4 steps to beating blepharitis
Blepharitis is an inflammatory condition of the eyelids leading to red, irritated, itchy, and dandruff-like scales that form on the eyelashes.
is an inflammatory condition of the eyelids leading to red, irritated, itchy, and dandruff-like scales that form on the eyelashes. It is a common eye disorder caused by bacteria or a skin condition, such as dandruff of the scalp or acne rosacea.1 No matter the cause, the only way we can beat blepharitis is to determine the location as anterior, posterior, or mixed; differentiate among the causative factors, and treat according to the severity of the condition.
Step 1
Differentiate and understand presentation differences
The first step in addressing blepharitis is to differentiate and understand the differences among the presentations. The term “blepharitis” has been commonly referred to as a single disease state; however, there are multiple presentations which are not the same at all. To complicate things further, there is inconsistency in terminology in addition to challenges related to overlap with other ocular surface diseases such as dry eye disease and allergic conjunctivitis. All three may present with similar signs and symptoms which, if not properly identified, will not be optimally treated.
Related: Understanding and defining MGD
Anterior blepharitis is an inflammation of the eyelid margin anterior to the gray line and concentrated around the lashes.2 The condition is typically associated with gram-positive bacteria, most commonly staphylococcal infections (Staphylococcus aureus and Staphylococcus epidermis).
Other causes include dry eye disease, Demodex mite infestations, rosacea, seborrheic dermatitis, isotretinoin, and giant papillary conjunctivitis.3 Typical clinical findings include debris or collarettes at the base of the eyelashes, erythema, and edema of the lid margin. Symptoms and presentation can be acute or chronic.
The most common forms of anterior blepharitis:
• Staphyloccal blepharitis frequently exhibits mildly sticky eyelids, thickened lid margins, and missing/misdirected eyelashes. This presentation also includes the hallmark signs of lid swelling-erythema of the lid margins, scaly collarettes at the base of the lashes, and possible skin ulceration.
The three possible mechanisms underlying staphylococcal blepharitis include direct bacterial infection, a reaction to bacterial exotoxins, or a cell-mediated hypersensitivity response to bacterial antigens.
• Seborrheic blepharitis presents with foamy, greasy flakes or scales around the base of eyelashes and a mild redness of the eyelids. It is part of a dermatologic condition that includes the scalp, face, and eyebrows (seborrheic dermatitis) and may be associated with rosacea and acne vulgaris.1
Related: Incorporating meibomian gland imaging
• Ulcerative blepharitis presents with matted, hard crusts around the eyelashes. Eyelash loss, distortion of the front edges of the eyelids, and chronic tearing are frequently associated.4
• Demodex blepharitis is an inflammatory reaction to a common mite that inhabits the eyelash follicles. Demodex mites are the most common microscopic ectoparasite found in the human skin. Classic symptoms include itching, burning, foreign body sensation, crusting and redness of the lid margin, and blurry vision.
In addition to cylindrical dandruff found in Demodex blepharitis, persistent infestation of the lash follicles may lead to malalignment, trichiasis or madarosis.5
Posterior blepharitis, or meibomian gland disease, is an inflammation of the posterior lid margin, which can have different causes, including meibomian gland dysfunction (MGD), infectious and allergic conjunctivitis, and acne rosacea.2 Recent literature has used the terms “posterior blepharitis” and “MGD” as if they were synonymous, but these terms are not interchangeable.6-11
According to the International Workshop on Meibomian Gland Dysfunction (MGD), the condition is a chronic, diffuse abnormality of the meibomian glands, commonly characterized by terminal duct obstruction, and qualitative and quantitative changes in the glandular secretion. Meibomian gland dysfunction may result in alterations of the tear film, symptoms of eye irritation, clinically apparent inflammation, and ocular surface disease.12
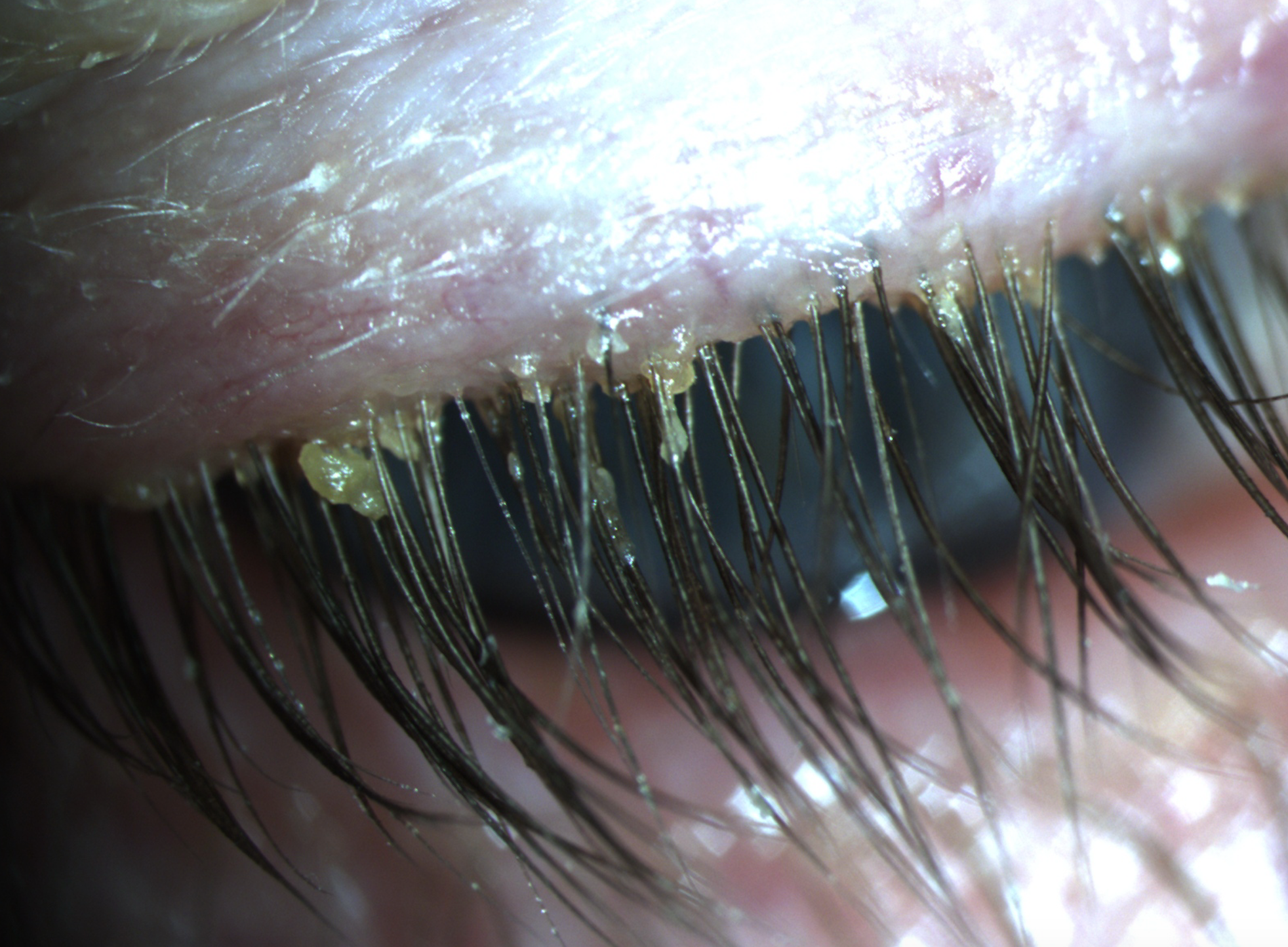
Anterior blepharitis associated with Demodex. Image courtesy of Scott G. Hauswirth, OD, FAAO
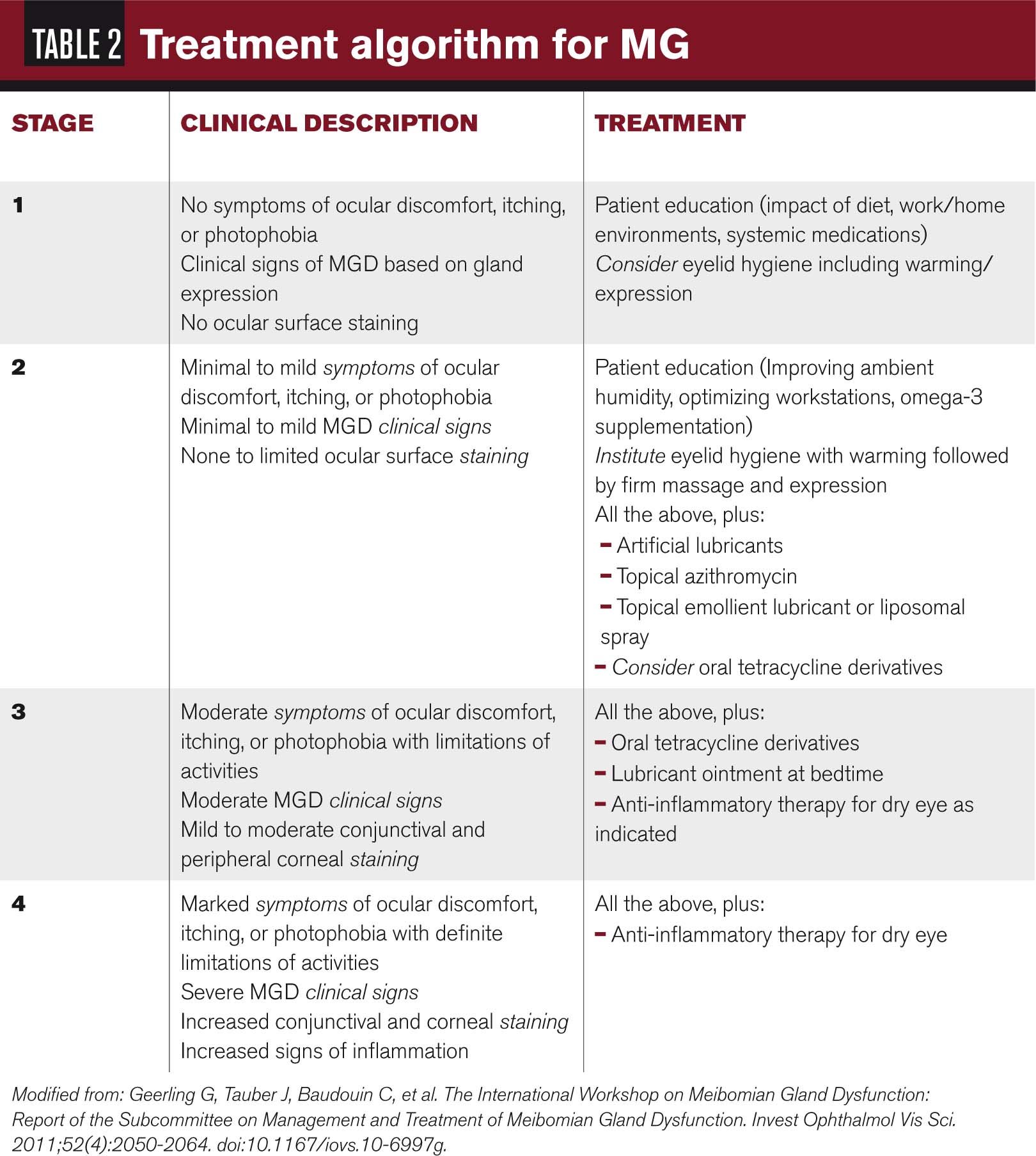
Patients may be asymptomatic or symptomatic and may present clinically or subclinically. The diagnosis is made via the number of meibomian gland expression, quality of meibomian gland secretion, and loss of gland structure and function.
As the disease progresses, symptoms develop and lid margin signs may include inspissated meibomian glands, telangiectasia, and thickened eyelid margins. At this point, an MGD-related posterior blepharitis is said to be present.2 The end result is a decrease in the quality of the lipid layer of the tear film resulting in evaporative dry eye disease.
Related: 5 ways to go beyond baby shampoo for lid hygiene
With so many presentations of blepharitis, there is a need to identify and classify the condition to allow for a clinically straightforward diagnostic and treatment algorithm.
Step 2
Understand the prevalence and who is affected
The second step in addressing blepharitis is to appreciate why it matters and who is affected. As optometrists, we are judged by the ocular comfort and quality of vision for our patients. We understand that ocular surface disease, including dry eye disease, ocular allergy, and both anterior and posterior blepharitis, plays a role. So the question remains, who gets blepharitis?
Related: How MGD can work for your practice
According to a 2009 survey, ophthalmologists and optometrists reported that 37 percent and 47 percent of patients, respectively, present with some form of blepharitis whether symptomatic or asymptomatic.13,14 MGD (may be a form of posterior blepharitis) is considered to be the most common cause of evaporative dry eye disease.13,14
Despite its prevalence, blepharitis is still often overlooked, misdiagnosed, and therefore suboptimally treated, which is why it is so important for practitioners to be cognizant of the condition.
According to Venturino et al, in patients seeking an eye examination because of ocular discomfort or irritation, the prevalence of posterior blepharitis was 24 percent, dry eye disease 21 percent, and anterior blepharitis 12 percent.15
Nonetheless, symptomatic patients are typically the easiest to identify and treat with available treatment options.
The key to Step Two is to understand the high prevalence of this condition and to identify patient whether asymptomatic or symptomatic.
Step 3
Listen to patient complaints and look for the disease
The third step in blepharitis management is listening to our patients’ complaints and looking for the disease-even if they do not present with symptoms. Whether patients present for a routine evaluation, contact lens fitting, surgical evaluation, or something else, a thorough evaluation of the lids and the ocular surface must be performed in order to promote and address the ocular health and surface.
Blurred and fluctuating vision can affect all of our patients and can lead to remakes of glasses.
Contact lens wearers want to be able to wear their lenses comfortably throughout the day, and all forms of blepharitis can lead to contact lens dropouts due to this discomfort. Blepharitis can also lead to the increased risk of ocular infections and inflammatory conditions such as contact lens-related red eye, marginal keratitis, and corneal ulcers.
Related: What’s all the craze about demodex?
What about our surgical patients? With the rise of our cataract population, we need to be concerned about the increase risk of endophthalmitis due to bacteria on the lid flora. According to the Endophthalmitis Vitrectomy Study, 70 percent of isolates were gram-positive, coagulase-negative organisms (primarily Staphylococcus epidermidis), 24 percent were other gram-positive organisms, and 6 percent were gram-negative organisms.16
A diagnostic algorithm for all forms of blepharitis includes a comprehensive eye evaluation and thorough history. Age and associated skin disorders (dermatitis, rosacea, and acne vulgaris) must be considered.
For anterior blepharitis, listening for symptoms of morning lid stickiness or crusting, burning, and acute/chronic may be clues to the diagnosis as well as the signs of lid erythema, edema, and debris. For MGD and posterior blepharitis, symptoms will include burning, stinging, and fluctuating vision due to a poor lipid layer of the tears.
Signs can be identified with meiboscopy (transilluminator), meibography (Lipiview II, TearScience) and diagnostic manual expression, using a Q-tip, fingertip, or Meibomian Gland Evaluator (TearScience), which will identify the number of secreting glands and the quality of secretions.
For chronic conditions, cultures of the eyelid margin may be indicated for patients who have recurrent anterior blepharitis or who are not responding to therapy. Another consideration is microscopic evaluation of epilated eyelashes may reveal Demodex mites, which have been implicated in some cases of chronic blepharoconjunctivitis.3
Prior to initiating treatment, providers must remember that both conditions may present concurrently; however, once correctly identified, treatment can be instituted. We must remember that we can’t find it if we aren’t looking for it.
Step 4
Treat and manage accordingly
Goals for the treatment and management of all forms of blepharitis include reducing the symptoms and signs, minimizing structural damage, and preventing loss of visual function.3 To accomplish these goals, providers must identify the condition, determine the severity, and treat accordingly. Patient education is key to treatment for any ocular or medical condition, including blepharitis. Patients must understand that this is their condition and there is no cure; however, we are going to help them manage it.17 Warm compress, eyelid hygiene, nutraceuticals, topical/oral antibiotics, and topical anti-inflammatories have been the traditional mainstay of treatment. Showing patients how to properly use each treatment will help with compliance and adherence.

Basic treatment
The most basic treatment regimen for all forms of blepharitis utilize a combination of warm compresses, lid scrubs, and nutraceuticals.18
For both anterior and posterior blepharitis, warm compresses are used to promote meibomian gland secretion and loosen eyelid scurf prior to lid hygiene.
Eyelid scrubs, which include diluted baby shampoo or detergent-based products, are now available in foam surfactant cleansers (such as Ocusoft Foam Plus or TheraTears Sterilid), which effectively remove debris and excessive oils from the lid margin.
In the last several years, hypochlorous acid (HOCl)has been become a popular treatment for blepharitis. HOCl prescription (Adenova, NovaBay) and non-prescription (HypoChlor, OcuSoft) eyelid cleaners incorporate 0.01% and 0.02% HOCl, respectively, which is found in our innate immune system.19 HOCl is produced by our bodies’ neutrophils, which can help kill bacteria, block bacterial derived toxins, and slow the effects of human cell-derived pro-inflammatory mediators.20,21
For patients who present with demodex blepharitis, tea tree oil has become the mainstay of treatment. Cliradex (BioTissue) lid wipes have become the primary treatment for patients with Demodex blepharitis.
The active ingredient, 4-terpineol from tea tree oil, has been identified as the most potent demodicidal element.22 It is generally prescribed twice daily for several weeks, then at bedtime in order to maintain coverage throughout the life cycle of the mite.
Topical/oral antibiotics and anti-inflammatories
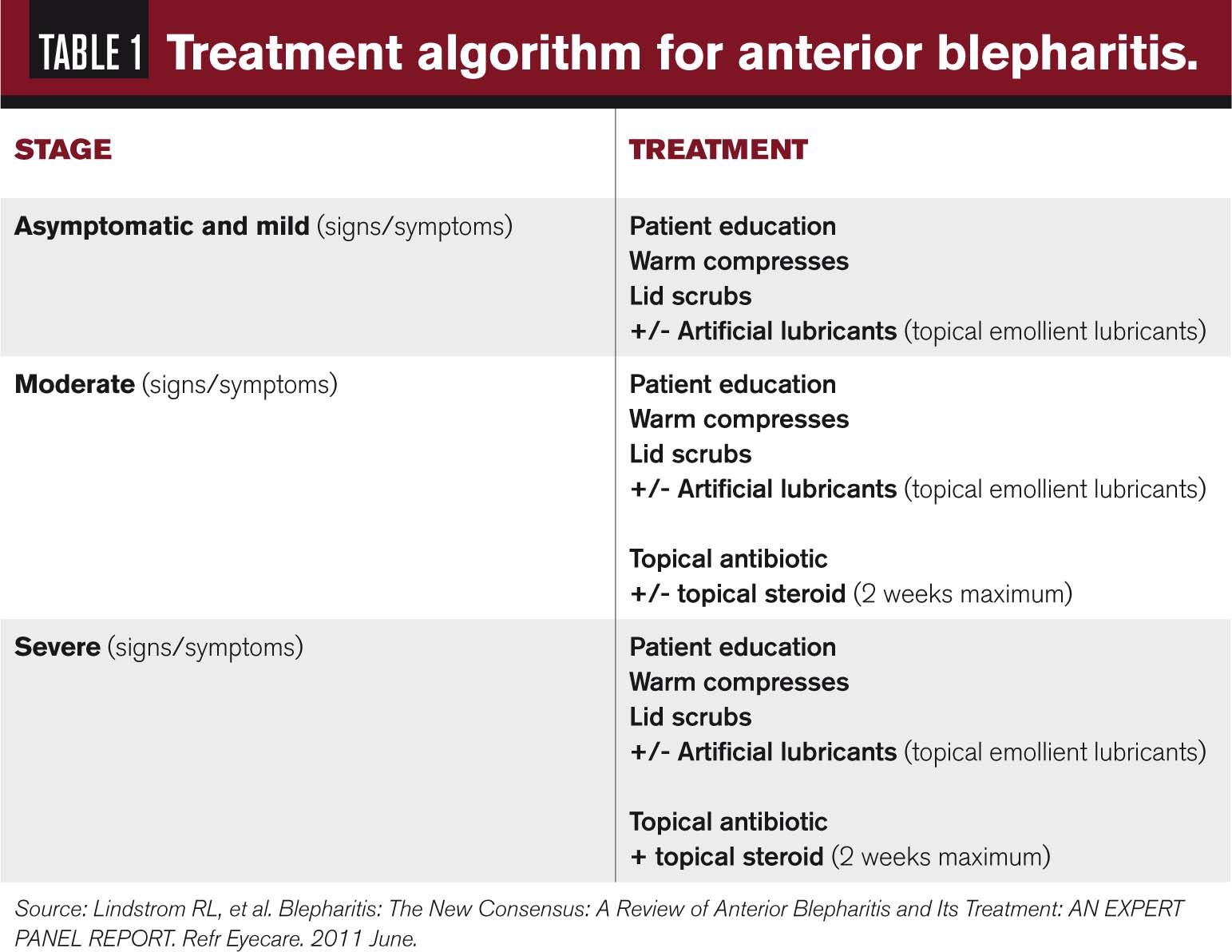
The severity of the condition and the presence of inflammation will determine the utilization of antibiotics and anti-inflammatories (see Table 1). Most current topical antibiotics are not sufficient for the treatment of blepharitis because of the inability to penetrate and remain active in the lid tissues.
Related: How ODs can do better with dry eye
Erythromycin ointment is a cost-effective option which provides both antibacterial coverage as well as anti-inflammatory effects. It can also be beneficial for patients who suffer from concurrent nocturnal lagophthalmos.
Azithromycin 1% ophthalmic solution (AzaSite, Akorn Pharmaceuticals) has been shown to be antimicrobial to the most common eyelid bacteria as well as address inflammation by inhibiting pro-inflammatory cytokines and matrix metalloproteinases (MMPs).
In several studies, AzaSite has shown improved bioavailability in the target tissues without continuous dosing, which is significant in the treatment of this chronic blepharitis. AzaSite is applied by rubbing or massaging the medication onto the lid margins one to two times daily. 23,24
For patients with moderate-to-severe or unresponsive posterior blepharitis, oral antibiotics such as tetracycline derivatives should be considered. Tetracyclines are believed to disrupt the production of bacterial lipases and have potent anti-inflammatory agents.25,26 Doxycycline is prescribed from 20 mg to 100 mg once or twice daily depending on the severity of the condition and duration of treatment. As a reminder, the tetracycline class should be taken on an empty stomach and should not be given to pregnant women or children under the age of 8.
In the presence of corneal or conjunctival inflammation, providers can use short-term corticosteroid-antibiotic combinations such as tobramycin 0.3%/dexamethasone 0.05% ophthalmic suspension (Tobradex ST, Alcon) and loteprednol etabonate 0.5%/tobramycin 0.3% ophthalmic suspension (Zylet, Bausch + Lomb).27 These options allow us to address inflammation while reducing the bacterial load on the ocular surface.
However, as with any corticosteroid treatment, we must be cautious of the effects of long-term use. Due to the concurrent nature of blepharitis and dry eye, cyclosporine 0.5% (Restasis, Allergan) can be used to treat inflammation, especially for posterior blepharitis, meibomitis, or chronic rosacea.28
There have been multiple innovations in blepharitis treatment which has helped manage patients’ chronic condition. Devices such as BlephEx (Rysurg), Lipiflow (Tear Science), and Mibo Thermoflo (Mibo Medical Group) have improved our ability to fully address the underlying causes of blepharitis for both anterior and posterior blepharitis.
In our experience, we utilize a combination of treatments to reduce the bacteria load and biofilms while improving MG secretions and symptoms scores.
Related: Why you’re missing the dry eye right in front of you
BlephEx is an in-office tool that allows an eye care provider to safely microblepharoexoliate, or deep clean, the eyelid margin and the base of the eyelashes. It is a painless procedure that can be performed by an optometrist or technician to clean both the anterior and posterior lid margins. In addition to mechanical debridement, the cleaning agent used for the procedure will help kill bacteria. This procedure effectively removes bacteria, biofilm, and debris from the patient’s eyelids.
TearScience’s LipiFlow is a thermal pulsation treatment that combines heat with physical massage to liquefy and express the meibomian gland contents. LipiFlow is a 12-minute procedure that is FDA-approved to restore gland function in patients with meibomian gland dysfunction. The device consists of activators that are placed beneath the eyelids and vault over the globe. T
he activator produces heat, up to 109° F, outward to the glands while utilizing rubber pads that apply pulsatile pressure to the eyelids to remove gland obstructions and express contents of the glands. In a three-year study, meibomian gland secretion scores and the Standard Patient Evaluation of Eye Dryness (SPEED) scores showed improvement continued at three years.
Tear film break-up time (TBUT) and the average Ocular Surface Disease Index (OSDI) score both showed improvement at one month but were no longer statistically significant at one year and two years, respectively.29
Intense pulsed light Therapy (IPL) is a laser treatment designed to heat the meibomian glands in patients with MGD and evaporative dry eye disease. Originally used to treat conditions such as rosacea, sun damage, and hair removal, IPL is now used to direct high intensity bursts of light along the lower eyelids and upper cheek to liquefy the hardened secretions that plug the meibomian glands.30 IPL closes irregular blood vessels to reduce telangiectasia of the eyelids.
Take steps for accurate diagnosis
With up to 50 percent of our patients presenting with some form of blepharitis, it is important that we take a step-by-step approach to accurately diagnose blepharitis, educate and address our patients’ complaints, and treat and manage accordingly. This process includes identifying our asymptomatic patients and those who do not associate their symptoms with blepharitis. At that point, we can utilize our treatment algorithms based on the severity of the condition, in conjunction with newer innovative procedures, to truly beat blepharitis.
Related: Shire gets FDA nod for Xiidra (lifitegrast) for dry eye
References
1. AOA Optometric Clinical Practice Guidelines. Care of the Patient with Ocular Surface Disorders Available at:. http://www.aoa.org/documents/optometrists/CPG-10.pdf. Accessed 06/14/16.
2. Nelson JD, Shimazaki J, Benitez-del-Castillo JM, et al. The International Workshop on Meibomian Gland Dysfunction: Report of the Definition and Classification Subcommittee. Invest Ophthalmol Vis Sci. 2011 Mar 30;52(4):1930-7.
3. American Academy of Ophthalmology Cornea/External Disease PPP Panel, Hoskins Center for Quality Eye Care. Blepharitis PPP – 2013. Available at: http://www.aao.org/preferred-practice-pattern/blepharitis-ppp--2013#references. Accessed 06/18/16.
4. American Optometric Association. Blepharitis. Available at: http://www.aoa.org/patients-and-public/eye-and-vision-problems/glossary-of-eye-and-vision-conditions/blepharitis?sso=y. Accessed 06/17/16.
5. Liu J, Sheha H, Tseng SCG. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010 Oct;10(5):505-10..
6. Gutgesell VJ, Stern GA, Hood CI . Histopathology of meibomian gland dysfunction. Am J Ophthalmol. 1982 Sep;94(3):383–387.
7. Keith CG . Seborrheic blepharo-kerato-conjunctivitis. Trans Ophthalmol Soc UK. 1967;87:85–103.
8. McCulley JP, Dougherty JM, Deneau DG . Classification of chronic blepharitis. Ophthalmology. 1982 Oct;89(10):1173-80.
9. Luchs J. Efficacy of topical azithromycin ophthalmic solution 1% in the treatment of posterior blepharitis. Adv Ther. 2008 Sep;25(9):858-70.
10. McCulley JP, Sciallis GF . Meibomian keratoconjunctivitis. Am J Ophthalmol. 1977 Dec;84(6):788-93.
11. Mathers W. Meibomian gland disease. In: Pflugfelder S Beuerman R Stern M eds. Dry Eye and Ocular Surface Disorders. New York: Marcel Dekker, Inc.; 2004:255.
12. Nichols KK, Foulks GN, Bron AJ, et al. The international workshop on meibomian gland dysfunction: executive summary. Invest Ophthalmol Vis Sci. 2011 Mar 30;52(4):1922-9.
13. Lemp MA, Nichols KK. Blepharitis in the United States 2009: A survey-based perspective on prevalence and treatment. Ocul Surf. 2009 Apr;7(2 Suppl):S1-S14.
14. Donnenfeld ED, Mah FS, MacDonald MB. New considerations in the treatment of anterior and posterior blepharitis. Refract Eye Care. 2008;12(4 Suppl.):3-14.
15. Venturino G, Bricola G, Bagnis A, Traverso CE. Chronic Blepharitis; Treatment Patterns and Prevalence. Invest Ophthalmol Vis Sci. 2003;44(13):774.
16. Han DP, Wisniewski SR, Wilson LA, et al. Spectrum and susceptibilities of microbiologic isolates in the Endophthalmitis Vitrectomy Study. Am J Ophthalmol. 1996 Jul;122(1):1-17.
17. Lindsley K, Matsumura S, Hatef E, Akpek EK. Interventions for chronic blepharitis. Cochrane Database Syst Rev. 2012; 5: CD005556.
18. Macsai MS. The Role of Omega-3 Dietary Supplementation in Blepharitis and Meibomian Gland Dysfunction (An AOS Thesis). Transactions of the American Ophthalmological Society. 2008;106:336-356.
19. Wang L, Bassiri, Najafi R, et al. Hypochlorous acid as a potential wound care agent: part I. Stabilized hypochlorous acid: a component of the inorganic armamentarium of innate immunity. J Burns Wounds. 2007;6:e5.
20. Gray MJ, Wholey WY, Jakob U. Bacterial responses to reactive chlorine species. Annu Rev Microbiol. 2013;67:141-60.
21. Ono T, Yamashita K, Murayama T, Sato T. Microbicidal effect of weak acid hypochlorous solution on various microorganisms. Biocontrol Sci. 2012;17(3):129-33.
22. Tighe S, Gao YY, Tseng SC. Terpinen-4-ol is the most active ingredient of tea tree oil to kill Demodex mites. Transl Vis Sci Technol. 2013 Nov;2(7):2.
23. Abelson M, Protzko E, Shapiro A, et al. A randomized trial assessing the clinical efficacy and microbial eradication of 1% azithromycin ophthalmic solution vs tobramycin in adult and pediatric subjects with bacterial conjunctivitis. Clin Ophthalmol. 2007 Jun;1(2):177-82.
24. Ianaro A, Ialenti A, Maffia P, et al. Anti-inflammatory activity of macrolide antibiotics. J Pharmacol Exper Ther. 2000 Jan;292(1):156-163.
25. Dougherty JM, McCulley JP, Silvany RE, Meyer DR. The role of tetracycline in chronic blepharitis. Inhibition of lipase production in staphylococci. Invest Ophthal Vis Sci. 1991 Oct;32(11):2970-5.
26. Stone DU, Chodosh J. Oral tetracyclines for ocular rosacea: An evidence based review of the literature. Cornea. 2004 Jan;23(1):106-9.
27. Jackson WB. Blepharitis: current strategies for diagnosis and management. Can J Ophthalmol. 2008 Apr;43(2):170-9.
28. Rubin M, Rao SN. Efficacy of topical cyclosporin 0.05% in the treatment of posterior blepharitis. J Ocul Pharmacol Ther. 2006 Feb;22(1):47-53.
29. Greiner JV. Long-term (3 year) effects of a single thermal pulsation system treatment on meibomian gland function and dry-eye symptoms. Eye Contact Lens. 2016 Mar;42(2):99-107.
30. Barbarino SC. A variety of cosmetic procedures available. Advanced Ocular Care. 2015. Jul/Aug 2015. Available at: http://eyetubeod.com/2015/08/a-variety-of-cosmetic-procedures-available. Accessed 06/19/16.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.