removal devices or scleral lens insertion rings are available to help patients with the insertion process. Because the lenses are filled with fluid, patients’ heads need to be as close to horizontal as possible to avoid spilling the fluid. Patients need to look directly into the lens as they apply it because the lens needs to be placed directly on the cornea.
Related:
Scleral lenses are so fundamentally different that it is important to learn as much as you can about them. There are a number of resources available to increase your knowledge.
Two websites to consider are:
Additionally, a guide to fitting scleral lenses is available at
All of these resources are available to practitioners at no cost.
You will also need practical experience placing these lenses on patients’ eyes and assessing the fits at the slit lamp. A number of workshops that provide practical experiences for ODs are available across the country. We recommend ODs attend and get practical experience at these workshops.
Also key in the fitting process is understanding how to position the fitting of scleral lenses, and more important, specialty lenses in your practice. This includes how to schedule patients, setting appropriate expectations, knowing what to look for at follow-up visits, and appropriately billing and coding the lenses and the fitting process involved.
2. Purchase a fitting set
This will be critical. Scleral lenses are not empirically ordered based on refraction and keratometry readings. The lenses have to be physically placed on the eye in order to maximize the fitting characteristics of the lens.
Related:
Many lenses may be placed on and off of the patient’s eye before the appropriate fit is determined. The prescription is determined by performing an over-refraction with the lens on the eye once the appropriate fit is achieved. The resultant prescription in the lens that you order for the patient may not be related to the patient’s prescription.
3. Have a mentor
This is essential because as you start the fitting process, a number of questions will arise. Although consultants at the lab that you use will be able to help you with many questions, it is critical to have a colleague to call. A close colleague will be able to help with questions on the practical aspects of fitting scleral lenses once you start the process in your practice.
Fitting scleral lenses can change lives. Although we discussed them specifically with respect to keratoconus, they can also be used with other corneal ectasias, corneas that are scarred, severe ocular surface disease, and patients require more stability with their vision-specifically those with high corneal astigmatism.
Scleral lenses are different than traditional corneal lenses, but they are rewarding to fit for both patients and practitioners. When it comes to fitting specialty lenses, we think that when it is appropriate, you should go big or go home!
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.