Blog: Examine evaporative dry eye disease exposure in your patients
Interpalpebral corneal staining of a healthy patient who frequently travels on planes, rides a motorcycle without eye protection, and spends 4 to 6 hours a day on a computer.

The views expressed here belong to the author. They do not necessarily represent the views of Optometry Times or Multimedia Healthcare.
Some 30 million people in the world suffer from dry eye disease (DED). It is estimated that more than 85 percent of this population experiences symptoms associated with evaporative influences and meibomian gland dysfunction (MGD).1
Exacerbated by numerous intrinsic and extrinsic factors, an insult to the cornea results in the breakdown of one or more of the aqueous, lipid, and/or mucin layers of the tear film.
This causes chronic damage to the surface of the epithelium, while notoriously contributing to fluctuations in vision, burning, stinging, and watering eyes.
Related: Understanding prevalance, demographics of dry eye disease
In order to solve the root problem, it is important to address the underlying cause(s) of tear film instability before more serious problems-such as permanent loss of meibomian gland function-occur. Sometimes the main cause of evaporative DED is hidden in a patients’ medications list, contact lens habits, or everyday home and work environments.
Frequent causes of the evaporative component that I have seen in my dry eye patients include environmental factors, improperly placed fans/vents, continuous positive airway pressure (CPAP) masks, prolonged computer usage, contact lens wear, and medications such as topical eye drops with preservatives.
These common evaporative influences can leave the ocular surface vulnerable and appear to affect people all ages.
Pictured to the right: Interpalpebral corneal staining of Sjogren’s patient who has incomplete blinks after a previous blepharoplasty, and who is also a glaucoma patient using 2 different glaucoma drop daily.
Related: How to use tear osmolarity to help treat dry eye disease
Evaporative factors
Evaporative factors to be considered asking when assessing DED include:
Altitude, low humidity, windy places
Environments such as airplanes contain low humidity and cause increased tear film evaporation, resulting in a decrease in tear film break-up time (TBUT).2 Areas with higher altitude and little to no humidity can also cause the perfect storm for dry eye symptoms.2
A constant breeze of air across the cornea for an extended amount of time destabilizes the tear film and is never ideal. Other common everyday windy activities contributing to evaporative DED can include sleeping with overhead ceiling fans and riding in a vehicle with the windows down.
Additionally, the positioning of air vents pointed at the face-while a person is awake or asleep, at home or at work, in the car or in bed-can have a significant impact on chronic fluctuation in vision throughout the day.
Related: Explore the relationship between dry eye and sleep
CPAP machine
To make evaporative DED even worse, imagine someone who also sleeps with an additional continuous stream of airflow on the cornea all night, every night. CPAP devices are often found to be ill-fitting and cause air to blow directly into the eyes from a mask leak. Be on the lookout for interpalpebral corneal staining in these patients.
Prolonged device time/reading
Computer use and extended reading have been associated with a decreased blink rate, causing tear film instability.1
Screen time has been shown to reduce blink rates by about 78 percent, decreasing from about 20 blinks per minute before screen use to about four blinks per minute during screen use.3 Asking patients more questions about details of their occupations and work demands reveals how often they are immersed in using computers and electronic devices.
Contact lenses
DED is the primary reason for dropout among contact lens wearers. Associated with increased evaporative tear loss, contact lens wear can cause abnormal tear osmolarity and MGD.1
In my office, daily contact lenses and preservative-free artificial tears (with an increased lipid component) are often recommended to improve comfort.
For more moderate to severe cases of contact lens-related DED, a combination of punctal plugs and either lifitegrast ophthalmic solution 0.5% (Xiidra, Shire) or cyclosporine 0.05% (Restasis, Allergan) is recommended.
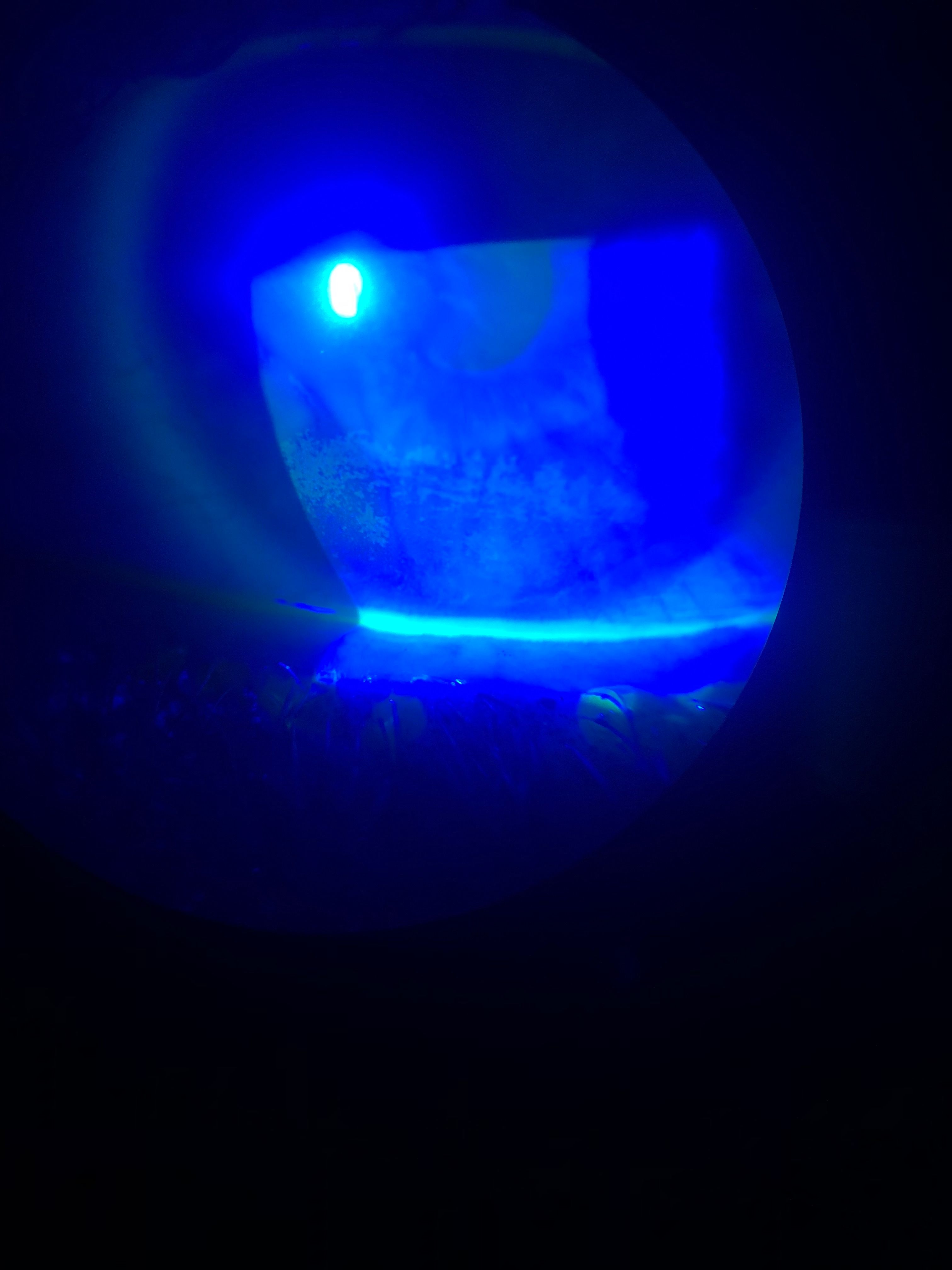
Pictured to the right: Interpalpebral corneal haze and dryness due to lagopthalmos, nightly overhead ceiling fan, and overnight CPAP use with mask leak.
Related: Combating dry eye with punctal plugsTopical drugs or systemic medicines
Of the top 100 orally-prescribed systemic medications in the U.S., about 20 percent have been found to be associated with DED as a side effect.1
The preservative benzalkonium chloride (BAK) commonly found in topical eye drops is correlated with amplifying evaporative dry eye. Research has shown that when taking three topical glaucoma drops every day, 40 percent of patients were suffering from dry eye as a side effect.1
To help reduce the amount of glaucoma medicines needed, it may be a good idea to consider options such as selective laser trabeculectomy (SLT) to decrease the amount of topical preservatives.
Related: Targeting dry eye in glaucoma patients
Intrinsic factors
Other intrinsic factors such as lid aperture disorders, incomplete blinks, lagophthalmos, and meibomian gland oil deficiency can also be combined with the previously mentioned factors to produce even worse evaporative dry eye signs and symptoms.2
Any abnormal anatomical positioning of the eyelids can directly cause meibomian oil deficiency because the oil from the meibomian glands is not dispersed properly into the tear film when blinking.
Because inferior corneal staining and DED may be intermittent and not picked up in an annual eye exam-and can occur with seemingly functional meibomian glands-it is important to ask the right questions.
Related: Blog: Don't leave dry eye disease patients high and dry
For every patient who mentions “blurry,” “burning,” “watering,” or “irritating” eyes, sodium fluorescein is used to assess the TBUT to highlight areas of epithelial defects of the inferior or interpalpebral cornea.
Staining the cornea also enables me to take a photo in order to educate the patient on why her vision is being affected by dryness. I have found that dry eye patients are more motivated to remain compliant with the treatment plan if they understand the extend of the damage being done.
On examination, I also find it helpful to visualize the aberrations caused by tear film disruption and epithelial defects via retroillumination of the cornea.
Conclusion
The modern risk factors for evaporative DED are not the same as 30 years ago. dry eye is changing, and it is likely that the population of affected patients will continue to grow.
Listening for vague complaints of watering, burning, stinging, foreign body sensations, photophobia, and fluctuations in vision can all be symptoms of dry eye and can greatly impact patient’s activities of daily living. It is important to assess other factors such as lid function, environmental factors, and behavioral factors that may exacerbate evaporative DED.
Pictured to the left: Interpalpebral corneal staining of a healthy teenager who sleeps with numerous fans and vents pointed towards the face
Pictured to the right: Interpalpebral staining in a patient with decreased blinks associated with excessive computer screen time (8 to 10 hours per day), and poor placement of overhead vents at home and at work.
Disclosure: Dr. Coats is a speaker and on the advisory board for Shire/TakedaRead more dry eye awareness content here
References:
1. Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo CK, Liu, Nelson JD, Nichols JJ, Tsubota K, Stapleton F. TFOS DEWS II Definition and Classification Report. Ocul Surf. 2017 Jul;15(3):276-283.
2. Calonge M, Pinto-Fraga J, González-GarcÃa MJ, EnrÃquez-de-Salamanca A, Lopez-de la Rosa A, Fernández I, Lopez-Miguel A. Effects of the External Environment on Dry Eye Disease. Int Ophthalmol Clin. 2017 Spring;57:2:23-40.
3. Wensi S, Baker R, Chuke JC, Rouholiman BR, Hasan BR, Hasan SA, Gaza W, Stava MW, Porter JD. Age-related changes in human blinks: passive and active changes in eyelid kinematics. Invest Ophthalmol Vis Sci. 1997 Jan;38(1):92-9.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.