Better manage nocturnal lagophthalmos for dry eye patients
Evaluating lid seal performance key to effectively treat dry eye patients.

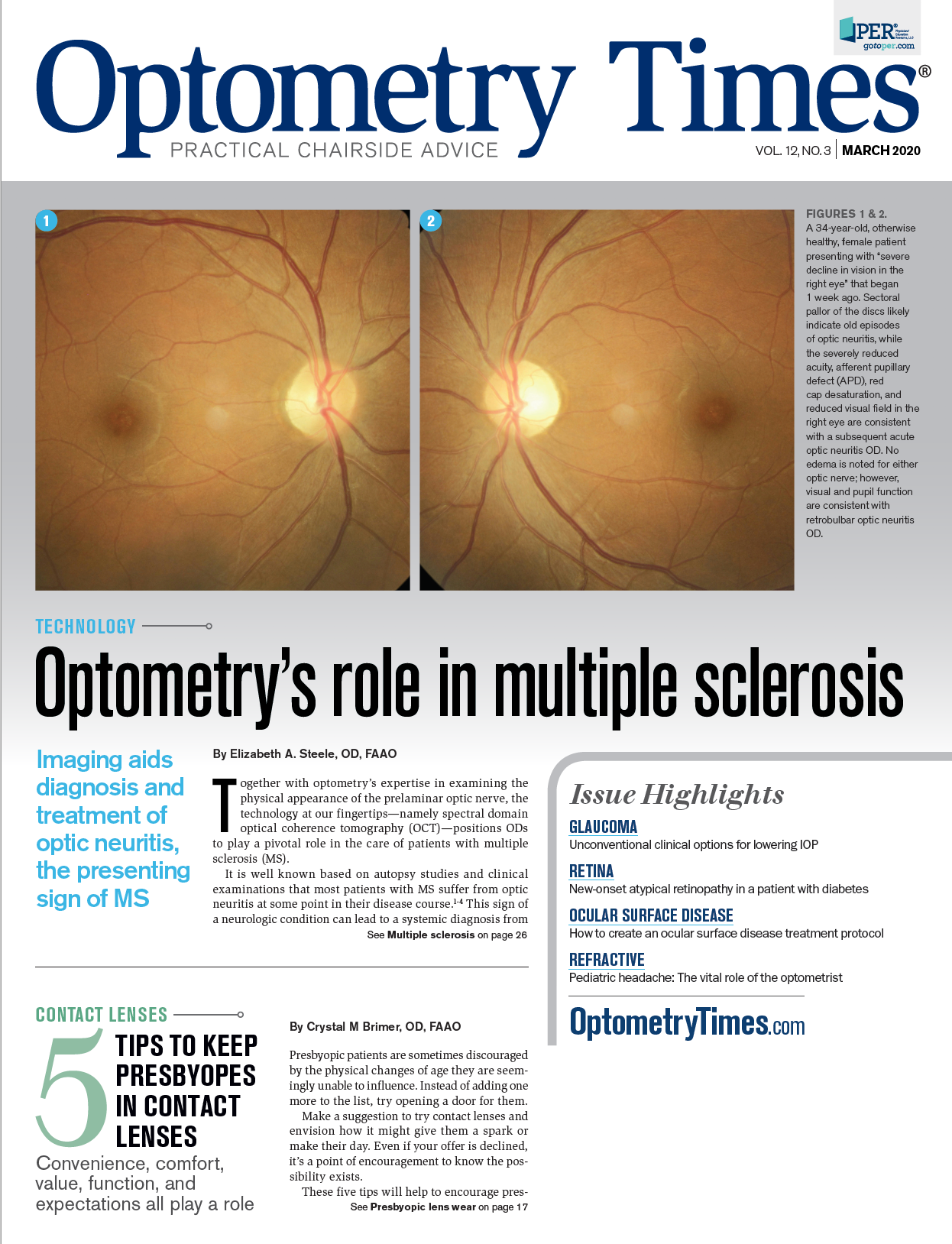
Amy Nau, OD, FAAO, is in group practice in Boston

The Korb-Blackie light test is a simple method for detecting poor nocturnal lagophthalmos and should be used to evaluate patients with dry eye. Once poor lid seal has been diagnosed, appropriate treatment can be given, as shown in the stated case study.
Nocturnal lagophthalmos (NL) describes incomplete eyelid closure during sleep. The problems associated with NL manifest similarly to those from inadequate blinking during the day or prolonged screen use: namely, symptoms of dryness and irritation due to enhanced tear film evaporation, with ensuing ocular surface inflammation.
NL should be proactively investigated and addressed as, from my experience, it can greatly exacerbate other forms of dry eye (such as aqueous-deficient, Bell’s palsy, medication-induced, etc.). It is difficult to successfully treat any dry eye condition if NL is not effectively managed.
Related: Overlooked causes of dry eye
Common triggers for NL include cosmetic surgical procedures, Botox (onabotulinumtoxinA injection, Allergan), Grave’s disease, floppy eyelid syndrome associated with sleep apnea and keratoconus, high axial myopia, lid deformities, age-related lid laxity, senile ectropion, and dermatochalasis.1,2
Diagnosing NL
NL is easily recognized when a patient presents with significant lid deformities. However, more subtle forms (such as lid seal deficiency occurring in patients with normal lid configurations) are frequently overlooked.
In clinical practice, a common scenario involves a patient complaining about ocular discomfort with no obvious cause. Many situations in which discomfort worsens in the morning (upon waking) and resolves slowly throughout the day do not lead to objective clinical findings, making a satisfactory diagnosis elusive.
Related: Common systemic conditions associated with dry eye disease
Standard methods of examination often indicate that lids appear capable of full closure, even though signs and symptom severity peaks in the morning. Even to discerning clinicians, this has been an enigma. It wasn’t until 2015 that researchers realized that, even though lids may appear to be closed, if they are not properly “sealed, air will reach the ocular surface, resulting in evaporative stress and associated symptoms upon awakening.3
Related: Explore the relationship between dry eye and sleep
A simple method for detecting NL is the Korb-Blackie light test, wherein a practitioner places the patient in a darkened room, instructing her to gently close her eyes as if sleeping. Application of a transilluminator placed at the upper tarsal plate will show leakage of light onto the cheek if NL is present. Asking the patient to then tightly squeeze her eyes shut will reveal whether they are capable of complete closure.
Contemporary treatment strategies
Historically, poor awareness of the problem and lack of a diagnostic test prevented identification and treatment of this condition. Typical recommendations for morning dryness include drops used before bedtime, on the assumption that inadequate lubrication is the primary challenge. This erroneous assumption was perpetuated by NIH definitions of dry eye, which until recently focused on aqueous deficiencies as the major cause of dry eye.4 In my experience, ointments can be effective, but they can also irritate a patient’s eyes, blur vision in the morning, fail to protect the eye from desiccating stress, or be contraindicated by medications or comorbidities.
Related: Use aesthetics to treat lid and periorbital conditions
When ointments do not work, fabric sleep masks which can keep the eyes closed may be recommended. In some patients, these are effective. For others, these simple masks are inadequate.
Other interventions, such as use of surgical tape or Breathe Right nasal strips can be used to secure the lids together. Saran Wrap or Cling Wrap combined with fabric sleep masks can also work, with the goal of creating a periorbital high humidity microenvironment.
Related: How to treat dry eye in the pediatric and young adult population
Moisture-chamber goggles designed specifically for the management of dry eye symptoms, including eyeseals or Onyix goggles (Eye Eco), are another option. Finding a solution that produces the desired effect of absence of symptoms upon arising is critical.
Case study
A healthy Caucasian female, age 53, was referred by her primary-care physician due to ongoing problems with dry eye. She had a history of dry eye with blepharospasm, for which she received punctal plugs in all four lids, Restasis (cyclosporin, Allergan) twice daily, and Botox injections, which helped with the blepharospasm but sometimes made her symptoms worse, especially in the morning. She tested negative for Sjögren’s syndrome.
The patient reported that she could no longer read due to dryness and that she used a screen for about four hours daily.
Related: Sleeping position may cause increased glaucoma risk
Her evaluation included the Standardized Patient Evaluation of Eye Dryness (SPEED) questionnaire, and her score of 26 out of a possible 28 confirmed significant discomfort. The patient had moderate meibomian gland dysfunction, with meibography showing approximately 20 percent atrophy of the upper and lower glands, and 50 percent anterior migration of the Line of Marx on the lower lid margins bilaterally.
A meibomian gland evaluator (TearScience)showed severe lower lid obstruction with three glands open on the right lid and two glands open on the left lid. The upper lid on the right eye had 13 glands open and the upper lid on the left eye had four glands open.
Related: Sleep apnea: More than a snore and floppy eyelids
Fluorescein staining showed Grade 1 inferior superficial punctate keratitis (SPK) OD and Grade 2 inferior SPK OS. She exhibited conjunctival chalasis bilaterally. Her osmolarity was 308 OD and 318 OS.
The Korb-Blackie light test was performed with a Finoff transilluminator against the upper eyelid immediately superior to the tarsal plate. The patient exhibited severely compromised lid seal bilaterally, which was worse on the left side. Neither eye fully closed with attempted forced closure.
A diagnosis of NL resulting in desiccating stress led to prescribing ointments before bedtime. The patient was also placed on therapy for meibomian gland dysfunction including compresses (Tranquileyes, Eye Eco), lid margin scrubs with hypochlorous acid, (Avenova) non-preserved lipid-based tears (Retaine MGD), blinking exercises, and Azasite (azithromycin, Akorn) drops for one week, along with reduced screen time and omega-3 supplementation (PRN).
Related: IPL treats rosacea and meibomian gland dysfunction
At the one-month follow-up visit, the patient reported symptom improvement and LipiFlow (Johnson & Johnson Vision) was performed. Gland function improved substantially at the three-month time point, with no corneal staining, normal osmolarity and a SPEED score of 12.
Related: Offer IPL as a treatment for MGD and dry eye disease
However, the patient still exhibited significant symptoms of dryness in the morning and continued to have cosmetic Botox. At this point, we added a moisture-preserving sleep mask (EyeSeals 4.0, Eye Eco) to her prescribed regimen. After sufficient protection was achieved, rapid improvement followed with her SPEED score decreasing to 7.
Conclusion
As eyecare practitioners better understand the nature and importance of NL, they must ensure lid seal is evaluated in all patients with dry eye. Reduction in symptoms necessitates complete enclosure of the periorbital area to promote a high-humidity microenvironment.
Related: How the blink affects contact lens wear
Dr. Nau graduated from The New England College of Optometry and completed a residency in ocular disease with the Boston VA Health Service. Prior to practicing in Boston, Dr. Nau was on staff at the department of ophthalmology at Beth Israel Deaconess Hospital and assistant professor at the University of Pittsburgh. She was the 2008 recipient of the Western Pennsylvania Optometric Association’s Young Optometrist of the Year Award. Her research interests include dry eye and medical contact lenses.
anau@korbassociates.com
References:
1. Latkany RL, Lock B, Speaker M. Nocturnal lagophthalmos: an overview and classification. Ocul Surf. 2006 Jan;4(1):44-53.
2. McNab AA. The eye and sleep. Clin Exp Ophthalmol. 2005 Apr;33(2):117-25.
3. Blackie CA, Korb DR. A novel lid seal evaluation: the Korb-Blackie light test. Eye Contact Lens. 2015 Mar;41(2):98-100.
4. National Eye Institute. Dry Eye. Available at: https://www.nei.nih.gov/sites/default/files/health-pdfs/factsaboutdryeye.pdf. Accessed 2/28/20.
5. Korb DR, Greiner JV, Glonek T, Esbah R, Finnemore VM, Whalen AC. Effect of periocular humidity on the tear film lipid layer. Cornea. 1996 Mar;15(2):129-134.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.