5 things you don’t know about punctal plugs
How often are you using punctal plugs in your practice? If your answer is similar to mine, it’s “not as often as I used to.” Classically, punctal plugs were a go-to treatment for dry eye patients. If artificial tears failed to yield relief, plugs were a logical next choice.
How often are you using punctal plugs in your practice? If your answer is similar to mine, it’s “not as often as I used to.” Classically, punctal plugs were a go-to treatment for dry eye patients. If artificial tears failed to yield relief, plugs were a logical next choice. When research began to support a significantly higher prevalence of evaporative dry eye disease compared to aqueous deficiency, punctal plugs fell by the wayside in many practices. However, plugs continue to be a reliable treatment for the right patient at the right time.
1. Choose wisely: Accurate diagnosis
Accurately diagnosing dry eye disease begins with a thorough case history. Typically, doctors and patients alike focus on the frequency and onset of symptoms. Blur, foreign body sensation, and photosensitivity affect the patient’s ability to work comfortably, drive safely, and enjoy life. However, a complete history of a dry eye disease patient must go beyond how the patient feels. A full medical history is required to establish the root of the patient’s complaint and may point toward a specific tear film deficiency. Medications, systemic disease, and surgical history are key to providing the whole picture.
More from Dr. Hauser: MGD: Identification and treatment
Punctal plugs can provide significant relief to the patient with decreased lacrimation. Diagnostic testing is essential to differentiate aqueous deficient dry eye disease (ADDE) from evaporative dry eye disease (EDE). Schirmer’s strip testing is the most common method of evaluating aqueous production. However, the more than 100-year-old test is not without problems. It offers low specificity, sensitivity, and reproducibility. Additionally, patients who often present with pain as a complaint find that Schirmer’s strips add insult to injury. Phenol red thread (PRT) testing is emerging as an alternative to conventional Schirmer’s strips. PRT uses a thread inserted at the temporal conjunctival sac of an anaesthetized eye. The pH of the tears changes the thread from yellow to red and indicates tear volume. While reported to be more sensitive and comfortable for patients, the jury is still out on exactly what PRT measures.1
While Schirmer’s testing and PRT validate the ADDE diagnosis, it is equally informative to rule out an EDE component. Performing meibography and lipid layer thickness analysis help determine if there is a mixed mechanism to the patient’s dry eye disease. Once a diagnosis of ADDE has been made, proceeding with punctal plugs is a reasonable course if the patient failed to resolve with less invasive treatments.
Related: When cataract outcomes are confounded by dry eye
2. Take the risk out of Risky Business
The risks associated with punctal plugs are generally very low and easily managed. Foreign body sensation (FBS) or irritation after insertion is the most common complaint (60 percent of all reported).2 If the patient has a feeling of awareness vs. FBS, consider encouraging a re-assessment after 24 hours. If awareness persists or the complaint mirrors pain, repositioning or removal eliminates the problem. Inserting a “low profile” style plug may allow for more comfortable wear.
Epiphora can result if EDE is treated with a punctal occlusion. In fact, some physicians use epiphora after plug insertion as a diagnostic indicator of evaporative dryness. Fortunately, conventional diagnostic testing and a trial with a temporary collagen plug often decrease the occurrence. Again, extracting the plug will resolve the complaint.
Infections such as dacryocystitis pose a greater risk. Removal of the plug and initiation of an antibiotic such as a fourth-generation fluoroquinolone is recommended. On occasion, surgical intervention is required such as dacryocystorhinostomy.
Punctal canalicular erosion can occur beneath the plug due to chronic irritation. After removing the plug, an antibiotic and steroid will treat acute complaints. Rarely, suturing is necessary to reconstruct the puncta. Dry eye patients who concurrently suffer from ocular allergy may appreciate an increase in symptoms. When an increased tear volume is maintained, the eye is bathed in inflammatory mediators. These mediators can increase itching and redness.2
More from Dr. Hauser: Challenges and opportunities with OSD in 2020
3. Measure twice, plug once
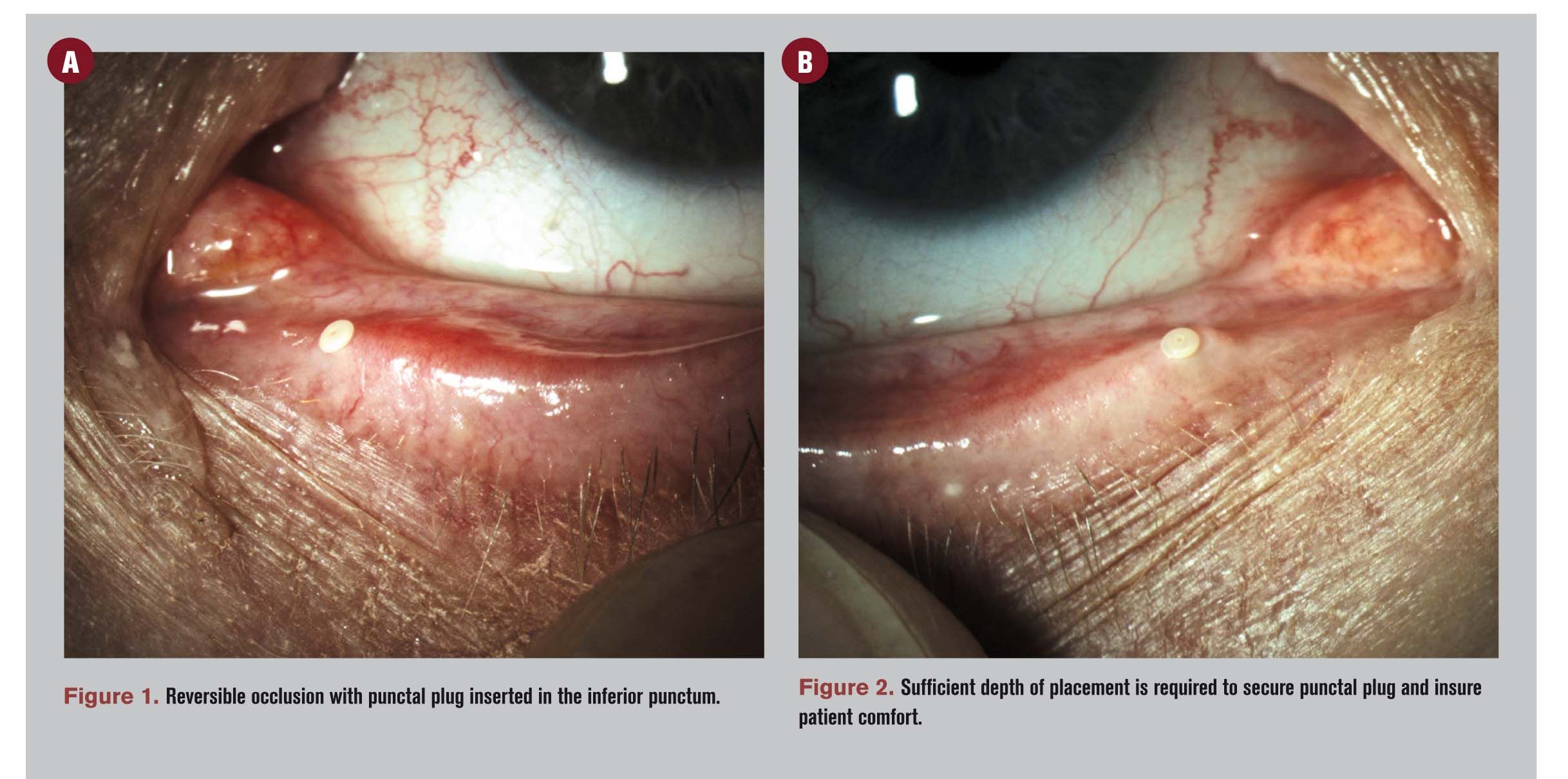
Before selecting a plug or utilizing a gauge to measure, stop and look at the puncta behind the slit lamp. Getting the lay of the land often saves time for the doctor and frustration for the patient. Using a gauge-often provided by the manufacturer-measure the puncta for the appropriate plug size. Ideally, the punctal opening will stretch slightly when the plug is properly inserted. Slight blanching may be noted. If no resistance is felt, the next size up should be attempted. Likewise, if significant resistance is appreciated, a step down is size is warranted. Measuring puncta of the fellow eyelids are recommended due to potential anatomical variations in size and orientation. When in doubt, do not force a plug into place. Keep in mind that extrusion rates with plugs are relatively high. Warn your patient that a reinsertion may be required even with careful measurement.
4. Location, location, location
The inferior canaliculus contributes approximately 60 percent of the maximum outflow of the lacrimal drainage.3 Most physicians start with occluding the inferior puncta, then determine if measurable improvement occurs. If improvement is reported, but symptoms fail to resolve to either doctor or patient satisfaction, insertion of superior plugs may be necessary. Consider, however, that superior plugs are often the last to be inserted and the first removed. Physicians may shy away because they can be tricky to insert from behind the microscope. Patients may not prefer superior plugs because the plugs increase the occurrence of FBS. If symptoms are severe enough to demand superior plugs, thermal cautery is often a better permanent solution.
Related: Why lid wiper epitheliopathy is a game changer
5. Show me the billing
Pitfalls may present from a billing and coding perspective as well as clinically. When medically necessary, Medicare and most major insurance providers will cover punctal occlusion (68761, Closure of lacrimal punctum; by plug, each). As a surgical procedure, supportive documentation in the patient’s medical record is required. Risks, benefits, alternatives, and the procedure itself should be outlined for the patient. Documented informed consent is a necessity. Details of the procedure such as location, brand, size, material, and lot number are logged in the medical record. In terms of medical necessity, punctal occlusion is not an acceptable primary treatment for dry eye disease. Documentation of insufficient or failed therapies is needed before proceeding. A 10-day global fee applies to plug insertion, and the examination is a piece of the global surgical package unless there is a documented and identifiable separate diagnosis.4
Click here for more advice on dry eye!
References
1. Savini G, Prabhawasat P, Kojima T, et al. The challenge of dry eye diagnosis. Clin Ophthalmol. 2008 Mar;2(1):31-55.
2. Kronemyer B. Minimize punctum plug complications by proper patient, design choice. Primary Care Optometry News. 2007 November. Available at: http://www.healio.com/optometry/cornea-external-disease/news/print/primary-care-optometry-news/%7B70201df3-b84f-4126-9bc1-6f15cf58599c%7D/minimize-punctum-plug-complications-by-proper-patient-design-choice. Accessed: 08/07/2015.
3. Murgatroyd H, Craig JP, Sloan B. Determination of relative contribution of the superior and inferior canaliculi to the lacrimal drainage system in health using the drop test. Clin Experiment Ophthalmol. 200 Aug;32(4):404-10.
4. Corcoran Consulting Group. Medicare reimbursement for punctal occlusion with plug (FCI Ophthalmics). Available at: http://www.corcoranccg.com/products/faqs/punctal-occlusion-fci/. Accessed: 08/07/2015.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.