Reviewing pediatric primary care optometry
Primary care optometrists play a crucial role in the wellbeing of a child, often serving as the gatekeeper for the critical care of our youngest patients. After hours, these doctors must sift through a vast array of evidence-based literature to foster the insight required just to get through a day in the life.

Figure 1. Viral conjunctivitisPrimary care optometrists play a crucial role in the wellbeing of a child, often serving as the gatekeeper for the critical care of our youngest patients. After hours, these doctors must sift through a vast array of evidence-based literature to foster the insight required just to get through a day in the life. Strapped with the responsibility of treating a wide variety of common pediatric conditions that often require extra thought and/or patience, the primary care optometrist must also have the expertise to recognize rare but ominous signs and symptoms representing vision or even life-threatening conditions.

Figure 2. Transient ptosisMyopia
Myopia is one of the more common conditions in pediatric primary care optometry. The Correction of Myopia Evaluation Trial (COMET) study showed that average progression per year was approximately 0.50 D in elementary school-aged children with low to moderate initial myopia.1
Although progressive addition lenses were not shown in this study to provide a clinically meaningful control of such progression, the most recent literature suggests that distance-center, near-surround contact lenses may actually have a bigger impact on slowing down myopia.2-5
Binocular vision conditions
Binocular vision disorders are also commonly discovered by the astute primary care optometrist who performs cover test at both distance and near. In convergence insufficiency (CI), a larger exophoria exists at near compared to that at distance. Combined with a reduced near-point of convergence and low positive fusional vergences, patients with CI have a low accommodative convergence (AC/A), suggesting that lens therapy is not ideal. Because the angles are different at distance vs. near, prism is also not helpful in most cases.
The Convergence Insufficiency Treatment Trial showed that office-based vision therapy is a treatment option that is successful in a majority of cases and that the Convergence Insufficiency Symptom Scale may be a helpful tool in eliciting the severity of potential symptoms.6
In binocular conditions in which the AC/A is high (convergence excess, divergence excess), a 16 prism diopter esophoria at near quickly becomes ortho with the addition of +2.00 D at near when the AC/A is 8/1. Understanding how changes in refractive error correction modify accommodation, and therefore the phoria through the AC/A, is an important part of the primary care optometrist’s day.
Strabismus and amblyopia
Strabismus and amblyopia likely represent another constellation of conditions that the primary care optometrist must be armed to treat. The Amblyopia Treatment Studies conducted by the NEI through the Pediatric Eye Disease Investigator Group have significantly changed the way amblyopia is managed relative to years past.
With more than 27% of children aged 3 to 7 with anisometropic amblyopia achieving nearly equal visual acuity with glasses alone,7 the child with amblyopia is now treated using a step-wise approach.
Starting with glasses alone, a child can be seen every 5 to 8 weeks until a visual acuity plateau is reached (often in 4 months according to the ATS studies).
For those who don’t achieve 20/25 or better or maintain unequal visual acuities with best correction alone, the ATS studies have shown that adding only 2 hours per day of patching8 or 1 drop of atropine ophthalmic solution 1% (Akorn) every Saturday and Sunday is very often successful at improving the vision in the amblyopic eye in 3 to 7 year olds.9 F
or older children, the ATS studies have shown that treating the amblyopia with best full correction (maintaining the full anisometropia and cutting the plus symmetrically as needed) and penalization helps maximize visual acuity even in teenagers.10
For the youngest patients, the most common condition seen during an infant exam is, fortunately, a normal healthy child. Primary care optometrists can get important information when inquiring about the pregnancy and birth, including number of weeks gestation and birth weight. It is also important to identify normal development in infancy, including the “doggie stage” at roughly 6 months when children should begin to roll over, sit, and shake (or reach for an object).
At this time, children’s visual development includes normal pupils, strong and accurate accommodation, improving saccades, robust convergence and divergence, detectable color vision, and good stereoacuity that developes quickly at around 3.5 months. As infants age, visual acuity dramatically improves. By age 4, according to the MEPEDS study, a large majority of children can complete formal visual acuity testing.11
Those who have unequal visual acuities should be examined carefully for amblyogenic anisometropic refractive errors (1.00 D of hyperopia, 2.00 D of myopia, 1.50 D of astigmatism).12 In absence of amblyogenic refractive error, unequal acuities require continued work up to rule out strabismus, functional vision loss, or sight-threatening pediatric ocular diseases.
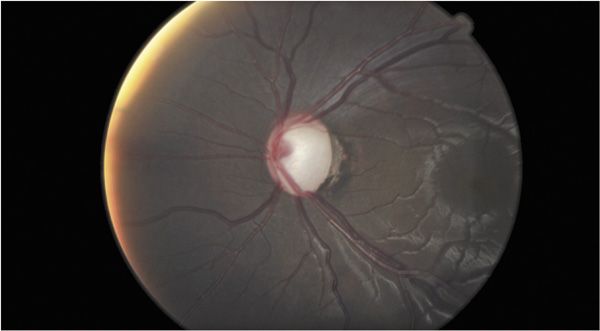
Figure 3. Pediatric glaucoma following observation of posterior embly otoxin/AxenfeldSight and life-threatening conditions
Although identifying the common but somewhat benign pediatric ocular condition is an important part of the primary care optometrist’s day, being able to identify conditions that may be sight or life threatening is crucial no matter how rare they may be.
Glaucoma is one such rare condition that requires immediate referral to a glaucoma specialist because infantile and pediatric glaucoma is rarely managed by therapeutic intervention alone, given that it is often a structural problem with the angle.
However, signs including a larger-than-normal cornea (9 to 10 mm in an infant; adult-size or 11 to 12 mm in a 3-year-old), cloudy cornea, posterior embryotoxin, excessive tearing, and myopia are all often first seen by the primary care optometrist in addition to the optic nerve appearance.
Cataracts represent another ominous condition in infancy requiring immediate referral as studies suggest that for maximum visual benefit, surgery to remove the lenses should occur by 6 weeks of age if unilateral13,14 and by 10 weeks of age if bilateral.15 Nystagmus in an infant may be the first sign of cataract in the child, or it can be congenital.
Congenital nystagmus generally has a null point, is latent (worsens when one eye is covered), and, importantly, remains horizontal in upgaze. Nystagmus that beats up in up gaze and beats down in down gaze generally requires a neurological referral.

Figure 4. OD blurred marginsOther conditions that may require neurological referral include Horner Syndrome in the absence of birth trauma because it may be the presenting sign of neuroblastoma in a child.16,17
Divergence insufficiency (presenting as more esophoria at distance relative to near with a low AC/A) is often due to decompensated phoria but may mimic a lateral rectus palsy (with abduction deficits) or divergence paralysis, which may also be the presenting sign of neurological compromise. Retinoblastoma, an amelanotic lesion in the posterior segment requires immediate referral and is most often identified between 1 and 3 years.18, 19

Figure 5. OS > OD blurred marginsA puffy lid in a child may represent another neurological referral if rhabdosarcoma is suspected.
More commonly, a compromised lid represents something that may be benign or require oral antibiotics. Whether for internal hordeolum or preseptal cellulitis, knowledge of FDA dosing guidelines is critical to the proper dosages for oral medications in children.
Because such guidelines are reported in kilograms, the primary care optometrist must convert the child’s weight from pounds to kilograms (1 kg = 2.2 lbs), then determine the desired dosage based on severity (e.g., 20 to 40 mg/kg/d) choose the route supplied (liquid, chewable tablet, or tablet), and avoid prescribing more than the adult dosage. Knowledge of allergies and cross-reactivity with other medications in addition to proper FDA-recommended dosing is critical in providing therapeutic intervention to our most vulnerable population.
Because such a broad spectrum of conditions exists and because the primary care optometrist must rely largely on objective data when examining a child, a dilated eye exam on all children even at the first visit often proves to be essential. For children 12 months old or younger, 0.5% cyclopentolate (Cyclogyl, Alcon) or 0.5% tropicamide (Mydriacyl, Alcon) may be used to reliably assess the child’s refractive error and ocular health.
For those older than 12 months, 1% cyclopentolate and/or 1% tropicamide may be used with or without 2.5% phenylephrine (Minims, Bausch + Lomb). Cyclopentolate is contraindicated in children who have had seizures, have CNS concerns, Down syndrome, and necrotizing enterocolitis, but tropicamide is often a safe alternative.
Through dilated eye exam and cycloplegic retinoscopy, the primary care optometrist can feel confident in the objective findings uncovered.
Whether rare and in your chair or common yet significant, the primary care optometrist can make a big impact on the life of a child-not bad for a day’s work.ODT
This is the fourth in a series of articles summarizing the Diplomate preparatory course by the Primary Care Section of the American Academy of Optometry.
References
1. Gwiazda J, Hyman L, Hussein M, et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children.Invest Ophthalmol Vis Sci. 2003 Apr;44(4):1492-500.
2. Walline JJ, Greiner KL, McVey ME, et al. Multifocal contact lens myopia control. Optom Vis Sci. 2013 Nov;90(11):1207-14.
3. Sankaridurg P, Chen X, Naduvilath T, et al. Adverse events during 2 years of daily wear of silicone hydrogels in children. Optom Vis Sci. 2013 Sep;90(9):961-9.
4. Berntsen DA, Kramer CE. Peripheral defocus with spherical and multifocal soft contact lenses.Optom Vis Sci. 2013 Nov;90(11):1215-24.
5. Walline JJ, Lindsley K, Vedula SS, et al. Interventions to slow progression of myopia in children.Cochrane Database Syst Rev. 2011 Dec 7;(12)
6. Mutti DO, Gwiazda J, Norton TT, et al. Myopia-yesterday, today, and tomorrow. Optom Vis Sci. 2013 Nov;90(11):1161-4.
7. Convergence Insufficiency Treatment Trial Study Group. Randomized clinical trial of treatments for symptomatic convergence insufficiency in children. Arch Ophthalmol. 2008 Oct;126(10):1336-49.
8. Cotter SA; Pediatric Eye Disease Investigator Group, Edwards AR, et al. Treatment of anisometropic amblyopia in children with refractive correction. Ophthalmology. 2006 Jun;113(6):895-903.
9. Repka MX, Beck RW, Holmes JM, et al. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol. 2003 May;121(5):603-11.
10. Repka MX, Cotter SA, Beck RW, et al. A randomized trial of atropine regimens for treatment of moderate amblyopia in children. Ophthalmology. 2004 Nov;111(11):2076-85.
11. Scheiman MM, Hertle RW, Beck RW, et al. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Arch Ophthalmol. 2005 Apr;123(4):437-47.
12.Cotter SA, Tarczy-Hornoch K, Wang Y, et al. Visual acuity testability in African-American and Hispanic children: the multi-ethnic pediatric eye disease study. Am J Ophthalmol. 2007 Nov;144(5):663-7.
13. Weakley DR Jr. The association between nonstrabismic anisometropia, amblyopia, and subnormal binocularity. Ophthalmology. 2001 Jan;108(1):163-71
14. Birch EE, Stager DR. The critical period for surgical treatment of dense congenital unilateral cataract. Invest Ophthalmol Vis Sci. 1996 Jul;37(8):1532-8.
15. Birch EE, Stager DR. Prevalence of good visual acuity following surgery for congenital unilateral cataract. Arch Ophthalmol. 1988 Jan;106(1):40-3.
16. Lambert SR, Lynn MJ, Reeves R, et al. Is there a latent period for the surgical treatment of children with dense bilateral congenital cataracts? J AAPOS. 2006 Feb;10(1):30-6.
17. Mahoney NR, Liu GT, Menacker SJ, et al. Pediatric horner syndrome: etiologies and roles of imaging and urine studies to detect neuroblastoma and other responsible mass lesions. Am J Ophthalmol. 2006 Oct;142(4):651-9.
18. Smith SJ, Diehl N, Leavitt JA, et al. Incidence of pediatric Horner syndrome and the risk of neuroblastoma: a population-based study. Arch Ophthalmol. 2010 Mar;128(3):324-9.
19. Bai S, Ren R, Shi J, et al. Retinoblastoma in the Beijing Tongren Hospital from 1957 to 2006: clinicopathological findings. Br J Ophthalmol. 2011 Aug;95(8):1072-6.
20. MejÃa Aranguré JM, Flores Aguilar H, Juárez Muñoz I, et al. Age of onset of different malignant tumors in childhood. Rev Med Inst Mex Seguro Soc. 2005 Jan-Feb;43(1):25-37.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.