Managing the astigmatic patient with contact lenses
We can easily dispell the myth, “I can’t wear contact lenses because I have astigmatism.” Today’s lenses offer high quality visual options with excellent comfort and efficient empirical fitting.

In the last 10 years, the disparity between the percentage of patients wearing astigmatic correction in their glasses vs. their contact lenses has been nearly eliminated.1-4 Today, roughly 40 percent of patients are currently wearing astigmatic correction in their spectacles, and about 30 percent of contact lens wearers are also wearing astigmatic correction.5-7 The majority of the remaining 10 percent have low levels of cylinder less than 0.50 D to 0.75 D of cylinder and do not experience significant visual decline.8,9
These new statistics are a testament to the many and varied outstanding toric options available to improve vision and the advances in fitting techniques which optimize chair time.
• Masking cylinder has been shown to be ineffective.10
• Aspheric lenses do not improve vision.11
• Empirically ordering both gas permeable (GP) and soft torics is highly successful even in patients with moderate to high astigmatism.12
Related: 3 tips to upgrading astigmatic contact lens patients
• Orthokeratology is now available in toric for patients with moderate cylinder.13
• Hybrid lenses are also effective in the correction of regular astigmatism.14
• Scleral lenses for the normal cornea provide yet another option for those patients with significant astigmatism.15
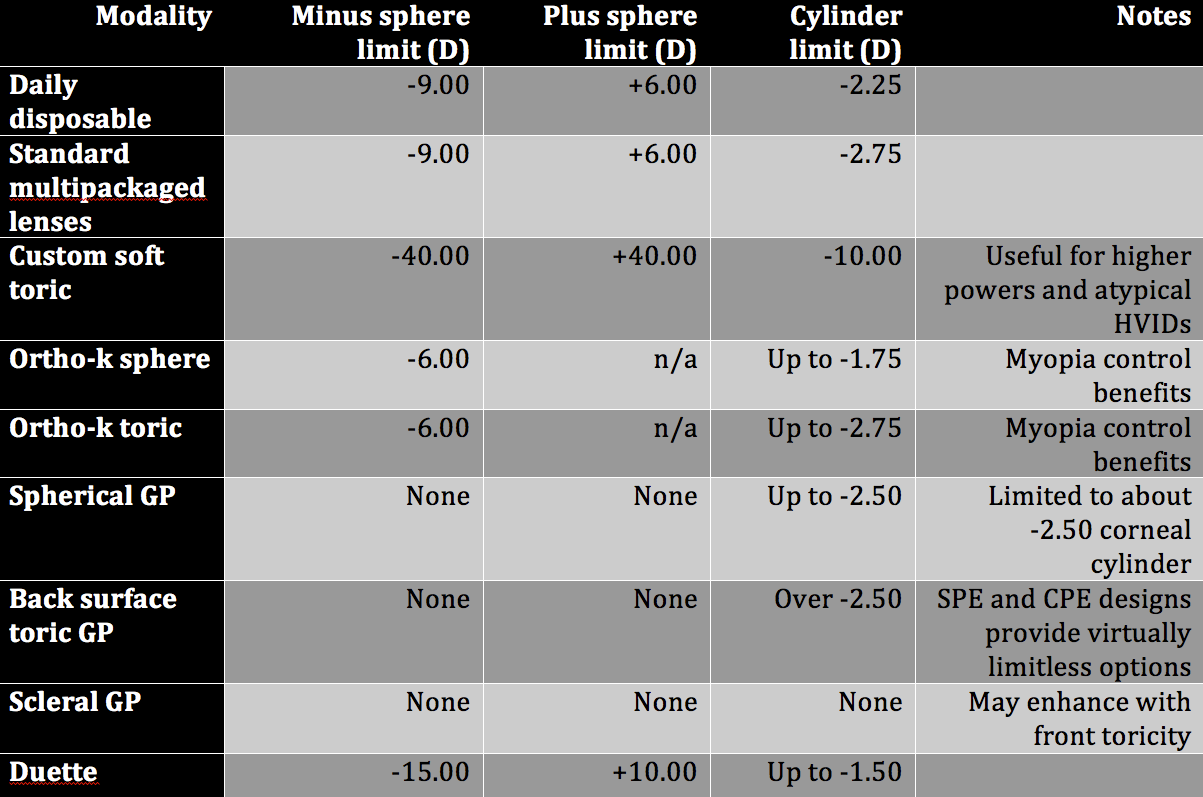
Table 1 demonstrates the diverse options now available for astigmatism correction in contact lenses.
Options for the low astigmat
Patients with cylinder between -0.75 and -1.75 are easily fit with daily or traditional multipackaged soft contact lenses16,17 in an extremely wide range of spherical power. The lenses are highly successful, and newer designs provide extremely stable fitting and vision.18
A recent study showed that patients wearing toric contact lenses had a better quality of life than patients who wore spherical lenses as determined by the NEI-RQL-42 survey.19 This study supported previous works that indicated nearly 92 percent of patients with a toric correction preferred their vision when they were fully corrected.9
Young children (ages 4-10 years) with toric correction adapt extremely well to rigid modalities.20 Young patients with low to moderate myopic astigmatic prescriptions can easily be corrected with orthokeratology (ortho-k), which provides the benefit of full correction of their prescriptions and myopia control.
For hyperopic astigmatism and those with higher amounts of myopia, spherical corneal GPs remain an outstanding option. The smaller overall diameter of corneal GPs can facilitate successful application and removal training due to the patient’s small eye. In addition, these lenses can be ordered empirically, allowing children to experience outstanding vision with their very first contact lens experience.
Related: Experts weigh in: What do you wish ODs knew about fitting torics?
Cost in these situations for spherical GP lenses on mildly toric corneas with mild to moderate refractive cylinder is significantly less in cost of goods.
GPs remain an outstanding vision correction option due to the precise optical quality generated.
For slightly older children, ortho-k may remain an outstanding option; however, cost and desire for disposability are attractive features of soft torics. Orthokeratology may also provide an alternative in adults who struggle with contact-lens–induced dry eye.
For most adults and teens, daily disposables and multipackaged lenses dominate the lens selections with their expansive array of parameters, outstanding comfort, and convenience.
Options for moderate-to-high astigmat
Soft toric lenses have been shown to be successful in low, moderate, and high astigmatism.17,18 With expanded parameters of daily disposable lenses ranging from -0.75 D to -2.25 D, very few patients have prescriptions outside of what is currently available. Multipackaged lenses expand the available parameters to -2.75 D cylinder. The latest designs offer multiple stabilization zones resulting in a lens that remains rotationally stable in primary as well as extreme gazes.
Toric ortho-k lenses are emerging in most marketplaces. These modified designs provide on average -2.50 DC correction while also offering myopia control for those with higher amounts of compound myopic astigmatism.13
When corneal cylinder exceeds -2.50 D, back-surface toric GPs become an outstanding option. Fitting them empirically is straightforward, efficient, and extremely successful.12 For smaller corneas, the saddle method of fitting the cornea 0.50 D steep in the flat meridian and 0.50 D flat in the steep meridian is highly effective. For average and large corneas, the Mandell-Moore method of fitting the flat meridian 0.25 D flat and the steep meridian flatter than K on a sliding scale as the cylinder increases is equally successful. Find an online calculator tool at http://www.gpli.info/mandell-moore/ to aid in designing your initial bitoric lenses.
These patients achieve excellent vision which may be superior to that of soft lenses. In fact, a study by Michaud showed that 4/10 current soft toric lens wearers chose to wear toric GPs for improved vision.12 This dispels the myth that a previous soft lens wearer will not adapt to corneal GPs.
Related: Considering scleral lenses for astigmatic patients
When patients have struggled with standard multipackaged soft lenses and GP options, it may be time to consider custom soft lenses, hybrids, and scleral lenses. Some patients with atypical corneal diameters may experience more stable fitting and vision with a custom soft lens with a custom diameter. Additionally, new designs offer lens powers that are nearly limitless in sphere and extend to -10.00 D in cylinder.
For patients who have struggled with vision stability with soft lenses and do not tolerate corneal GPs, SynergEyes Duette hybrid is an excellent option. Duette has been shown to offer excellent astigmatic correction when corneal cylinder and refractive cylinder are similar.14
In addition, the development of scleral lenses for the regular cornea offer virtually limitless power options and high-quality vision correction. Newer regular cornea scleral GPs are similar in size to soft lenses and can be designed with toric peripheries or haptics to stabilize lens rotation as well as front toric optics to correct any residual astigmatism for patients with high astigmatic corrections.15,21
There are now as many options for the astigmatic patients as there are for the spherical patient.
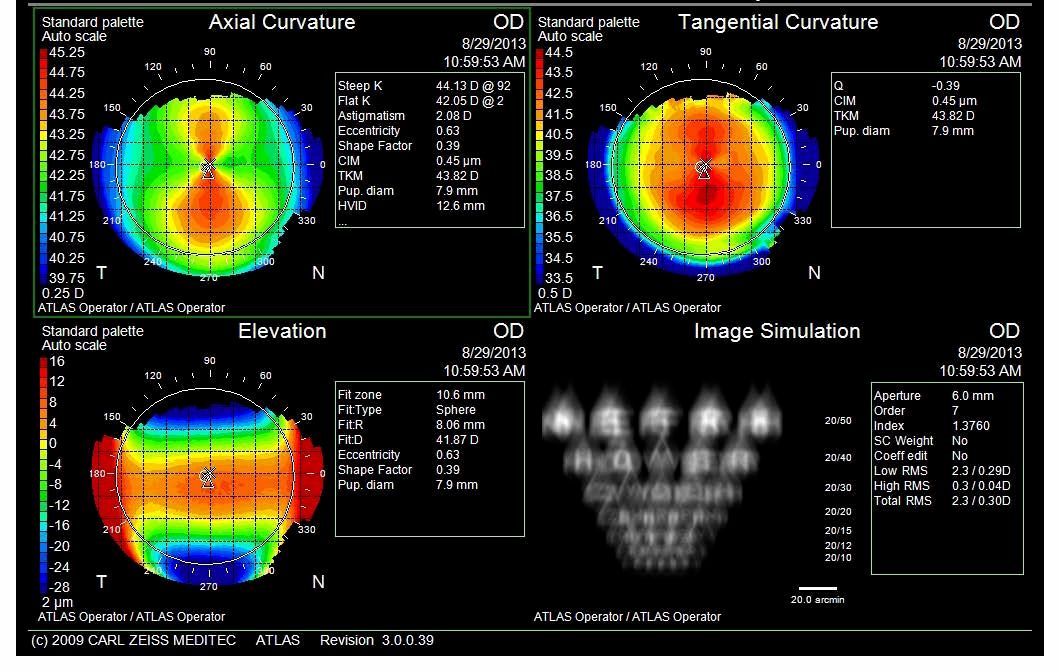
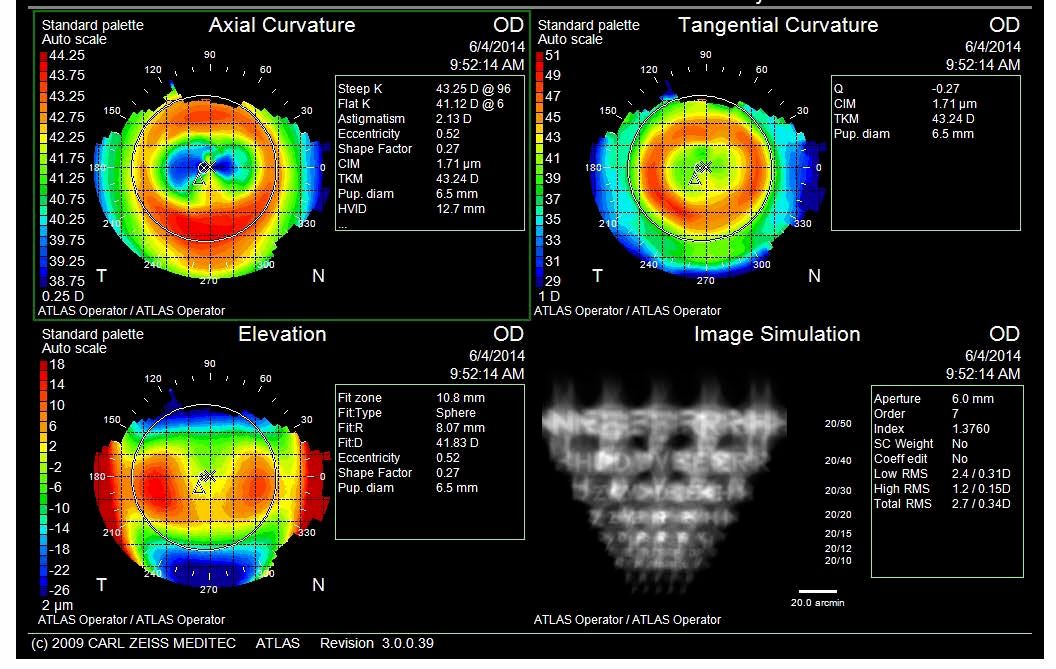
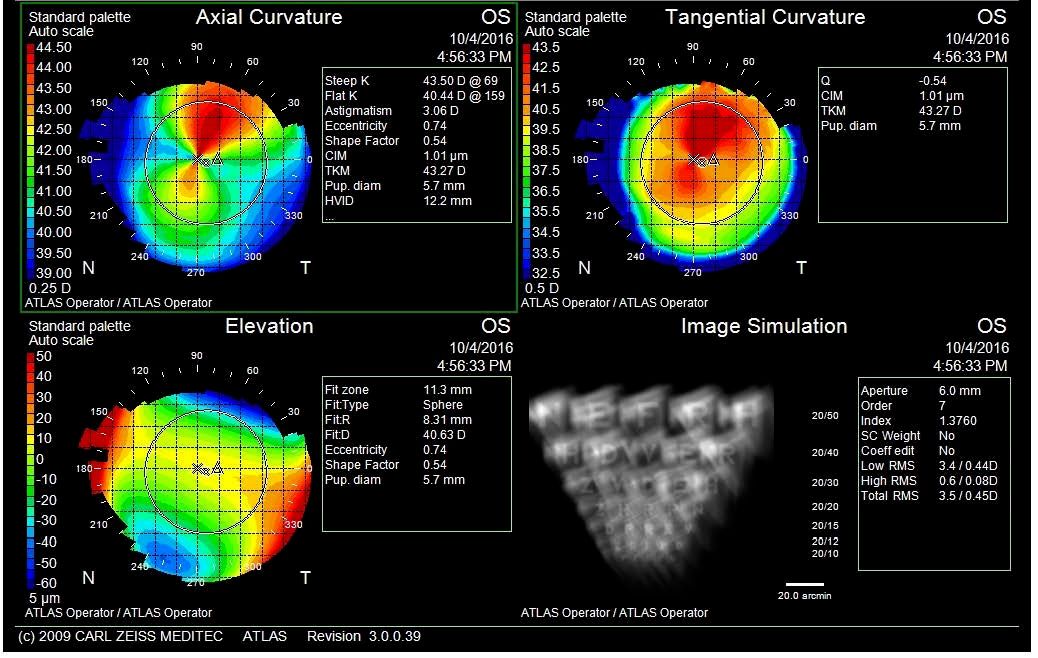
Figures 1 (top) and 2 (bottom). Pretreatment topographies showing significant with-the-rule (WTR) astigmatism.
Case 1
9-year-old female
The patient’s mother is very concerned about myopic progression in her daughter. The patient has increased from -2.75 D to -4.00 D in a year. However, she also has -2.25 D cylinder.
Related: Top toric contact lens fitting tips from the experts
After discussing options of soft toric, GP or ortho-k, the parent opted for ortho-k for multiple reasons including myopia control, gymnastics, and swimming. The parent strongly preferred no lens wear for sports. Topographies were sent electronically to the manufacturer along with spectacle prescription, and lenses with enhanced toric peripheries were designed. Spherical ortho-k lenses were ordered empirically.
SRx:
OD: -4.00-2.25 x 007; 20/20 ; SimKs 42.05/44.13
OS: -3.00-2.25 x 178; 20/20; SimKs 41.88/44.08
See Figures 1 and 2.

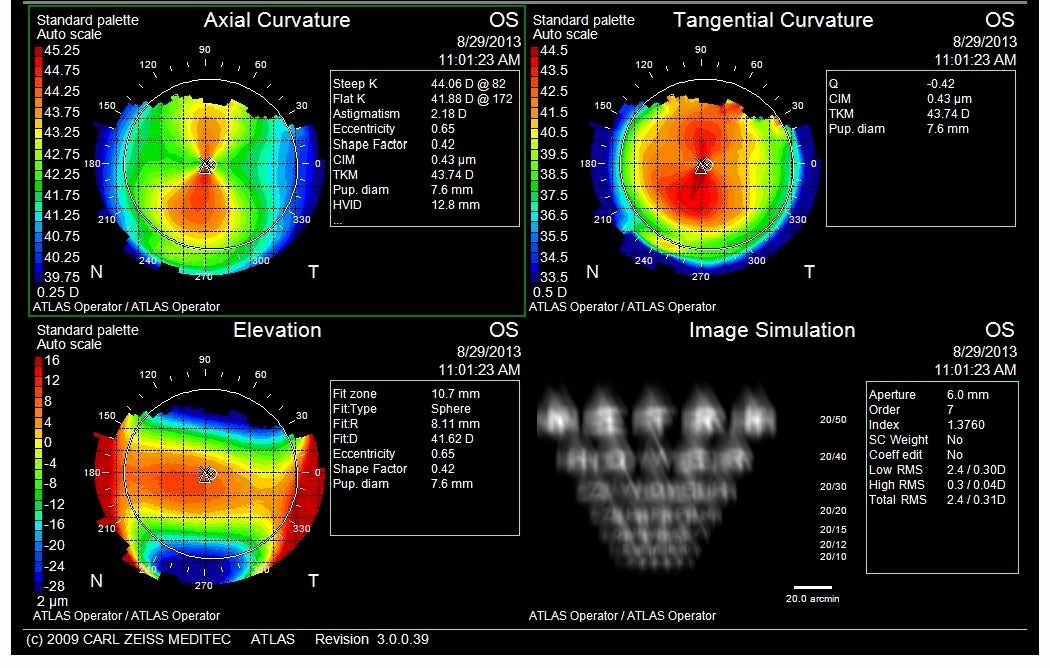
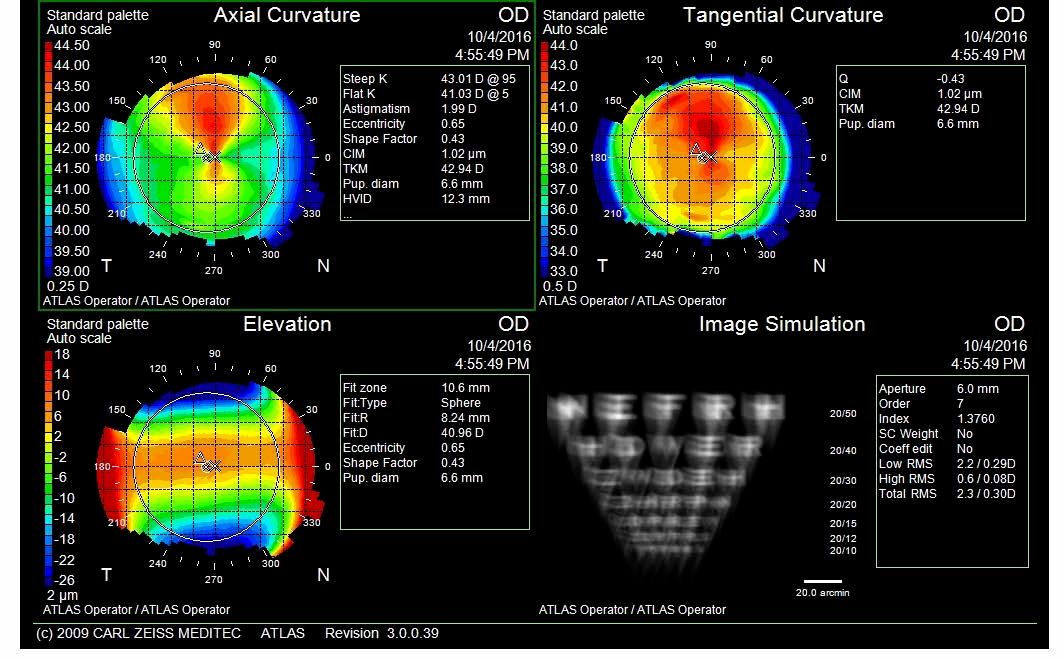
Figures 3 (top) and 4 (bottom). Classic ortho-k bulls eye patterns.
The lenses provided very centered treatment zones. See Figures 3 and 4.
At one year, the vision remained 20/25 unaided with a -0.25 DS refraction to 20/20 in each eye. See Figures 5 and 6 for post-treatment topographies.
Figures 5 (top) and 6 (bottom). Post treatment topographies.
Case 2
12-year-old male
The child has broken multiple pairs of glasses and refuses to wear them. His mother is concerned that he will lose contact lenses and wants him to have something disposable so he will have spares.
SRx:
OD: +2.75-2.75 x 020; 20/40; SimKs 43.20/46.25
OS: +2.75-4.25 x 160; 20/40; Sim Ks 42.47/46.21
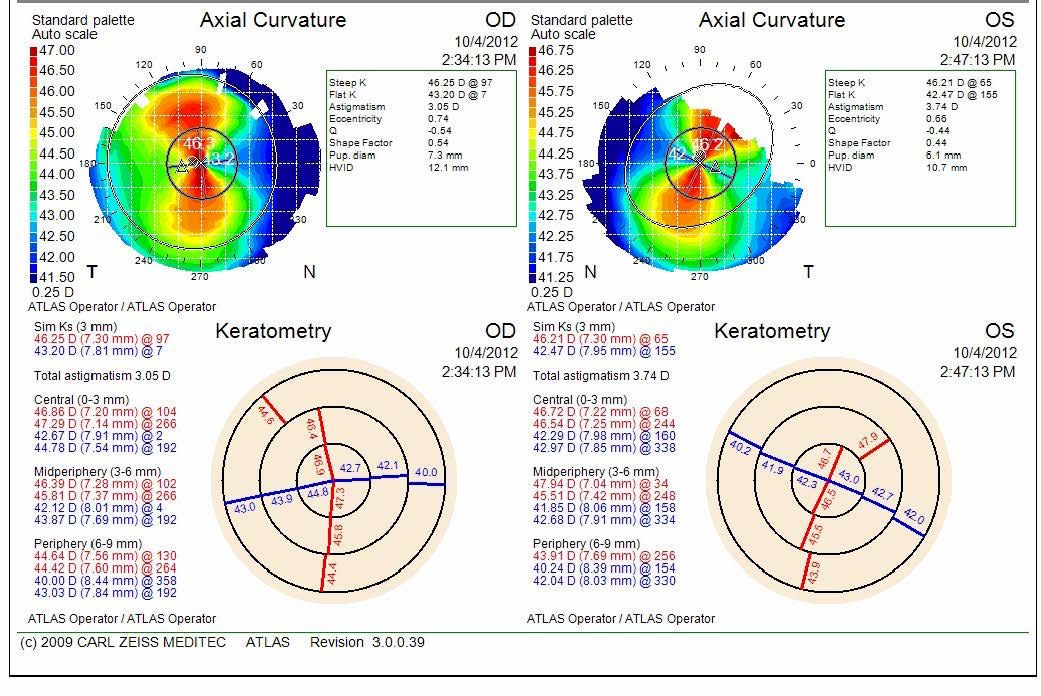
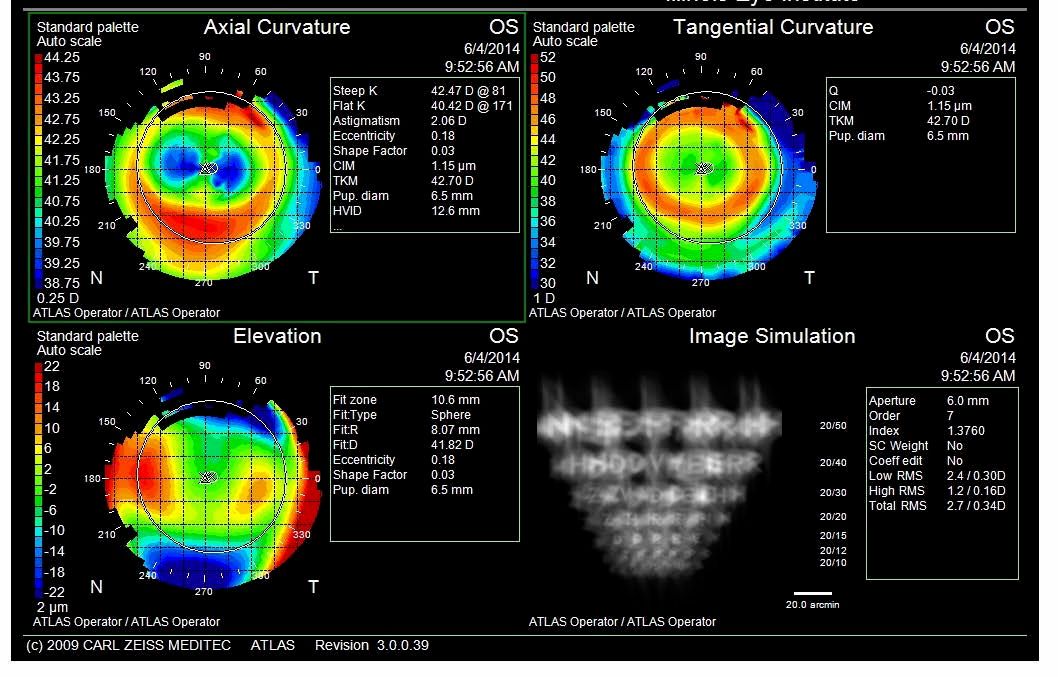
Figure 7. OD and OS topographies showing high regular astigmatism.
See Figure 7 for topographies.
I prescribed custom soft toric monthly replacement contact lenses.
Related: Managing astigmats when they hit presybopia
OD: +3.25-3.25 x 010; 8.7 mm base curve; 14.5 mm diameter; 20/25
OS: +3.00-3.75 x 165; 8.7 mm base curve; 14.5 mm diameter; 20/30
The patient very successful with application and removal. At the six-month follow-up visit, his parent reports improved academic success.
Figures 8 (top) and 9 (bottom). High slightly asymmetric astigmatism OD and OS.
Case 3
8-year-old female
Parents report that the patient does not wear her spectacles, and they would like her to try contact lenses.
SRx:
OD: +0.50-2.50x010; 20/20; SimKs 41.03/43.07
OS: +1.25-2.75x163; 20/30; SimKs 40.44/43.50
Bitoric GPs were designed using a saddle technique and ordered based on an over-refraction on Pl/-3.00; 41.00/43.00; 9.2 mm diagnostic lenses.
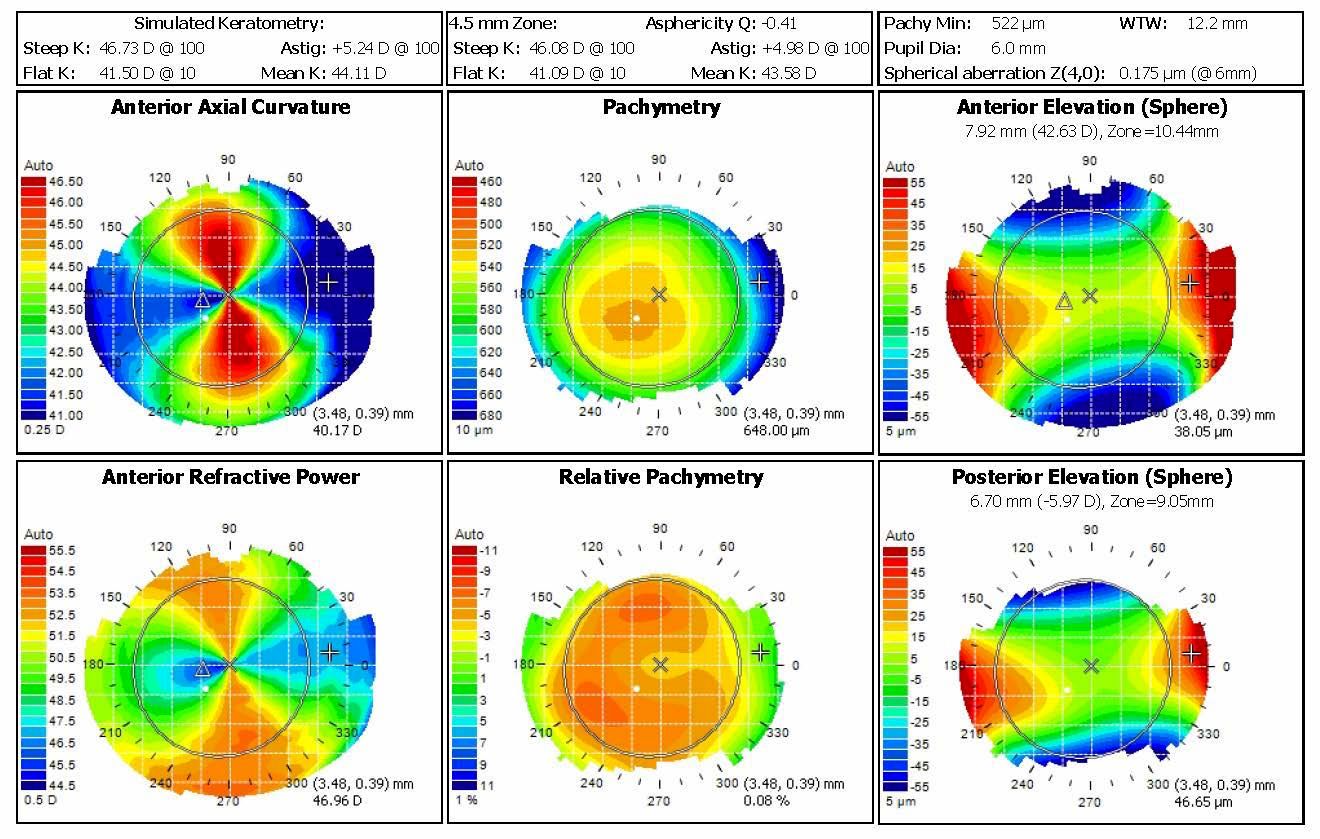
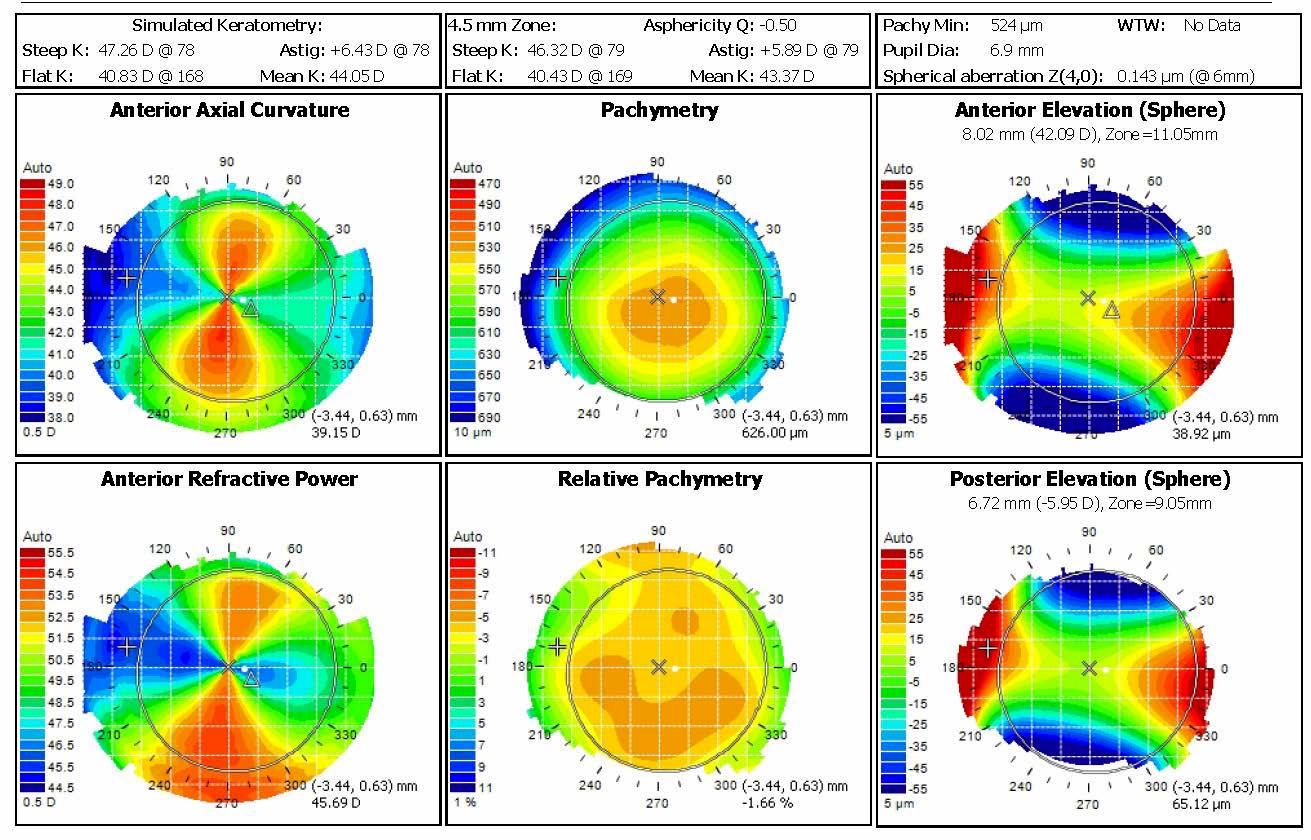
Figures 10 (top) and 11 (bottom). Very high regular astigmatism with no evidence of ectasia.
Final lenses were:
OD: -0.25/-2.25; 41.00/43.00; 9.0 mm; 20/20
OS: -0.50/-2.50; 41.00/43.00; 9.0 mm; 20/25
Related: 5 reasons ODs don’t fit toric contact lenses
The child and parents were successful with application and removal. The patient wore lenses for school with good success.
Case 4
8-year-old female
This patient was referred from the pediatrics department for a contact lens fitting. Pediatrics’ goals were to maximize her vision so she will be more successful with vision therapy for an intermittent left exotropia.
SRx:
OD: -1.75-6.50 x 005; 20/30; Manual Ks 41.75/46.75
OS: -1.00-8.50 x 180; 20/50; Manual Ks 40.75/47.75
Initially she was fit with bitoric corneal GPs which provided excellent vision; however, she struggled with redness and irritation.
Initial bitoric corneal GPs:
OD: -2.00/-6.00; 41.50/45.75; 8.8 mm; 20/25
OS: -2.00/-6.00; 41.50/46.75; 8.8 mm; 20/40
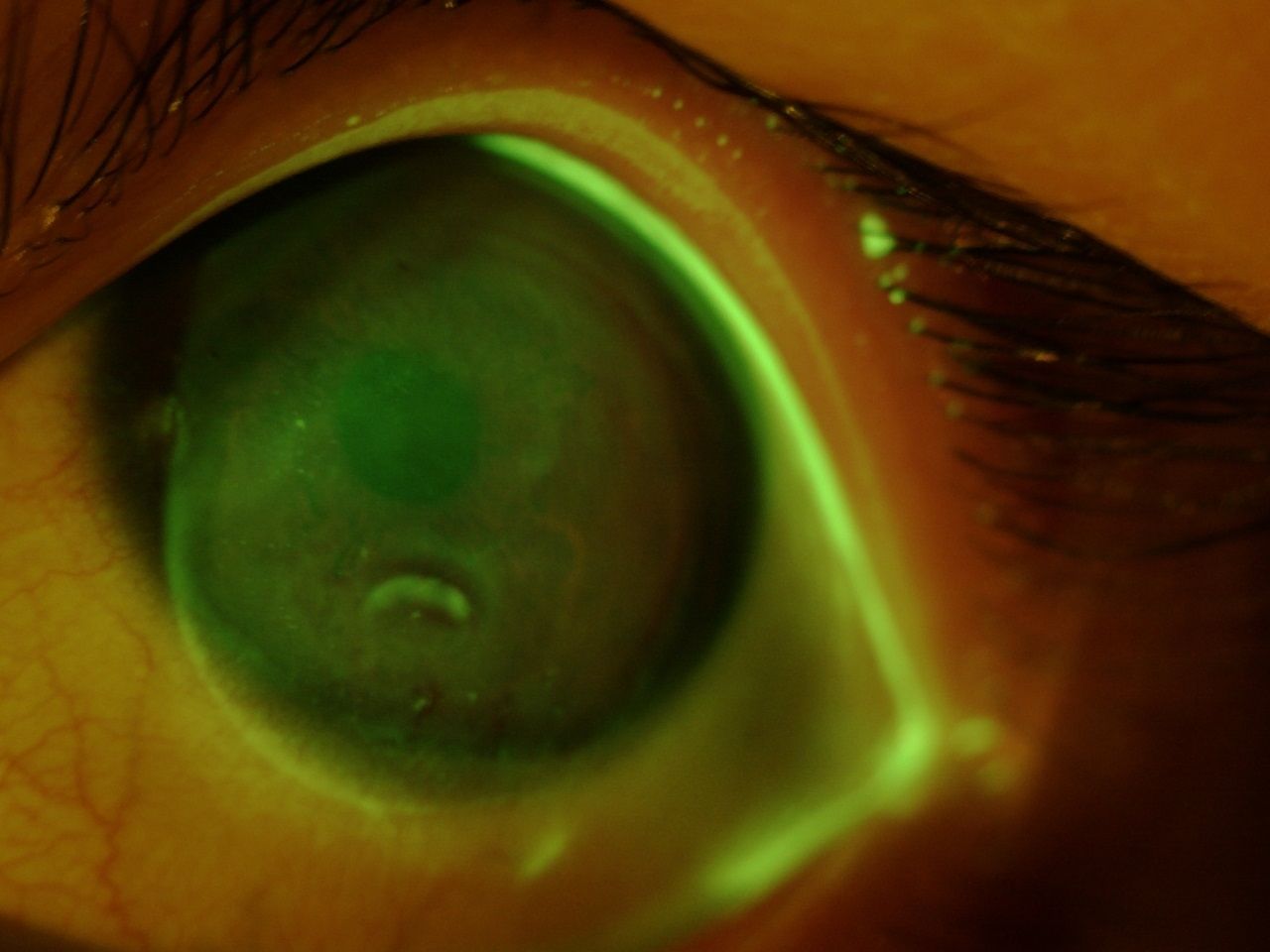
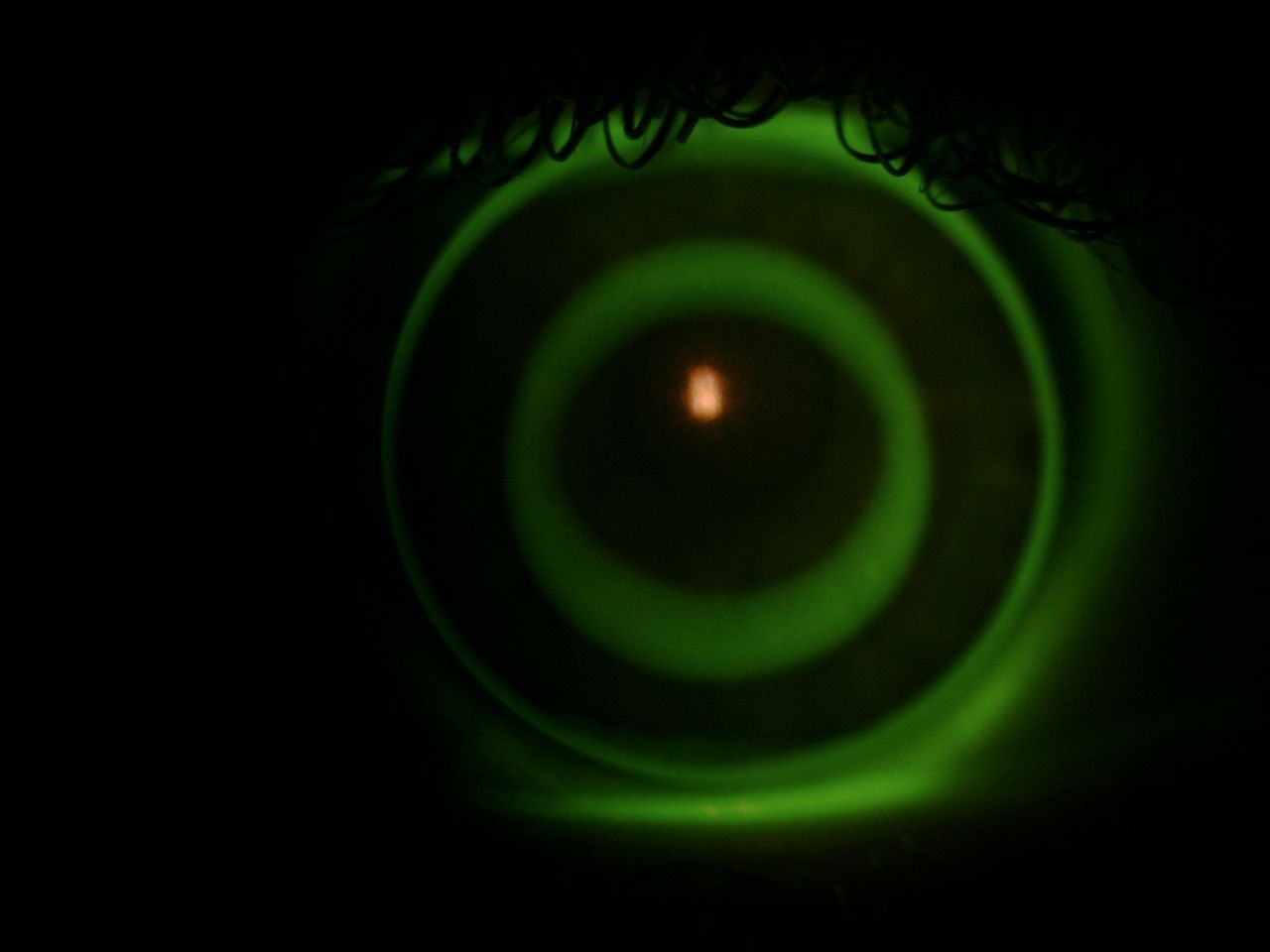
Figure 12. Prominent impression of the lens and punctate stain upon removal of bitoric GP.
Unfortunately, upon follow-up, the lenses became adherent (See Figure 12). Therefore, she was refit into scleral lenses. Her staining resolved, and she was able to wear the sclerals throughout the school day.
Final scleral GPs:
OD: -5.50; 7.40 mm; 14.3 mm flat edge; 20/25
OS: -4.50; 7.40 mm; 14.3 mm flat edge; 20/25
Related: Educate your patients about astigmatism
After vision therapy and a year in the sclerals, best corrected vision improved to 20/20 and 20/25, and her left eye no longer tropes.
Case 5
36-year-old male
The patient presents to the clinic with a desire to improve his vision in his left eye. He is currently wearing spectacles:
OD: -0.50-2.50 x 180; 20/20
OS: +2.00-4.00 x 180; 20/200
Updated refraction:
OD: -1.50-2.50 x 180; 20/20; SimKs 40.00/43.10
OS: -1.75-6.50 x 175; 20/30; SimKs 40.70/45.30
Cycloplegic evaluation revealed a left prescription of +6.00-7.50 x 170. However, with the full prescription, the patient experienced diplopia at near and OS suppression at distance. Therefore, he was fit with bitoric lenses in hopes of improving his vision, equalizing image size and eliminating diplopia (see Figures 13 and 14).
Figures 13 (top) and 14 (bottom). High regular astigmatism visible on topography with corneal thinning but no posterior ectasia.
An initial pair of diagnostic lenses were applied based upon Mandell-Moore, and after over-refraction the following corneal GPs were ordered:
OD: -0.75/-2.25; 41.00/43.00; 9.2 mm; 20/20
OS: +5.50 back toric; 39.50/44.75; 9.2 mm; 20/25
The diplopia resolved with the new lenses, and the patient reported increased driving confidence, especially at night.
Conclusion
All of these patients experienced vision improvement when they were fit with contact lenses to correct their astigmatism. Based on the patient’s needs, each needed a different type of lens.
For myopia control, toric ortho-k was helpful for Case 1. For his active lifestyle, soft torics provided a better option for Case 2. For Case 3, a scleral was needed to provide appropriate ocular health and vision correction. And for Cases 4 and 5, GP torics optimized vision.
Related: Upgrade your patients to new technology
We can easily dispell the myth, “I can’t wear contact lenses because I have astigmatism.” Today’s lenses offer high quality visual options with excellent comfort and efficient empirical fitting.
References
1. Morgan PB, Efron N. A decade of contact lens prescribing trends in the United Kingdom (1996-2005). Cont Lens Anterior Eye. 2006 May;29(2):59-68.
2. Woods CA, Jones DA, Jones LW, Morgan PB. A seven year survey of the contact lens prescribing habits of Canadian optometrists. Optom Vis Sci. 2007 Jun;84(6):505-10.
3. Morgan PB, Efron N. Prescribing soft contact lenses for astigmatism. Cont Lens Anterior Eye. 2009 Apr;32(2):97-8.
4. Young G, Sulley A, Hunt C. Prevalence of astigmatism in relation to soft contact lens fitting. Eye Contact Lens. 2011 Jan;37(1):20-5.
5. Efron N, Morgan PB, Helland M, Itoi M, Jones D, et al. Soft toric contact lens prescribing in different countries. Cont Lens Anterior Eye. 2011 Feb;34(1):36-8.
6. Morgan PB, Efron N, Woods CA, International Contact Lens Prescribing Survey Consortium. An international survey of toric contact lens prescribing. Eye Contact Lens. 2013 Mar;39(2):132-7.
7. Efron N, Nichols JJ, Woods CA, Morgan PB. Trends in US Contact Lens Prescribing 2002 to 2014. Optom Vis Sci. 2015 Jul;92(7):758-67.
8. Villegas EA, Alcón E, Artal P. Minimum amount of astigmatism that should be corrected. J Cataract Refract Surg. 2014 Jan;40(1):13-9.
9. Gao J, Wang XX, Wang L, Sun Y, Liu RF, Zhao Q. The Effect of the Degree of Astigmatism on Optical Quality in Children. J Ophthalmol. 2017:5786265.
10. Snyder C, Talley DK. Masking of astigmatism with selected spherical soft contact lenses. J Am Optom Assoc. 1989 Oct;60(10):728-31.
11. Morgan PB, Efron SE, Efron N, Hill EA. Inefficacy of aspheric soft contact lenses for the correction of low levels of astigmatism. Optom Vis Sci. 2005 Sep;82(9): 823-828.
12. Michaud L, Barriault C, Dionne A, Karwatsky P. Empirical fitting of soft or rigid gas-permeable contact lenses for the correction of moderate to severe refractive astigmatism: a comparative study. Optometry. 2009 Jul;80(7):375-83.
13. Lyu B, Hwang KY, Kim SY, Kim SY, Na KS. Effectiveness of Toric Orthokeratology in the Treatment of Patients with Combined Myopia and Astigmatism. Korean J Ophthalmol. 2016 Dec;30(6):434-442.
14. Abou Samra WA, El-Emam DS, Kasem MA. Clinical Performance of a Spherical Hybrid Lens Design in High Regular Astigmatism. Eye Contact Lens. 2016 Sep 22. DOI 10.1097/ICL.0000000000000326
15. Michaud L, Bennett ES, Woo SL, Reeder R, Morgan BW, Dinardo A, Harthan JS. Clinical Evaluation of Large Diameter Rigid Gas Permeable Versus Soft Toric Contact Lenses for the Correction of Refractive Astigmatism A MultiCenter Study. Eye Contact Lens. 2016 Nov 24. DOI 10.1097/ICL.0000000000000323.
16. Moody KJ, Hickson-Curran S. Fitting low astigmats with a soft contact lens. Cont Lens Spectrum. 2001 Nov; 34-42.
17. Richdale K, Berntsen DA, Mack CJ, Merchea MM, Barr JT. Visual acuity with spherical and toric soft contact lenses in low- to moderate-astigmatic eyes. Optom Vis Sci. 2007 Oct;84(10):969-75.
18. Momeni-Moghaddam H, Naroo SA, Askarizadeh F, Tahmasebi F. Comparison of fitting stability of the different soft toric contact lenses. Cont Lens Anterior Eye. 2014 Oct;37(5):346-50.
19. Cox SM, Berntsen DA, Bickle KM, Mathew JH, Powell DR, Little BK, Lorenz KO, Nichols JJ. Efficacy of Toric Contact Lenses in Fitting and Patient- Reported Outcomes in Contact Lens Wearers. Eye Contact Lens. 2017 Sep 21: 1-4. DOI 10.1097/ICL.0000000000000418
20. Jones-Jordan LA, Walline JJ, Mutti DO, Rah MJ, Nichols KK, Nichols JJ, Zadnik K. Gas permeable and soft contact lens wear in children. Optom Vis Sci. 2010 Jun:87(6):414-420.
21. Visser ES, Visser R, Van Lier HJ. Advantages of toric scleral lenses. Optom Vis Sci. 2006 Apr;83(4):233-6.
Read more toric contact lens content by visiting our Toric Contact Lens Resource Center
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.