Treating patients with brain injuries
The idea of working with patients with brain injuries can be intimidating at first. The results can be rewarding for the patient, family, and yourself, making it worth the time and effort spent. Whether you are the last stop on a frustrating journey or the diagnosing clinician, the difference you can make is life-altering
Approximately 2.6 million people suffer a traumatic (TBI) or acquired brain injury (ABI) annually;1 this is a staggering number. Optometrists, in many cases, are part of the treatment team, or they may be the first point of contact. Patients with brain injury will inevitably walk into your office, and you must be prepared to step up to the plate to ensure your patient’s visual and systemic well-being.
Acquired brain injury is an injury to the brain that is not congenital.2 The most common cause, by far, is stroke/cerebrovascular accident(CVA), followed by tumor, and aneurysm.1 The incidence annually of ABI is about 917,000 individuals. A TBI is a sudden physical assault on the head that causes damage to the brain.2 The trauma can be a closed (shaken baby syndrome, stroke) or penetrating head injury (gun shot, car accident). TBI is the leading cause of death and disability among children and young adults in the United States. Approximately 1.7 million Americans sustain a TBI each year,3 and 5.3 million live with a long-term disability as a result.1 A greater risk has been documented in adolescents, young adults, and persons older than age 75. Men are twice as likely as women to sustain a TBI.1 About 75% of TBIs that occur each year are concussions or other forms of mild TBI.4 The common causes include accidents, falls, assaults, and work-related trauma. Blasts are a leading cause of TBI for active duty military personnel in war zones.5
An understanding of the anatomy and physiology of the brain is necessary; the area of the brain injury will dictate the types of deficits with which patients present (Figure 1). The left hemisphere is responsible for language, memory, and analysis. The right hemisphere is responsible for object location, body position, remembering, and forming percepts. Table 1 reviews the specific functions of the lobes of the brain.6
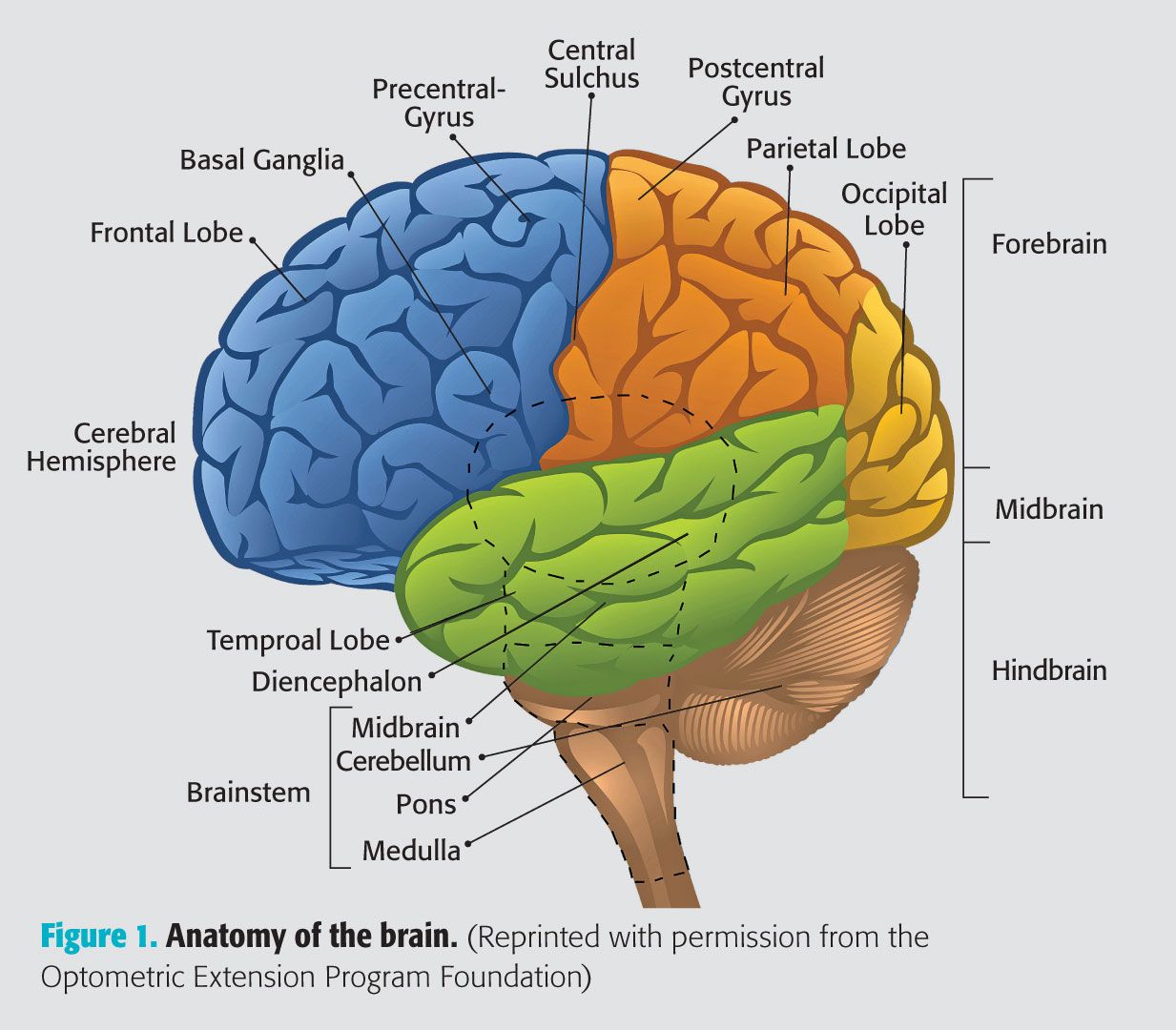
Figure 1. Anatomy of the brain. (Reprinted with permission from the Optometric Extension Program Foundation)
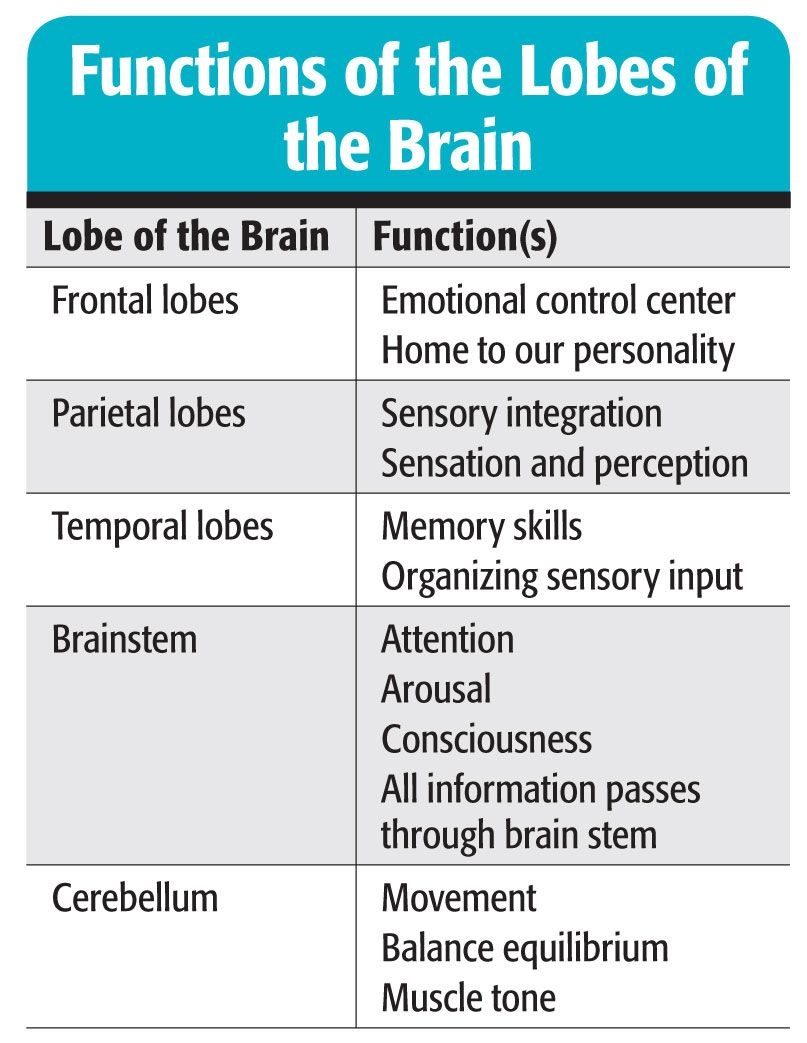
Table 1. Functions of the lobes of the brain.
While there are certainly patterns that emerge when treating patients with brain injury, no two patients are identical. Each patient’s injuries impact them differently-physically, socially, emotionally, and cognitively. Managing patient and family member expectations should be done cautiously, and promises should never be made. Patients who present for optometric care related to TBI and ABI range in age tremendously and often seek treatment anywhere from days to years after the initial incident. These patients typically are involved in several concurrent treatments, including physical, occupational, cognitive, and speech-language therapies, and are taking multiple medications. Working with the other professionals on the treatment team, including physical and occupational therapists, physiatrists, and a multitude of medical specialists, is vital. The optometrist will often need to coordinate care to ensure that visual care is incorporated into the greater treatment plan.
Brain injuries and vision
Regardless of the type of injury-TBI or ABI-the most common visual symptoms are similar. Patients often complain of loss of balance, dizziness, eyestrain and headaches with near work, loss of place while reading, and distance and near blur. Frequent concerns also relate to visual field defects, reduced or diminished stereopsis, reduced reaction time, reduced accommodative ability and flexibility, dry eye symptoms from a decreased blink rate, and reduced hand-eye coordination.7-9
The conditions encountered, including binocular vision, accommodative, ocular motor and visual information processing concerns, visual field defects/visual neglect, and nerve palsies, occur in greater amounts in relation to the general population. Alvarez et al,10 in a study involving 557 civilians with TBI, found in the inpatient subgroup:
• Convergence insufficiency both with and without simultaneous diagnoses (23.3% [130])
• Convergence insufficiency without simultaneous diagnoses (9%)
• Cranial nerve palsies (26.9%)
• Accommodative dysfunction (24.4% [76 of 314])
• Visual field deficits or unilateral visual spatial inattention/neglect (29.6% [80 of 270])
Within the convergence insufficiency subgroup, photophobia (16.3%) and vestibular dysfunction (18.5%) were detected.
Treating patients with brain injuries
In serving this population, optometric care can be provided either within the rehabilitation center or hospital as an inpatient, or as an outpatient in a traditional office. Both types of care can be challenging and require a different approach. In an acute care setting, you are tasked with ensuring both the quality of the visual system as well as the health of the eye. In slightly over 2 years of patient care at Memphis’ premier rehabilitation facility, I estimate that 20% of referrals were ultimately related to structure, not function. These problems can run the gamut from retinal to corneal in etiology. Artificial tears and ointments become vital treatment modalities. Keep in mind that the patient’s health history is not wiped clean and that findings may be related to previous conditions.
Visual complications should be approached in a stepwise manner, and you must address the patient’s and treatment team’s concerns. By far, the main problems that are found at the rehabilitation facility are related to visual field loss/neglect and diplopia. Both can impact the care the patient is receiving from occupational and physical therapists, so the goal is to eliminate diplopia and provide information to the care team to maximize success. If there is a field cut, therapists are educated and advised on how to best to work with that patient on their specific deficits. For example, if there is a right homonymous field defect, do not approach the patient from the right side. Seems simple, but a little bit of knowledge can go a long way.
Diplopia has a simple treatment-a black patch. Patch on, problem solved, right? Wrong! Full occlusion is in no way therapeutic and can inhibit the rehabilitation process in some cases. Occlusion should be aimed at preserving as much visual information as possible while eliminating the diplopia.11 For example, if the patient suffers from a 6th nerve palsy, there will be diplopia in a lateral view on the affected side. Patching of the temporal spectacle lens will help alleviate symptoms (Figure 2). Binasal occlusion could also be considered to reduce the amount of incoming visual information in patients with processing difficulties11 and has been shown to impact VEP amplitude in TBI patients.12 Another option for the relief of diplopia is Fresnel prism (Figure 3). This “stick on” prism can be applied to any spectacle lens, on either the front or back surface. Because the visual system is in a dynamic state, using this type of treatment allows for quick changes in the prism power as the healing process is taking place.

Activities aimed at preserving and improving visual function should be provided to the therapists because they are working with your patients on a daily basis. For example, for visual neglect, consider using yoked prism with varying orientations with hand-eye coordination activities to “show” the brain what it is missing. This will set the stage for the optometric vision therapy that will come later once the patient has been released from the acute care facility.
One of the difficulties related to in-patient care is vision correction. Because the average patient stay can last anywhere from 3 to 8 days, updating the prescription should be delayed unless in an extreme emergency. It can be a challenge for the practitioner to make a return trip for dispensing with such a tight window.
In the office, the practitioner must be prepared to improvise. Cognitive problems may prevent subjective testing, or the patient may be limited physically, reducing the ability to rely on traditional testing techniques. Testing may need to be broken up into several visits as fatigue may be an impediment. Having a variety of evaluation methods on which you can rely is the key to a comprehensive evaluation.
Optometric vision therapy is a crucial part of the treatment plan for those with an ABI or TBI. In a retrospective analysis of TBI/ CVA patients with oculomotor dysfunction, 100% of patents had successful treatment which was stable 2 to 3 months later.13 Convergence insufficiency, found in slightly under 25% of participants in the study by Alvarez et al,4 has been found to be best treated with in-office vision therapy, and it was successful in about 75% of patients (resulting in normal or significantly improved symptoms and signs).14 If the office at which you work does not offer optometric vision therapy, seek out the nearest provider to comanage the care. These optometrists can be located by using the doctor locater options at the Web sites for the Optometric Extension Program Foundation (www.oepf.org) and the College of Optometrists in Vision Development (www.covd.org). The Neuro Optometric Rehabilitation Association (www.nora.cc) should also be considered a great resource.
The idea of working with patients with ABI can be intimidating at first. The results can be rewarding for the patient, family, and yourself, making it worth the time and effort spent. Whether you are the last stop on a frustrating journey or the diagnosing clinician, the difference you can make is life-altering.ODT
References
1. Brain Injury Association of America. Brain Injury Facts. Available at: http://www.google.com/url?sa=t&rct=j&q=&esrc=s&frm=1&source=web&cd=1&ved=0CEkQFjAA&url=http%3A%2F%2Fwww.biausa.org%2FLiteratureRetrieve.aspx%3FID%3D104992&ei=-59BUpeUG4Ty2gXGsYCIAQ&usg=AFQjCNEcsXKQRbyU3qUudmEfLwVY5Mj3BQ&sig2=Vi-EU7nohbs8FjyrS0qLGQ&bvm=bv.52434380,d.b2I. Accessed 10/2/13.
2. Suchoff IB, Ciuffreda KJ, Kapoor N. An overview of acquired brain injury and optometric implications. In: Suchoff IB, Ciuffreda KJ, Kapoor N. Visual & Vestibular Consequences of Acquired Brain Injury. Santa Ana, CA: Optometric Extension Program Foundation. 2001, 1-10.
3. Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths. Atlanta (GA): Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010.
4. Centers for Disease Control and Prevention (CDC), National Center for Injury Prevention and Control. Report to Congress on mild traumatic brain injury in the United States: steps to prevent a serious public health problem. Atlanta (GA): Centers for Disease Control and Prevention; 2003.
5. Champion HR, Holcomb JB, Young LA. Injuries from explosions. J Trauma. 2009 May;66(5):1468-76.
6. Eubank, T. Beethoven in the vision therapy room. J Behav Optom. 2012;22(4);99-103.
7. Kapoor N, Ciuffreda KJ. Vision disturbances following traumatic brain injury. Curr Treat Options Neurol. 2002 Jul;4(4):271-80.
8. Cilo M, Politzer T, Ripley DL, Weintraub A. Vision examination of TBI patients in an acute rehabilitation hospital. NeuroRehabilitation. 2010;27(3):237-42.
9. Greenwald BD, Kapoor N, Singh AD. Visual impairments in the first year after a traumatic brain injury. Brain Inj. 2012;26(11):1338-59.
10. Alvarez TL, Kim EH, Vicci VR, Dhar SK, Biswal BB, Barrett AM. Concurrent vision dysfunctions in convergence insufficiency with traumatic brain injury. Optom Vis Sci. 2012 Dec;89 (12):1740-51.
11. Slotnick S, Baxstrom C, Clopton J. Optometric management of functional vision disorders. In: Taub MB, Bartuccio M, Maino D. Visual Diagnosis and Care of the Patient with Special Needs. Philadelphia: Lippincott Williams & Wilkins. 2012, 300-303.
12. Ciuffreda KJ, Yadav NK, Ludlum DP. Effect of binasal occlusion (BNO) on the visual-evoked potential (VEP) in mild traumatic brain injury (mTBI). Brain Inj. 2013:27(1);41-7.
13. Ciuffreda KJ, Rutner D, Kapoor N. Suchoff IB, Craig S, Han ME. Vision therapy for oculomotor dysfunctions in acquired brain injury: a retrospective analysis. Optometry. 2008 Jan;79(1):18-22.
14. Scheiman M, Rouse M, Kulp MT, Cotter S, Hertle R, Mitchell GL. Treatment of convergence insufficiency in childhood: a current perspective. Optom Vis Sci. 2009 May;86(5):420-8.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.