How to help patients who are depressed


Optometrists may encounter patients who are depressed due to their vision loss. Some may remark that they feel like prisoners in their own home (feelings of social isolation), while others may mention having suicidal thoughts.
Patients experiencing reduced or low vision due to age-related macular degeneration (AMD), glaucoma, corneal disease, and other ocular conditions may be at risk.
As optometrists we are well versed in the ocular side effects of antidepressants and related medications, but what else should we know?
Suicide in the news
Since the recent suicides of celebrities Kate Spade and Anthony Bourdain, there has been increased media attention and discussion concerning mental health and depression.
The World Health Organization reports that depression is one of the leading causes of disability in the world with over 300 million people affected and has increased by more than 18 percent between 2005 and 2015.1 Depression is treatable with medications and or psychotherapy.2 However many people with mental disorders go untreated3 possibly due to its stigma, poor awareness, lack of insurance coverage, and economic or cultural concerns.
Mental illness
As defined by the American Psychiatric Association (APA), “mental illnesses are health conditions involving the changes in thinking, emotion or behavior (or a combination of these) and are associated with distress and/or problems functioning in social, work or family activities.”4
There is a large range and types of mental health disorders. In fact, the Diagnostic and Statistical Manual of Mental Health Disorders 5 (DSM-5), published by the APA, defines 297 of them, of which many can share the same signs and symptoms as well as be causative to each other or associated with other health conditions causing depressive symptoms.
Common mental health disorders listed in DSM-5:
• Anxiety disorder
• Mood disorder
• Addiction disorder
• Eating disorder
• Attention deficit disorder
• Personality disorder
• Obsessive compulsive disorder
• Post-traumatic stress disorder
Depression
Depression (also called, major depressive disorder or clinical depression) is characterized as a mood disorder, which affects over 16.1 million Americans.3 It is seen in more women than men because men may be less likely to seek treatment2 and is more prevalent in adults with a median age of 32.5 years.3 Half of those who have had previous treated depression are more likely to have a reoccurrence.5
The signs and symptoms of depression are much more than feeling sad or “feeling the blues.” It is normal to feel sad after losing a loved one, going through a major life change, or failing an exam. This is part of normal mood variations. However, with depression these sad feelings persist and negatively affect a person’s daily life over a longer than normal period of time.
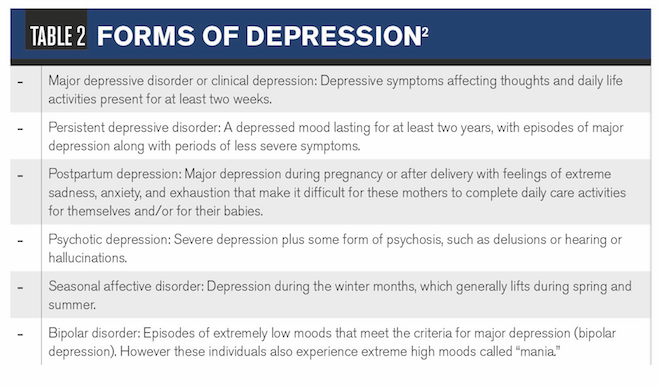
The signs and symptoms of depression may range from constant sadness and negative feelings to anhedonia (loss of interest in activities once enjoyed), hopelessness, or thoughts of suicide or a suicide attempt (See Table 1 for complete list).
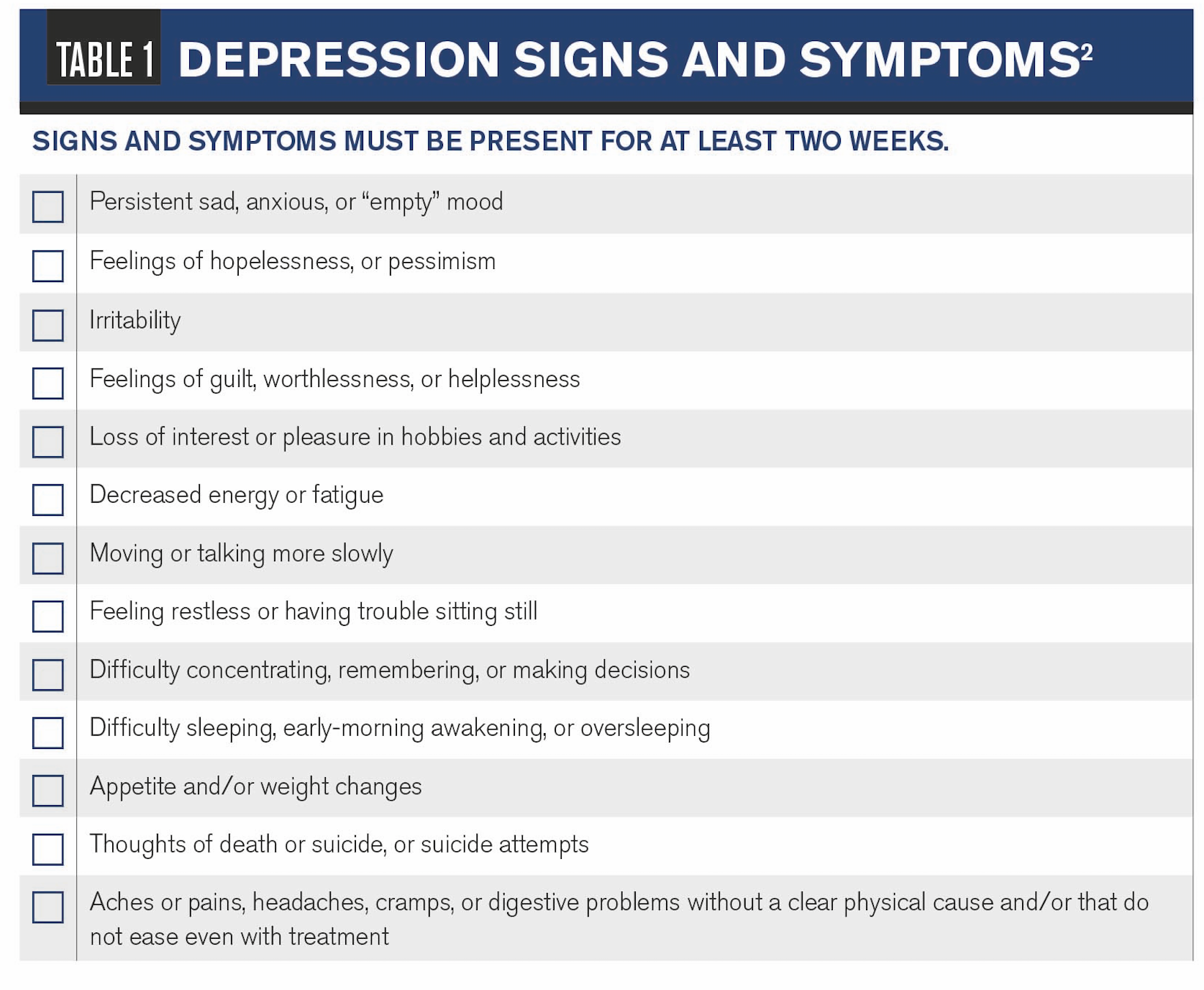
Forms of depression include persistent depressive disorder (or dysthymia), postpartum depression, psychotic depression, seasonal affective disorder, and bipolar disorder (see Table 2).
Although different, depression is sometimes confused with anxiety and other disorders. According to the Anxiety and Depression Association of America (ADAA), about 50 percent of those diagnosed with depression also have some form of anxiety disorder.3
Because both conditions may share similarities, the major difference is that someone with anxiety is worried about an outcome; while someone who is depressed thinks the outcome will always turn out negative and nothing in his power can change it.
Screening for depression
Screening and early referral for diagnostic evaluation can lead to early treatment. It is reported that the prognosis of depression may depend on early treatment with medication because longer untreated depression was related to severity.6
Many screening scales are available in the form of questionnaires based on patient signs and symptoms. If scored positive, a referral is warranted for further diagnosis and decision-making for treatment. Commonly, referrals are made to primary-care physicians (PCPs) or mental health professionals.
Screening scales used include Beck Depression Inventory (21-question scale), Geriatric Depression Scale (meant for elderly and for those with mild to moderate dementia), Patient Health Questionnaires (PHQ-2 & PHQ-9), and DSM-5 Self-Rated Level 1 Cross-Cutting Symptom Measure (consisting of three different age appropriate forms) which can then also be used to monitor progress.
These forms can be downloaded online.
Because many people with depression go untreated or undetected, researchers suggest PCPs might be best to recognize the condition early and to implement screenings at their practices.7 However, barriers both on the doctor and patient sides exist, which include stigma of depression, unwillingness of patient to discuss, or doctors solely concentrating on physical symptoms.8
Screenings at PCP offices have increased over the years; however, reports state that it is not enough.9
One study, which screened patients at State University of New York (SUNY) College of Optometry’s primary eye care clinic, suggests using PHQ-2 screening (consisting of two questions) and if positive, using a secondary screening tool to prevent over referral for further services.10
Another study, consisting of patients from a PCP clinic, agrees; however; researchers specifically recommended patients to complete PHQ-9 screening (consisting of nine questions, of which the first two questions is PHQ-2).7
Today, Facebook and other social media outlets are also being studied on how they influence or can help detect depression.
Raquel Van Der Biest, occupational and low vision therapist at the Miami Lighthouse for the Blind and Visually Impaired, says she uses Geriatric Depression Scale as part of her client’s assessment along with a functional assessment, prior to patient’s seeing the optometrist. If the screening is positive, she talks with the patient and makes a referral.
Van Der Biest shared in personal conversation that 47 percent of her patients from 2013-2018 screened positive. She stresses the importance of patients’ well-being to be included in their low vision care.
Because risk for depression is associated with vision loss and other chronic conditions (stroke, loss of hearing, and cardiac and chronic lung disease) in older age,11 optometrists can easily implement screening in their offices for low vision and ocular disease or general care patients.
ODs might consider The World Health Organization’s (WHO) mental health intervention guide meant for use by non-specialized practitioners.
Vision loss and depression
Most patients with vision loss are elderly, who in general have a higher rate of depression due to factors such as other disease, previous depression, social isolation, or loss of independence.
However, vision loss increases the risk of clinical depression.12 Many patients with vision loss become scared, nervous, angry, and as I have seen, lose hope. Depression also interferes with rehabilitation success, making low vision treatment goals more difficult to reach.
Related: How ODs can help combat depression in glaucoma patients
With age-related macular degeneration (AMD) expected to double by the year 2050,13 confronting depression needs to become part of the eyecare exam. The American Optometric Association and the American Academy of Ophthalmology recognize this need and recommend referral for mental health services in their respective vision rehabilitation guidelines.14,15
However, programs to help eyecare providers increase their understanding of depression may be needed. Instruction of its recognition has been shown to help eye doctors respond better to depression in patients with vision loss.16
When it comes to depression, knowledge is power for patients. In a large group of glaucoma patients, less depression was revealed in patients who had more understanding of their eye diseases.17 Chair time spent explaining a patient’s disease may not go in vain.
After low vision assessment, consider referring the patient for services with a certified low vision rehabilitation specialist and mental health professional. The combination of these along with specific behavioral therapy (such as increasing adaptive behavior and achieving wanted goals) reduced the incidence of depression in half of AMD patients.18 Another study showed that this model increased patients’ ability to perform daily activities.19
The Depression in Visual Impairment Trial (DEPVIT) found decreased depressive symptoms in subjects who received problem-solving therapy vs. referral to a PCP alone; however, this decrease was not statistically significant.20,21
Researchers are recommending a stepped-care approach to reduce depression in visually impaired patients, including physical activity, self-help programs, behavioral or problem-solving therapy, and medication.22 More study is needed to find the best method.
Related: Therapy helps with depression in AMD patients with low vision
Says Van Der Biest: “It is important for doctors to refer their patients for a rehabilitation program to learn how to be more independent in an environment with more social interaction to help with depression. It opens up new possibilities-I have seen clients explore new interests with enjoyment and take part in other programs such as learning technology, art, and music.”
I have seen the benefits of these programs. A few years ago, a patient spoke with me about thoughts of suicide. Through the help of a rehabilitative program, he is now thriving and gives talks on its benefits to help others.
The American Foundation for the Blind, through its Vision Aware Program, offers resources and a directory of national and local programs and services. Search the site at www.visionaware.com, and keep a list handy for referrals.
Younger and middle-aged patients may present with a different set of challenges than the senior population, but they are not immune to depression. Of 103 patients aged 13-65 years with Lebers hereditary optic neuropathy, 49.5 percent met the criteria of depression and had a negative impact when it came to their interpersonal life and career goals.23
Rafael Ramirez, area sales manager for OrCam Technologies, has been visually impaired since birth.
“When I was young, things were fine, but as I grew I realized there were things I could not do,” he says. “This became tied to my self-worth. As I grew older, depression set in and interfered with my thoughts of ever having a relationship. Who wants to be with a blind guy? I had suicidal thoughts but never tried it. But then someone’s love turned the key for me. Though my visual impairment was still inconvenient, it didn’t eat away at my soul like before. It’s a mental journey. Once you stop dwelling on it, you begin living.”
Depression and suicide
In 2016, The Centers for Disease Control reported that there were more deaths by suicide (nearly 45,000) in the U.S. than homicides and ranked suicide among the top 10 causes of death in America.24
Reasons for suicide are multifactorial and may not be secondary to a mental illness. While depression can be a risk factor, just over half of the people who die by suicide did not have a known mental health disorder.25 This statistic emphasizes the importance of mental health awareness among all healthcare providers, including ODs.
Methods for better detection by healthcare providers are being studied. One study found that PCPs often asked about suicidal thoughts only with increases in depression.26
People more risk for suicide are those with a previous attempt, family history, substance abuse history, mood disorder, access to lethal means of carrying out a suicide, a recent loss or failure (relationship breakup, death of loved one, academic failure), legal or financial difficulties, being bullied, history of trauma or abuse, chronic physical illness or pain, and exposure to other suicidal behavior.27
The Substance Abuse and Mental Health Services Administration (SAMHSA) established the National Suicide Prevention Lifeline: 1-800-273-TALK (8255). The Lifeline offers toll-free 24-hour access to one of 160 U.S. crisis centers. Help is also available via online chat via
. Military veterans who call will be immediately connected to a professional Veterans Affairs counselor.
SAMHSA offers its Suicide Safe app to help healthcare providers integrate suicide prevention strategies into their practices and address suicide risk among their patients. It is available on Google Play and the Apple App Store.
Suicide prevention also comes from family, friends, or others recognizing the warning signs. The American Foundation for Suicide Prevention lists the following signs.28At-risk talk
• Killing themselves
• Feeling hopeless
• Having no reason to live
• Being a burden to others
• Feeling trapped
• Unbearable pain
Risk behavior
• Increased use of drugs or alcohol
• Searching for a method for suicide
• Withdrawing from activities
• Isolating themselves from family and friends
• Sleeping too much or too little
• Visiting or calling people to say goodbye
• Giving away possessions
• Aggression
• Fatigue
Mood Risk
• Depression
• Anxiety
• Loss of interest
• Irritability
• Humiliation/shame
• Agitation/anger
• Relief/sudden improvement
What now?
Depression is a disease that should not be trivialized and can be severely debilitating. While it is a recognizable and a treatable medical disease, gaps exist for detection. ODs likely spend more face time with patients than others in health care and are well positioned to make a difference for depressed and suicidal patients. However, further training and research for best practices are still needed.
In my experience, optometry is filled with empathetic doctors who may want to consider implementing a depression screening process. Discussing depressive symptoms with patients and caring for their well-being may give patients confidence in their treatments, ease anxieties, or even save a life.
While depression screening may seem most appropriate for low vision patients, I suggest we consider it for others. ODs can understand how someone diagnosed with macular degeneration can become depressed, but what about the chronic dry eye patient? Everyone addresses life stresses differently.
Consider implementing screening for general patients if you notice changes in a long-time patient, or take a moment to ask patients who are on antidepressants, how they are doing. Recognize warning signs and ask patients if they need help. Letting people know you care can go a long way.
Read more from Bryan Wolynski.
References:
1. World Health Organization. Depression. Available at: http://www.who.int/news-room/fact-sheets/detail/depression. Accessed 7/10/18.
2. National Institute of Mental Health. Depression. Available at: https://www.nimh.nih.gov/health/topics/depression/index.shtml. Accessed 7/10/18.
3. Anxiety and Depression Association of America. Facts and Statistics. Available at: https://adaa.org/about-adaa/press-room/facts-statistics. Accessed 7/10/18.
4. American Psychiatric Association. What is Mental Illness? Available at: https://www.psychiatry.org/patients-families/what-is-mental-illness. Accessed 7/10/18.
5. American Psychiatric Association. Help With Depression. Available at: https://www.psychiatry.org/patients-families/depression. Accessed 8/16/18.
6. Hung CI, Liu CY, Yang CH. Untreated duration predicted the severity of depression at the two-year follow-up point. PLoS One. 2017 Sep 21;12(9):e0185119.
7. Arrol B, Goodyear-Smith F, Crengle S, Gunn J, Kerse N, Fishman T, Fallon K, Hatcher S. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann Fam Med. 2010 Jul-Aug;8(4):348-53.
8. Saver BG, Van-Nguyen V, Keppel G, Doescher M. A qualitative study of depression in primary care: missed opportunities for diagnosis and education. J Am Board Fam Med. 2007 Jan-Feb;20(1):28-35.
9. Bhattacharjee S, Goldstone L, Vadiei N, Lee JK, Burke WJ. Depression Screening Patterns, Predictors, and Trends Among Adults Without Depression in Ambulatory Settings in the United States. Psychiatr Serv. 2018 Jul 9:appips201700439. doi: 10.1176/appi.ps.201700439. [Epub ahead of print]
10. DellaBella ME, Schwartz SH, Nehmad L. The PHQ-2 as a Screening Tool for Clinical Depression in a Primary Eye-Care Clinic. Invest Ophthalmol Vis Sci. 2010 April;51(13):5360.
11. Huang CQ, Dong BR, Lu ZC, Yue JR, Liu QX. Chronic diseases and risk for depression in old age: a meta-analysis of published literature. Ageing Res Rev. 2010 Apr;9(2):131-41.
12. Casten RJ, Rovner BW. Update on depression and age-related macular degeneration. Curr Opin Ophthalmol. 2013 May;24(3):239-43.
13. National Eye Institute. Age-Related Macular Degeneration (AMD). Available at: https://nei.nih.gov/eyedata/amd. Accessed 7/10/18.
14. American Optometric Association. Optometric Clinical Practice Guideline: Care of the Patient with Visual Impairment (Low Visual Rehabilitation). Available at: https://www.aoa.org/documents/optometrists/CPG-14.pdf. Accessed 8/16/18.
15. Fontenot JL1, Bona MD2, Kaleem MA3, McLaughlin WM Jr4, Morse AR5, Schwartz TL6, Shepherd JD7, Jackson ML8; American Academy of Ophthalmology Preferred Practice Pattern Vision Rehabilitation Committee. Vision Rehabilitation Preferred Practice Pattern. Ophthalmology. 2018 Jan;125(1):P228-P278.
16. Rees G, Mellor D, Heenan M, Fenwick E, Keeffe JE, Marella M, Lamoureux EL. Depression training program for eye health and rehabilitation professionals. Optom Vis Sci. 2010 Jul;87(7):494-500.
17. Kong XM, Zhu WQ, Hong JX, Sun XH. Is glaucoma comprehension associated with psychological disturbance and vision-related quality of life for patients with glaucoma? A cross-sectional study. BMJ Open. 2014 May 26;4(5):e004632.
18. Rovner BW, Casten RJ, Hegel MT, Massof RW, Leiby BE, Ho AC, Tasman WS. Low vision depression prevention trial in age-related macular degeneration: a randomized clinical trial. Ophthalmology. 2014 Nov;121(11):2204-11.
19. Deemer AD, Massof RW, Rovner BW, Casten RJ, Piersol CV. Functional Outcomes of the Low Vision Depression Prevention Trial in Age-Related Macular Degeneration. Invest Ophthalmol Vis Sci. 2017 Mar 1;58(3):1514-1520.
20. Margrain TH, Nollett C, Shearn J, Stanford M, Edwards RT, Ryan B, Bunce C, Casten R, Hegel MT, Smith DJ. The Depression in Visual Impairment Trial (DEPVIT): trial design and protocol. BMC Psychiatry. 2012 Jun 6;12:57.
21. Nollett CL, Bray N, Bunce C, Casten RJ, Edwards RT, Hegel MT, Janikoun S, Jumbe SE, Ryan B, Shearn J, Smith DJ, Stanford M, Xing W, Margrain TH. Depression in Visual Impairment Trail (DEPVIT): A Randomized Clinical Trial of Depression Treatments in People with Low Vision. Invest Ophthalmol Vis Sci. 2016 Aug 1;57(10):4247-54
22. Van der Aa HP, van Rens GH, Comijs HC, Margrain TH, Gallindo-Garre F, Twisk JW, van Nispen RM. Stepped care for depression and anxiety in visually impaired older adults: multicentre randomised controlled trial. BMJ. 2015 Nov 23;351:h6127.
23. Garcia GA, Khoshnevis M, Gale J, Frousiakis S, Hwang TJ, Poincenot L, Karanjia R, Baron D, Sadun AA. Profound vision loss impairs psychological well-being in young and middle-aged individuals. Clin Ophthalmol.2017 Feb 22;11:417-427.
24. Centers for Disease Control. 10 Leading Causes of Death By Age Group, United States – 2016. Available at: https://www.cdc.gov/injury/images/lc-charts/leading_causes_of_death_age_group_2016_1056w814h.gif . Accessed 7/9/18.
25. Centers for Disease Control. Suicide rising across the US. Available at: https://www.cdc.gov/vitalsigns/suicide/index.html. Accessed 8/15/18.
26. Nutting PA, Dickinson LM, Rubenstein LV, Keeley RD, Smith JL, Elliot CE. Improving detection of suicidal ideation among depressed patients in primary care. Ann Fam Med. 2005 Nov-Dec;3(6):529-36.
27. American Psychiatric Association. Suicide Prevention. Available at: https://www.psychiatry.org/patients-families/suicide-prevention. Accessed 7/15/18.
28. American Foundation for Suicide Prevention. Risk Factors and Warning Signs. Available at: https://afsp.org/about-suicide/risk-factors-and-warning-signs/. Accessed 7/17/18.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.