Blog: Understand the science and art of managing chronic conditions
The views expressed here belong to the author. They do not necessarily represent the views of Optometry Times or Multimedia Healthcare.
Optometry is a remarkably empowering profession. ODs care for patients’ visual welfare through appropriate refractive correction and optimizing ocular health. Within the last 15 years, the technologies available to both diagnose and treat ocular conditions has drastically changed.
Looking back at our brief history as optometrists has been enlightening. Refractive care of patients is usually managed as a long-term chronic condition, but its symptoms are treated effectively by power changes that can be noticed immediately by the patient.
This makes refractive conditions somewhat straight forward as changes in treatment (the prescription in lenses), provides patients immediate improvement in symptoms.
Previously by Dr. Brujic and Dr. Kading: Blog: Keep an eye on meaningful metrics in the new year
An example is a myope whose myopia has progressed, and we are now increasing the power in his glasses. This provides immediate benefits to the patient.
If the patient is solely an eyeglass wearer, we can demonstrate the patient’s new prescription immediately with the help of loose lenses held over his glasses.
With a contact lens wearer, ODs have an opportunity to demonstrate the immediate benefits of the new prescription by placing the patient’s updated prescription on his eyes.
This clinical interaction produces a positive patient response for the patient by providing a change in treatment (prescription change) after managing a chronic condition.
With the chronic condition of myopia, the acute symptom is a change in vision. A positive patient response is delivered by an appropriate refractive correction-through glasses and/or contact lens prescription.
Related: Treating and diagnosing myopia
Chronic ocular disease
Chronic ocular disease brings a different set of opportunities and challenges with it. Glaucoma, for example, allows ODs to help patients avoid the potentially blinding effects of a condition that-for most patients-is relatively asymptomatic until the condition is advanced.
Glaucoma can be diagnosed and treated by ODs in most states in the United States. Many ODs are directly involved in caring for these patients by making decisions on whether intraocular pressures (IOPs) are appropriately controlled in light of exam and diagnostic test findings. But, there are differences in managing a patient with this condition versus a patient experiencing a change in refractive error.
Related: Chronic ocular diseases and patient psyche
Patient care
Despite both being chronic conditions and requiring long-term patient care, these individuals are managed with different expectations.
When managing a glaucoma patient, ODs may think they are successful with treatment because they have attained their set IOP goal.
Yet, the patient doesn’t see any better because of the treatment. The patient doesn’t feel any better because of the treatment.
Interestingly, a significant portion of patients may experience symptoms created by the medications ODs utilize to treat the condition.
This is what can often make compliance with glaucoma treatment a challenge. Unlike correcting refractive error, glaucoma treatment does not necessarily improve symptoms with successful treatment.
Related: Why documenting target IOP helps ODs
ODs’ responsibility
An OD’s role in treating the glaucoma patient is similar to the primary care physicians’ or endocrinologists’ role in treating a diabetic patient.
Those healthcare providers utilize objective metrics-such as hemoglobin A1c levels-in order to determine success or failure with treatment.
Although elevated glucose levels can have other effects on a person’s physiology, it will be the success or failure of maintaining appropriate glucose levels that will determine the long-term ramifications to other end organs-including the eye.
This is a similar strategy that ODs employ with glaucoma patients. Although ODs know the pathophysiology of glaucoma can be complex, the one modifiable risk factor is modifying the IOP.
Related: How to improve glaucoma referrals
Increasing amounts of technologies
Technological advancements have made tremendous improvements in how ODs diagnose and manage a number of conditions in their practices.
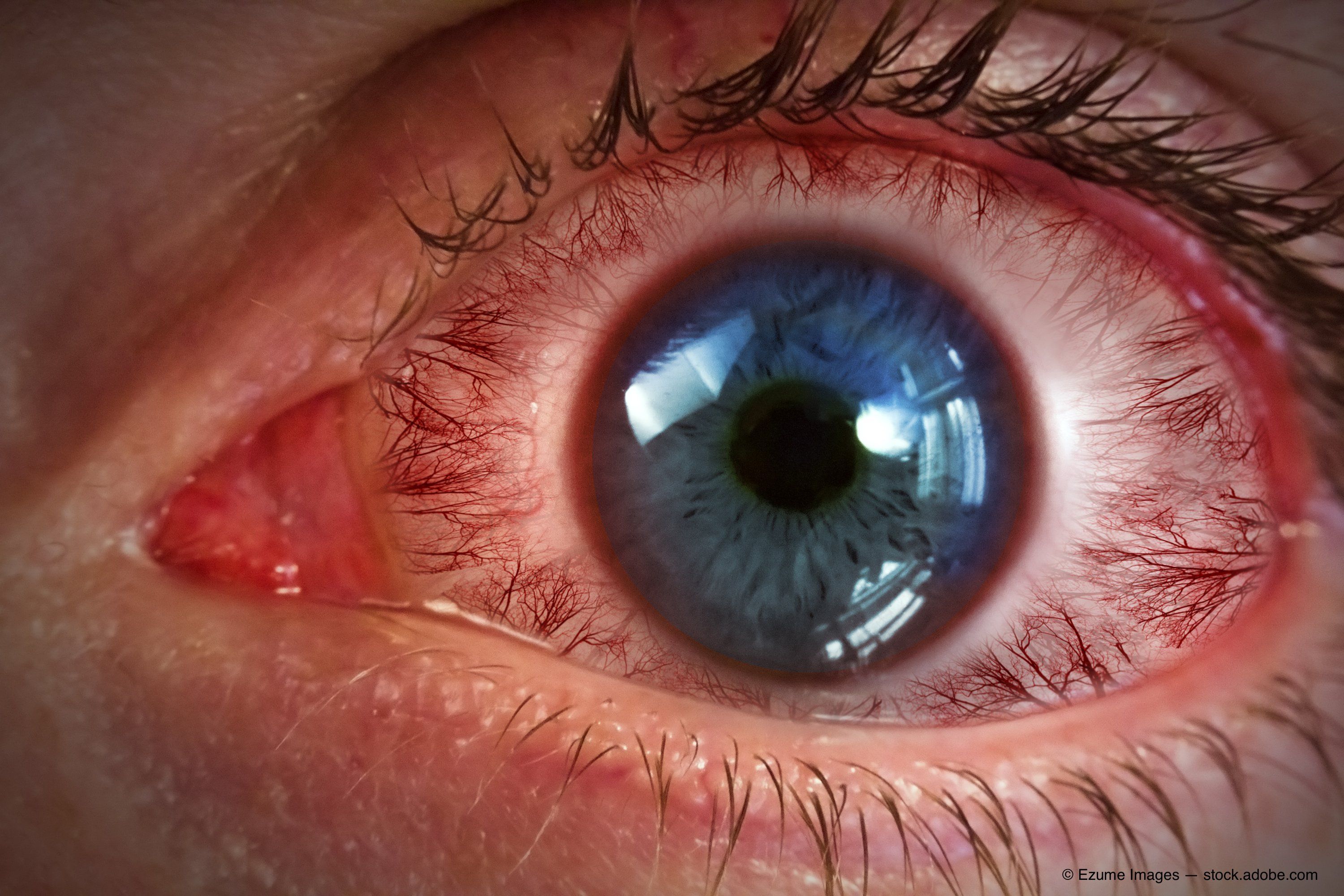
Our understanding, diagnosis, and management of ocular surface disease has expanded because of the passion behind the companies developing the tools available to manage this condition.
About 15 years ago, ODs identified dry eye by a patient’s complaint of ocular dryness. We often treated the condition with artificial tears.
For those practitioners who have embraced dry eye management, we understand that artificial tears have a place for temporarily ameliorating the symptoms a patient experiences.
But we now have technologies to improve how the ocular surface functions. ODs now understand that it is the delicate balance of appropriately produced tears, along with a functional blink, that will lead to the most successful outcomes.
With that said, managing a chronic condition such as dry eye disease requires a new set of clinical rules. ODs need to be cognizant of inflammation on the ocular surface, tear volume, health of the lids and meibomian glands, and with exogenous factors that may affect the way tears are formed on the eyes.
Related: Modern-day techniques for diagnosing dry eye disease
Manage the condition
Because there is no known cure for dry eye disease-only effective ways to manage the condition-more patient visits are required to help rehabilitate the ocular surface.
Improvement in both signs and symptoms is the goal; it usually requires a strategic approach that is multifaceted in nature. This is different than providing an updated glasses or contact lens prescription when managing a patient’s refractive error-the patient is able to immediately benefit from the new prescription.
Multiple clinic visits throughout the year instead of a single visit are often required when managing chronic ocular disease.
It is critical for an OD to give clear guidance to the patient on a treatment plan and appropriate expectations, including potential side effects from the treatment.
Related: Dry eye protocol for any practice
Evolving care
The way ODs manage refractive conditions today is much different than how we did in the past. Myopia progressing in the pediatric patient used to simply be corrected optically. Now, through myopia management, ODs are actively managing this condition through slowing the progression of myopia.
As diagnostics and treatments continue to evolve, ODs’ involvement in managing chronic ocular conditions will continue to increase. A greater portion of our clinical time is already devoted to managing many of these chronic conditions, and it will likely continue to only increase as optometry’s role in medically managing patients grows.
Understanding the scientific rationale for the diagnostics and treatments utilized to manage these conditions is critical. But understanding the difference in management strategy with chronic conditions provides us with the art of managing these conditions and our patients at more appropriate levels.
A successful understanding of the science and art of appropriately caring for chronic ocular conditions will offer us the best opportunity to best manage these patients that need our care the most.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.