Know the latest on classifying and referring hypertension
Routinely and accurately measuring blood pressure in office can influence patient health
Measuring blood pressure has become more routine in the care of patients and, like other numeric data points collected within an optometric exam, ODs compare their findings against a norm. Without a standard set of guidelines for both classification of elevated blood pressure readings and also referral urgency, the information is virtually useless.
Luckily, there are several sets of internationally recognized guidelines for the diagnosis of hypertension. The problem is that they do not all agree on the “standards.” The most recently published, in fact, created quite a stir.1-4
Defining hypertension
Hypertension, based on most current standards, is defined as having a measured blood pressure of ≥140 mm Hg systolic or ≥90 mm Hg diastolic.5
Under this definition, the prevalence of hypertension in the U.S. is astounding, affecting 30.8 percent of adults age 20 or older, which in 2015 amounted to 75 million Americans.6 Prevalence increases with age, impacting 64.9 percent of those age 60 and older, and is most common among African Americans.7
These statistics have been relatively stable since the early 2000s.
However, the 2017 American College of Cardiology/American Heart Association Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure (ACC/AHC) in Adults defined hypertension as ≥2 blood pressure readings in ≥2 settings with ≥120 mm Hg systolic or ≥80 mm Hg diastolic.4,8
In conflict with other internationally recognized standards, this lower threshold for diagnosis increases the prevalence of hypertension in American adults by 26.8 percent.4,8
Related: When to send your hypertensive patient to the ER
2017 guidelines criticized
The lowered thresholds for initiating management and treatment goals are based on lowering risk for future cardiovascular disease and the documented benefit of blood pressure reduction based on clinical trials.8
A more recent publication showed that patients had the same risk of cardiovascular disease regardless of threshold utilized, advocating an early start to therapy when indicated by the lower values.9
However, the lowered thresholds for classification and treatment have generated controversy among healthcare providers nationally and internationally with the criticism focused on the associated increased prevalence of hypertension, unnecessary treatment without perceived benefit, and subsequent cost to people and healthcare systems.1-4
On the other hand, the 2017 ACA/AHA Guidelines include 100 pages of useful points for the care of hypertensive patients, including methodologies, risk factors, etiologies, co-morbidities, and treatment strategies. Those aspects most applicable to optometry will be summarized here.8
Historically speaking, most practitioners recognize the blood pressure guidelines published by the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC), most recently updated in 2014.5
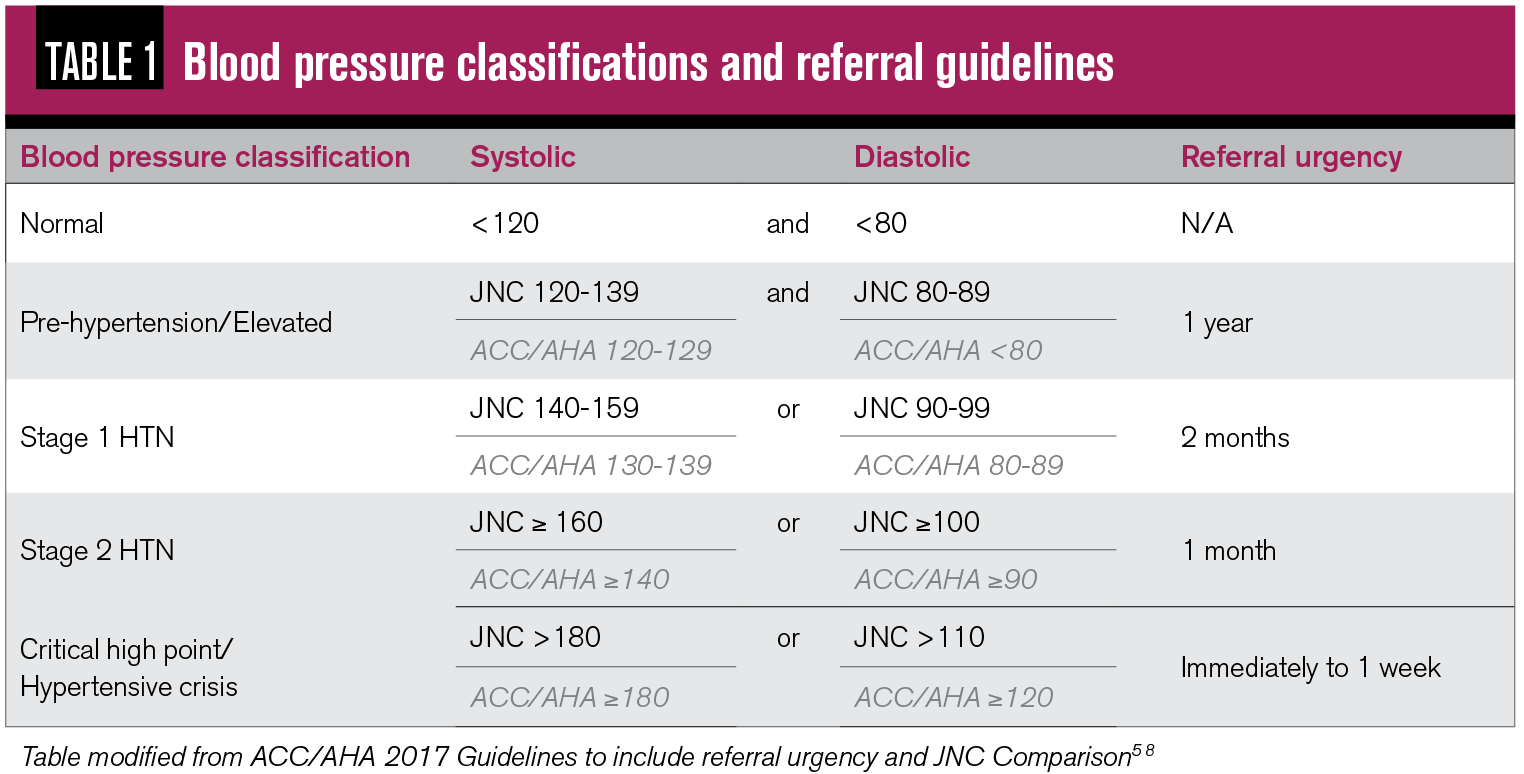
Table 1 illustrates JNC blood pressure classification and referral guidelines, with a comparison to the 2017 ACC/AHA guidelines (highlighted in gray). Generally speaking, most values are 10 mm Hg lower based on ACC/AHC.
See also: Nutrition in the future of primary-care optometry
One of the most notably positive aspects of the 2017 ACC/AHA Guidelines, which brought praise from the International Society of Hypertension and others in the healthcare community, was that its lower thresholds have the potential to increase awareness of hypertension as a chronic disease with significant risk of morbidity and mortality for those in the earlier stages of the disease. This awareness has the potential to cause preventive behavior, such as positive lifestyle modifications, before the disease progresses.
In addition, it emphasized the importance of considering risk factors when determining thresholds for treatment as well as treatment strategies. Risk factors including age >65, atherosclerosis or risk of developing it (e.g. high total cholesterol; smoking history), chronic kidney disease, and diabetes can be entered into an online risk calculator developed as a product of this publication.
The atherosclerotic cardiovascular disease (ASCVD) risk calculator can be accessed at this website or downloaded as a smartphone application.
Based on the results of the risk calculator for a patient’s 10-year risk of CVD, patients with blood pressure readings in different categories may be recommended for non-pharmacologic or pharmacologic therapy.
See also: Consider IOP fluctuations when diagnosing glaucoma
For example, a patient with blood pressure of 127/86 mm Hg with a low ASCVD 10-year risk (<10 percent) would be recommended strictly non-pharmacologic therapy, focusing on a healthy diet, exercise, and other positive lifestyle changes. A different patient with the same blood pressure but an ASCVD 10-year risk of >10 percent would be recommended pharmacologic therapy in addition to the lifestyle modifications. In fact, most adults who are classified as hypertensive under the 2017 ACC/AHA Guidelines, but not previously using JNC standards, would simply be managed with non-pharmacologic treatments.8
Proper blood pressure measurement
Accurate data is the first step to any medical decision-making process, and blood pressure readings are not an exception. The 2017 ACC/AHA Guidelines emphasized the importance of technique in obtaining accurate blood pressure readings, and possible sources of error.
Key steps:
- The patient should be seated and relaxed for five to 10 minutes prior to taking measurement
- The proper sized cuff should be chosen for the patient’s arm in order to avoid over- (if the cuff is too large) or under-estimation (if the cuff is too small) of actual reading
- The patient should have unrestricted bearing of the upper arm
- The patient should be seated with legs uncrossed and with back against a chair or wall
- The patient should have a slightly bent arm with palm up so the midpoint of the upper arm is resting at right atrium level. If the arm is above heart level, the reading will be underestimated. Due to gravitational forces, if the arm is held below heart level, the reading will be overestimated
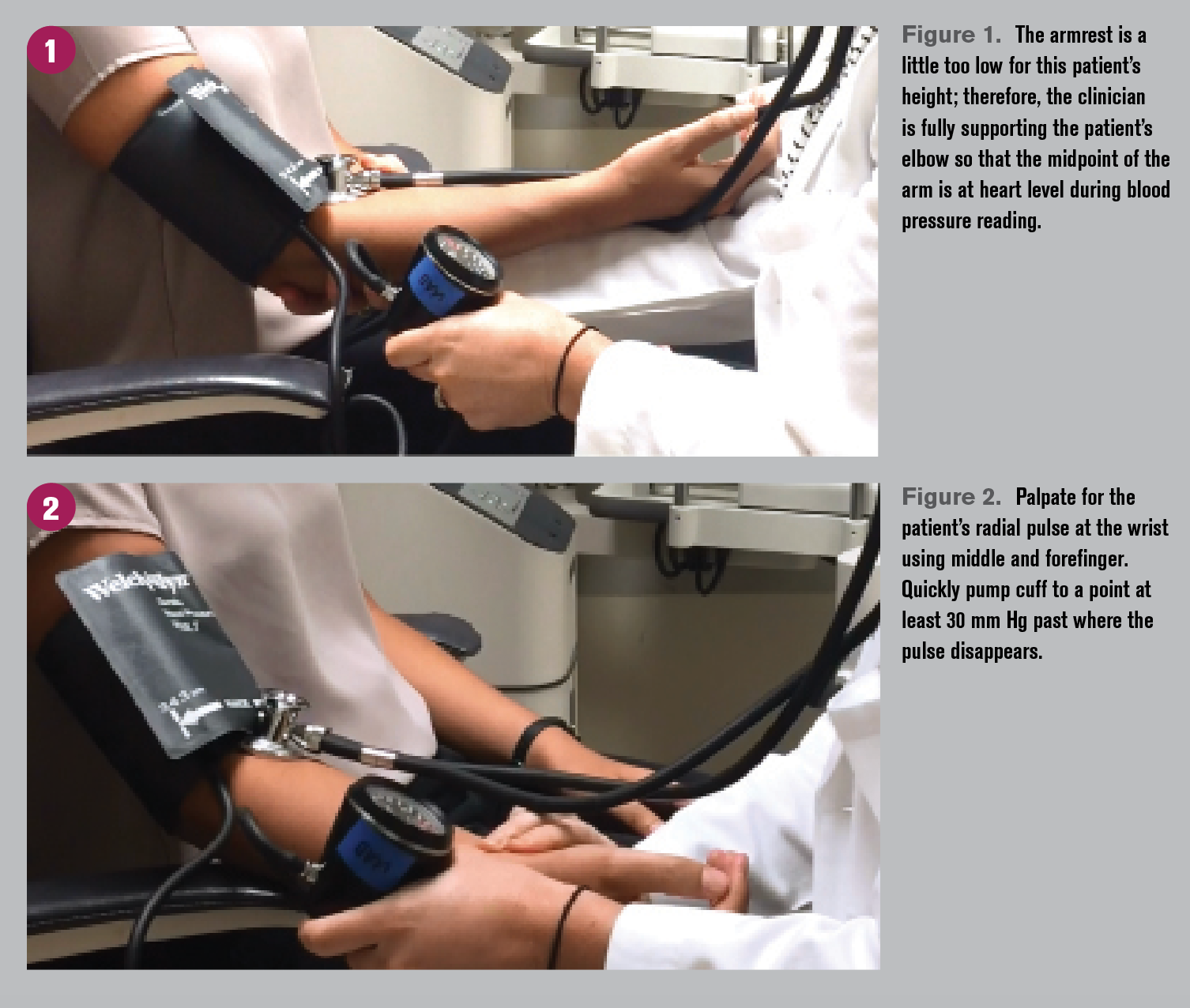
- The patient’s arm is rested on a table or an armrest, or it can be fully supported by the clinician (see Figure 1) if needed. No exertion should be present in order to prevent muscle contractions, which could artificially increase the reading.
- The clinician should palpate for the radial pulse (Figure 2), then pump the cuff quickly to the point where this pulse first disappears. The clinician should then continue to pump for an additional 30 mm Hg before slowly deflating the cuff at a rate of 2 to 3 mm Hg/second and listening for the first sound.
Pumping at least 30 mm Hg past the disappearance of the radial pulse will help to avoid the auscultatory gap, a period of diminished Korotkoff sounds during manual measurement and can prevent a gross underestimation of systolic blood pressure. This period of inaudible sounds impacting approximately 20 percent of patients can be up to 20 mm Hg long and is most common with increased arterial wall stiffness, such as those patients with chronic hypertension.
Automated blood pressure cuffs offer a quick and fairly accurate alternative to manual blood pressure for screening and can be easily taught to technicians. Accuracy is known to be a concern in extreme high and low ranges, so manual blood pressure can be used to repeat readings in these cases. For best results, patients using wrist cuffs should be asked to brace their tested wrist against the chest at heart level.
Handling a hypertensive crisis
One of the most important situations for which optometrists need accurate and the most up-to-date guidance is when a patient’s blood pressure is extremely high, obligating the practitioner to act quickly and with confidence.
Related: Keep an eye on link between glaucoma and blood pressure
The guidelines tell us that when a blood pressure is above the critical high point, defined by JNC as >180 mm Hg systolic or >110 mm Hg diastolic (note that ACC/AHA defines the diastolic as >120 mm Hg, interestingly enough), there is potential for a hypertensive crisis, which is a true medical emergency.
What differentiates the urgency from the emergency in these scenarios is evidence of end-organ damage, which most often occurs when the blood pressure has rapidly increased beyond the range within which the body’s auto-regulation system can adapt.
Optic disc and/or macular edema are examples of severe hypertensive retinopathy which do represent end-organ damage, making the eye exam key in the decision-making process. Evaluating these structures before sending the patients along is crucial.
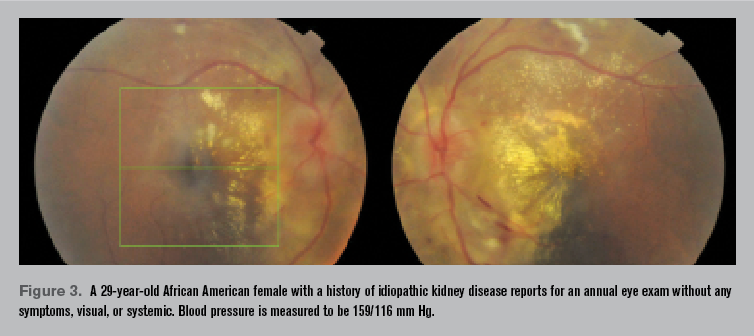
A patient with blood pressure of 159/116 mm Hg and notable optic disc as well as macular edema, as noted in Figure 3, for example, is treated as an emergency. A patient with the same blood pressure but the absence of disc edema can be treated urgently, referring within one week.
Related: Why Hollenhorst plaques can be key to carotid disease diagnosis
These referral decisions can be intimidating and based on many other factors, such as systemic symptoms (e.g. headache, malaise) as well as primary-care doctor recommendations.
There may be special considerations for the remainder of the eye exam after the blood pressure is known to be markedly elevated.
For example, ODs have a choice of a variety of dilation agents and in some cases the option of non-mydriatic or wide-field photographs instead. While 2.5% phenylephrine is considered safe and has not to date been noted to increase heart rate or blood pressure, it is likely not necessary for adequate dilation to examine the posterior pole. Phenylephrine 10%, on the other hand, should be avoided as even the slightest increase to heart rate or blood pressure can be life-threatening to patients in this vulnerable vascular state.10
Nasolacrimal occlusion can also be utilized to minimize systemic absorption of topical vasoconstrictors, when necessary.
Why a hypertensive crisis
Under normal blood pressure ranges, the autonomic nervous system’s auto-regulation helps to control retinal blood flow. However, it operates within a certain range, beyond which the system breaks down and vessels are no longer protected.
Typically optic disc and macular edema are caused by a very rapid increase in blood pressure to a point beyond this range, allowing for fluid and exudative material to escape outside of the vasculature.
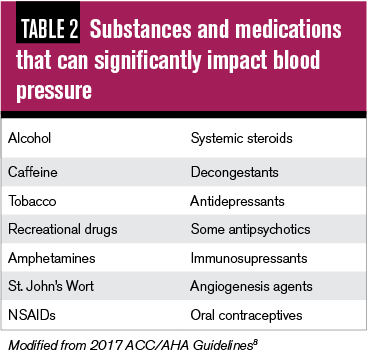
Most patients who experience a hypertensive crisis have a known history of hypertension but have had a recent change in medication, have problems with compliance, or may be having a drug interaction with a recent additional medication, such those listed in Table 2.
Unfortunately, these hypertensive events are strongly associated with mortality, with a one-year death rate of greater than 79 percent.8 Median survival of these patients is 10.4 months if the emergency is left untreated, which highlights the need for ODs to be on the lookout and to manage appropriately.
Optometry’s role
Optometry’s role continues to be recognition, accurate results, and timely referrals.
Part of discussions with patients suffering from hypertension, or those with elevated blood pressure, should always include education. Hypertensive retinopathy is second only to diabetic retinopathy, and while it does not as likely lead directly to vision loss, it is equally associated with systemic morbidity and mortality.11 Hypertension was a primary or contributing cause of more than 360,000 deaths in the U.S. in 2013, with stroke, heart attack, and kidney disease being the most common morbidities.12 These points tend to hit home when we relate them to vision.
Known hypertensives should also be encouraged to perform home monitoring of blood pressure because we now know that this is a crucial behavior for success stories in hypertension compliance.
Automated cuffs and other devices can be used at home to not only create daily modifications to behavior on the part of the patient but also to establish a record of data for the provider treating the disease and can reduce inaccuracies related to office-induced hypertension (ie. “white coat” hypertension).13,14
Measuring blood pressure in-office is quick, easy, and has the potential to influence a patient’s health in many ways.
Related: Know what common glaucoma mistakes to avoid
References:
1. Wilt TJ, Kansagara D, Qaseem A, Clinical Guidelines Committee of the American College of Physicians. Hypertension limbo: balancing benefits, harms, and patient preferences before we lower the bar on blood pressure. Ann Intern Med. 2018 Mar 6;168(5):369-370.
2. Crawford C. AAFP decides to not endorse AHA/ACC hypertension guideline: academy continues to endorse JNC8 guideline. American Academy of Family Physicians. Available at: https://www.aafp.org/news/health-of-the-public/20171212notendorseaha-accgdlne.html. Accessed 12/4/19.
3. Harmeet SR, Grover A, Hungin APS. Ambiguities in the guidelines for the management of arterial hypertension: Indian perspective with a call for global harmonization. Curr Hypertens Rep. 2017 Feb;19(2):17.
4. Khera R, Lu Y, Lu J, Saxena A, Nasir K, Jiang L, Krumholz HM.Impact of 2017 ACC/AHA guidelines on prevalence of hypertension and eligibility for antihypertensive treatment in United States and China: nationally representative cross sectional study. BMJ. 2018 Jul 11;362:k2357.
5. James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT Jr, Narva AS, Ortiz E. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) on Detection, Evaluation, and Treatment of High Blood Pressure. JAMA. 2014 Feb 5;311(5):507-20.
6. National Center for Health Statistics. Health, United States, 2015: With Special Feature on Racial and Ethnic Health Disparities. Hyattsville, MD. National Center for Health Statistics (US). 2016. May. Report No 2016-1232.
7. CDC/NCHS, National Health and Nutrition Examination Survey (NHANES). Available at: www.cdc.gov/nchs/nhanes/index . Accessed 12/4/19.
8. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr .2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection Evaluation and Management of High Blood Pressure in Adults. A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018 Oct 23;138(17):e426-e483.
9. Flint AC, Conell C, Ren X, Banki NM, Chan SL, Rao VA, Melles RB, Bhatt DL. Effect of Systolic and Diastolic Blood Pressure on Cardiovascular Outcomes. N Engl J Med. 2019 Jul 18;381(3):243-251
10. Stavert B, McGuinness MB, Harper CA, Guymer RH, Finger RP. Cardiovascular Adverse Effects of Phenylephrine Eyedrops: A Systematic Review and Meta-analysis. JAMA Ophthalmol. 2015 Jun;133(6):647-52.
11. Venkatramani J, Mitchell P. Ocular and systemic causes of retinopathy in patients without diabetes mellitus. BMJ. 2004;328(7440):625–629.
12. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Després JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2015 update: a report from the American Heart Association. Circulation. 2015 Jan 27;131(4):e29-322.
13. Wohlfahrt P, CÃfková R, Movsisyan N, Kunzová Å , LeÅ¡ovský J, Homolka M, SoÅ¡ka V, Bauerová H, Lopez-Jimenez F, Sochor O. Threshold for diagnosing hypertension by automated office blood pressure using random sample population data. J Hypertens. 2016 Nov;34(11):2180-6.
14. Filipovský J, Seidlerová J, KratochvÃl Z, Karnosová P, Hronová M, Mayer O Jr. Automated compared to manual office blood pressure and to home blood pressure in hypertensive patient. Blood Press. 2016 Aug;25(4):228-34.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.