Scleral contact lenses help manage ocular surface disease

In the past few years, scleral gas permeable (GP) contact lenses have become an integral part of the specialty contact lens practice. Uses of scleral lenses have expanded from the irregular cornea patient to many other uses, including patients with dry eye and other ocular surface conditions.
Scleral lenses provide a liquid reservoir that functions to help correct corneal irregularities and also to provide relief and healing of the ocular surface. In addition, scleral lenses prevent desiccation due to exposure and protects the cornea from trauma due to blinking.
According to the original Dry Eye Workshop (DEWS) study in 2007, approximately 5 million Americans over the age of 50 suffer from dry eyes.1Related: What's so special about specialty lenses?
Looking at dry eye
Many patients experience contact lenses intolerance. In addition, moderate to severe dry eye, such as those patients with systemic health conditions, can be helped by scleral contact lenses. The Scleral Lenses in Current Ophthalmic Practice Evaluation (SCOPE) study group reported that ocular surface indications comprised 16 percent of scleral lens fits.2
Advancements in lens manufacturing technology, lens materials, corneoscleral imaging, knowledge, experience, and fitting techniques have expanded the capabilities of treating those patients with compromised corneas.
According to the Tear Film and Ocular Surface Society (TFOS) Dry Eye Workshop DEWS II report, those who are symptomatic with signs of ocular surface disease may benefit from scleral lenses and show improvement in corneal punctate staining and filamentary keratitis. In addition, the DEWS II report stated that those with neurotrophic keratitis and neuropathic pain may benefit from scleral lenses.3Related: Blog: Don't leave dry eye disease patients high and dry
Ocular surface conditions
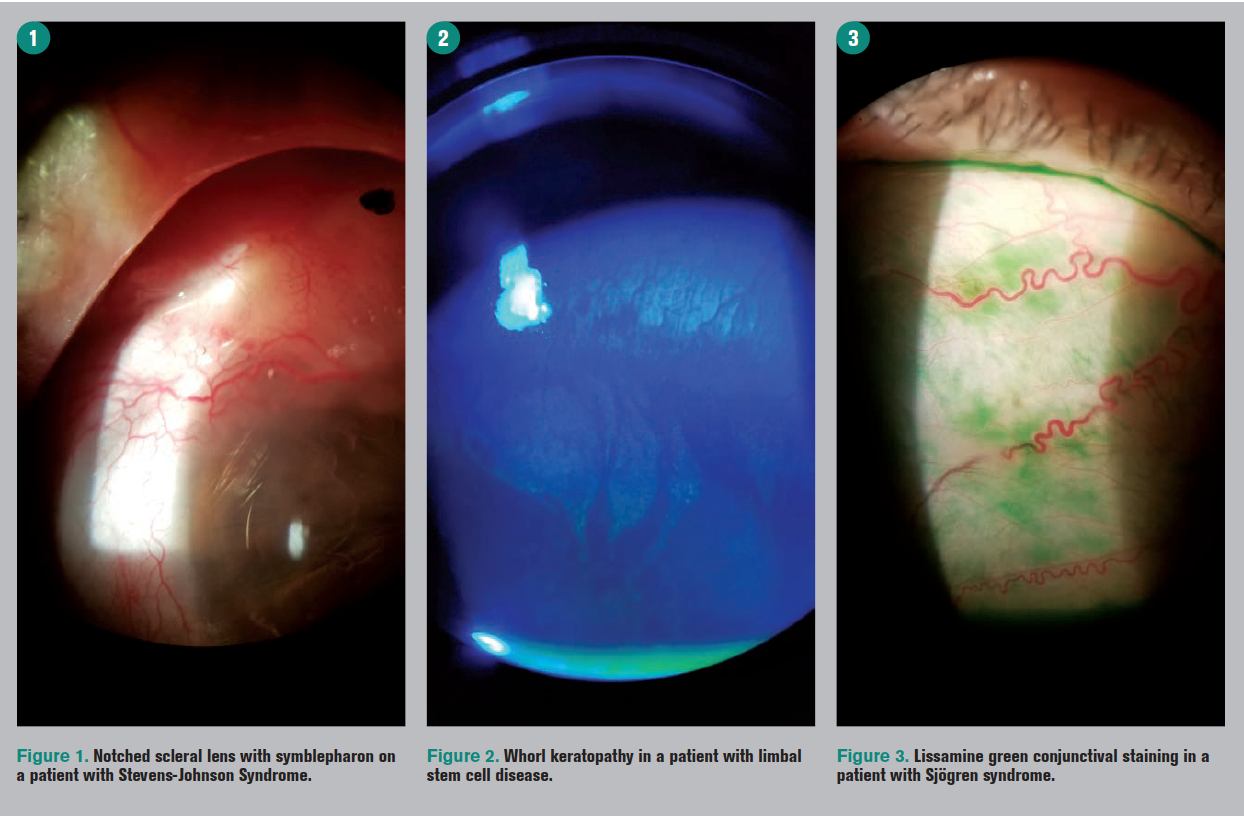
Severe ocular surface conditions-such as graft vs. host disease (GvHD), Sjögren syndrome, limbal stem cell disease (LSCD), filamentary keratitis, and exposure keratopathy-are challenging to treat, and scleral contact lenses may provide an effective option in the management of these refractory conditions.
Many patients with keratoconus and other forms of corneal ectasia and post-surgery patients also present with concomitant dry eye.
It is important to relay to patients that scleral lenses will not “cure” their ocular surface disease, and they will need to continue their current therapies and close follow-up care with their prescribing doctors and other medical specialists.
Related: Fitting ortho-k contact lenses
Typically, scleral lenses are utilized after more traditional therapies such as lubricants, cyclosporine (Restasis, Allergan), lifitegrast (Xiidra, Shire), topical steroids, bandage contact lenses, and punctual plugs have been employed. Additional therapies for severe dry eye include autologous serum and amniotic membranes.
Patients also need to be aware that the use of scleral lenses with dry eye conditions may require additional or extra care compared to other conditions.
Those with dry eye typically produce more mucus, and this may deposit on the anterior surface of the lens and/or in the post-lens tear layer reservoir. This may affect the patient’s vision.
Rinsing and refilling the lens may be necessary with tear film reservoir fogging; however, it may induce more clouding over time with insult to the goblet cells, causing more mucus production (a vicious cycle scenario).
In addition, the scleral lens surface is drier in ocular surface disease patients.
Related: Scleral lens aids in visual rehabilitation
Anterior surface filming can be addressed by adding Tangible HydraPEG (Tangible Science) lens treatment. It is currently available on Contamac materials and was recently approved on Boston lens materials.
Proper care of HydraPEG-coated lenses is critical to preserve the effectiveness of the coating. Patients must be educated on the approved solutions to be used with Tangible HydraPEG-tap water is contraindicated.
Anecdotally, the HydraPEG coating lasts for a shorter time on those patients with ocular surface disease. Tangible Science is planning to launch new care products for HydraPEG-coated lenses which may extend the effectiveness and performance of the coating.
Frequent artificial tear use may be necessary to properly lubricate the lens surface, lids, and conjunctiva because scleral lenses do not cover the entirety of the conjunctival surface. Lubrication drops may also reduce friction of the lid rubbing up against the lens.
Dry eye patients may require more frequent replacement of scleral lenses. Many dry eye patients also may not be able to sustain full-time lens wear due to the severity of their condition.
Related: 10 tips to enhance scleral contact lens success
In addition, treat meibomian gland dysfunction (MGD) aggressively. Chronic MGD and anterior blepharitis must be addressed because these conditions can adversely affect the performance of the contact lens and treatment of the underlying ocular surface conditions.
I recommend performing lid hygiene along with use of oral and topical medical treatment of eyelid disease.
There are also many adjunct therapies available to treat MGD, such as LipiFlow (Johnson & Johnson Vision), MiBo Thermoflo (Mibo Medical Group), iLux (Alcon), and TearCare (Sight Sciences) with more options coming in the future.
Proper patient instruction and monitoring of eyelid disease is critical in successful scleral contact lens wear. Using hypochlorous acid products and devices to debulk the eyelids is also an important step. Addressing the proper types of makeup and soaps are also critical in managing patients with ocular surface disease.
Related: Understanding the link between MGD and OSD
Lens care
Especially important in ocular surface disease patients is the use of proper scleral lens preservative-free saline. This saline will be bathing the cornea throughout the wear of the lens. Using inappropriate lens-filling solutions can adversely affect the cornea.
Currently available saline solutions include ScleralFil (Bausch + Lomb), Lacripure (Menicon), PurilensPlus (The Lifestyle Company), and off-label sodium chloride 0.9% inhalation vials.
Due to the fragile ocular surface in dry eye and ocular surface disease patients, non-preserved, non-buffered saline solution is recommended to reduce toxic reactions of the cornea.
Related: Work with patients to combat contact lens obsolescence
Ordering lenses
In 2019, there is a plethora of scleral lens manufacturers, lens designs, and lens materials available. Information that is critical in determining an initial lens includes horizontal visible iris diameter (HVID), corneal shape and profile, lid aperture size, and conjunctival or lid obstacles.
It is essential that the scleral lens be large enough to completely clear the limbus and vault the cornea. Typically, the more severe the ocular surface condition, the larger the lens diameter required.
Lens setting must also be taken into account when evaluating the lens. Proper clearance of the limbus is critical in keeping the fragile limbal stem cells intact. This is especially vital in those patients with pre-existing ocular surface disease.
Related: Amniotic membrane grafts help ocular surface disease
In some cases proper haptic alignment utilizing toric peripheral landing zones is important in the performance of the lens. A larger diameter lens may require toric haptics because the sclera has more toricity farther out from the limbus. Proper lens alignment with the sclera will prevent post-lens tear layer fogging in the case of edge lift or scleral blanching and impingement in tight haptics.
Many contact lens laboratories are able to manufacture lenses that allow the lens to avoid corneal or conjunctival obstacles such as pingeculae, elevated corneal scars, or glaucoma shunts. This is important because many glaucoma patients have both surgical tubes and concurrent ocular surface conditions that would be helped by scleral lens technology.
In addition, patients with Stevens-Johnson syndrome may have obstacles such as symblepharon which need haptic customization.
Related: GPC leads to contact lens instability
Conclusion
Scleral contact lenses have emerged as a go-to treatment modality in specialty contact lens practice in vision correction. Likewise, the use of large-diameter GP scleral lenses have become indispensable in the management of patients with multiple types of ocular surface disease. They provide excellent vision, comfort, and ocular health for those patients faced with challenging corneal and anterior segment conditions.
Read more contact lens content
About the authorDr. Sorkin is president of the Essex County Optometric Society, a member of the medical advisory board for the International Keratoconus Academy, and New Jersey State OD of the Year in 2018. He discloses relationships with Baush + Lomb, Blanchard Laboratories, BostonSight, Shire, and Visioneering Technologies, Inc.
eyedoc1228@gmail.com
References:
1. The epidemiology of dry eye disease: report of the Epidemiology Subcommittee of the International Dry Eye Workshop (2007). Ocul Surf. 2007 Apr;5(2):93-107.
2. Nau, CB, Harthan, J, Shorter E, Barr J, Nau A, Chimato NT, Hodge DO, Schornack MM. Demographic characteristics and prescribing patterns of scleral lens fittters: the SCOPE study. Eye Contact Lens. 2018 Sep;44 Suppl 1:S265-S272.
3. Craig, JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo CK, Liu Z, Nelson JD, Nichols JJ, Tsubota K, Stapleton F. TFOS DEWS II definition and classification report. Ocul Surf. 2017 Jul;15(3):276-283.

Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.