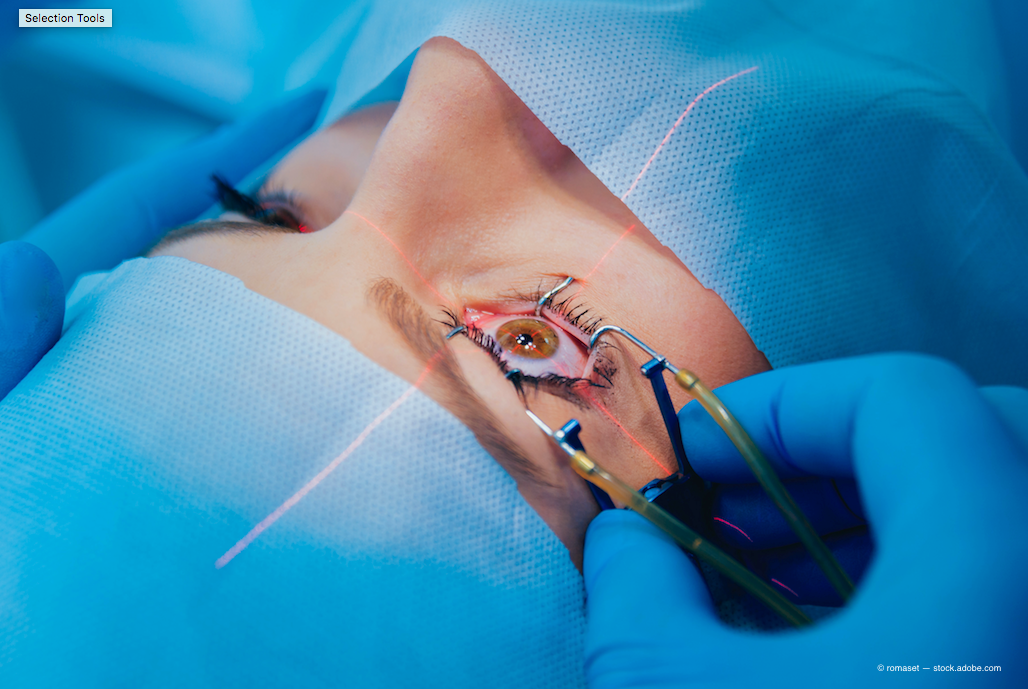
Understand the basics of cataract surgery measurements
Technicians play an invaluable role in eye care. Apart from performing eye tests and measurements, the technician is also something of a detective, obtaining key elements of the patient history and learning how to ask additional questions when the pieces of the puzzle don’t quite fit.
Taking measurements
One of the most critical tests that the technician performs is pre-cataract surgery eye measurements which are used to determine the power of the intraocular lens (IOL). Although current measurement technology is advanced, it is still important for the technician to understand the principles behind these measurements and learn to ask questions if the measurements don’t seem to make sense.
During cataract surgery, the natural lens of the eye is removed and replaced with an artificial IOL. The natural lens is part of the eye’s focusing system. The cornea is the primary refractor of light, accounting for about two-thirds of the eye’s focusing power. The lens provides the remaining one-third of the focusing power, or about 20.00 D.
Read more about cataract surgery
When this lens is removed, we replace it with an IOL which also has power. The power of that IOL is determined by the eye’s size and shape, along with the patient’s desired refractive end result.
The three primary measurements that we evaluate in order to determine the correct IOL power are:
• Axial length
• Corneal curvature (keratometry or K readings)
• Anterior chamber depth
These measurements are run through a particular formula to determine the correct IOL power to use for the patient.
Axial length
An eye with a long axial length and/or a steep cornea typically has a myopic refractive error, while an eye with a short axial length and/or a flat cornea is typically hyperopic.
A myopic eye will require a lower than normal IOL power, and a hyperopic eye will require a higher than normal IOL power. Remember, a myopic eye has “too much” focusing power, while a hyperopic eye has too little.
The axial length is the primary determinant of refractive error, so it is easy to understand the importance of this measurement. The axial length is defined as the distance between the cornea and the fovea; it is approximately 23.5 mm in the “normal” eye.
Related: 6 steps to manage cataract patient expectations
Axial length is measured with optical or ultrasound biometry, and every 1 mm change in axial length equates to approximately 3.00 D of refractive error change.
An eye that is significantly longer than 23.5 mm is myopic, while an eye significantly shorter than 23.5 mm is hyperopic.
It is important to note that corneal power can offset axial length. For example, a patient with a longer axial length and flat K readings may actually have no refractive error because the cornea power is canceling out the axial myopia.
Axial length is normally very similar between the two eyes, usually within 0.3 mm. It is unusual to see a large difference between the axial lengths; if such a difference is noticed while measuring the patient, verify by looking into the patient’s history. Is this difference noted in his old glasses prescription? Does the patient remember a difference between the two eyes when he was younger? Was he ever told he had a “lazy” eye?
Remember to check the historic glasses prescriptions when possible, along with verbally obtaining the patient history. Because a cataract can cause myopia, it can be difficult to correlate the patient’s current manifest refraction with his axial length measurements.
Keratometry
Keratometry is a measurement of the anterior curvature (power) of the cornea and is another critical component for determining IOL power.
The normal average keratometry or K value is about 44.00 D. This average value is the average of the K1 and K2 measurements taken by the keratometer. Given a normal axial length, an average K <44.00 D will usually result in a hyperopic refractive error, while an average K higher than 44.00 D will result in a myopic refractive error.
Just like axial length, the average K value between the two eyes is normally very similar, within 1.00 D. Evalute further if the patient exhibits a significant difference between the average K values. Check if there is something noted in the history that would help explain this difference, such as corneal scarring, corneal dystrophy, or dry eye syndrome. Has the patient had prior refractive surgery? Is the patient a contact lens wearer?
Corneal astigmatism is a common finding on eye measurements. In fact, it is rare to find a totally spherical cornea.
The technician should have an understanding of regular versus irregular astigmatism. Significant regular astigmatism will show a “bowtie” pattern on topography with the warmer colors of the bowtie indicating the axis of the astigmatism.
Related: When do you diagnose keratoconus?
Astigmatism is defined as with-the-rule (plus cylinder vertical; see Figure 1), against-the-rule (plus cylinder horizontal; see Figure 2), or oblique (think 10 o’clock and 2 o’clock; see Figure 3).
Astigmatic corneas normally have the astigmatism in the vertical meridian in both eyes, the horizontal meridian in both eyes, or the oblique meridian in both eyes. It is not normal to see significant astigmatism in the vertical meridian in one eye and horizontal meridian in the other eye. Patients with significant astigmatism in these opposite axes may have amblyopia. If this axis difference was not present since childhood, it is often the result of corneal scarring or corneal dystrophy, so ensuring that the patient history matches up with the measurement findings is very important.
It is now fairly common to see cataract patients who have had prior corneal refractive surgery. Sometimes the patient forgets to mention that she has had refractive surgery because it happened so many years ago or because she doesn’t think that it was “surgery.”
If the patient had PRK, there is no flap to be seen on slit lamp exam, and even LASIK flaps can sometimes be overlooked. Corneal topography measurements can show the effects of the refractive surgery, can provide an estimate of the amount of treatment performed, and show whether it was a hyperopic or myopic treatment.
Myopic corneal refractive treatment flattens the central cornea (see Figure 4), while hyperopic laser treatment steepens the central cornea (see Figure 5). A 1.00 D change in corneal power equals a 1.00 D change in refractive error, so looking at the average K value in a post-refractive eye gives a general idea of the patient’s prescription prior to her refractive surgery.
This can be helpful when counseling the patient for cataract surgery, and it is essential to know that the patient had refractive surgery in order to use the appropriate formula for selecting the IOL.
Anterior chamber depth
The third element measured for determining the appropriate IOL power for a patient is anterior chamber depth.
Anterior chamber depth helps determine the effective lens position of the new IOL.
An IOL that is more anterior in the eye is effectively a stronger lens compared to one that sits more posteriorly. Eyes with a shorter axial length tend to have a more shallow anterior chamber depth (<3 mm), while eyes with a longer axial length tend to have a deeper chamber (>3 mm).
Related: Educate your patients about astigmatism
More recent IOL formulas factor in the anterior chamber depth variable, which can increase the likelihood of hitting the desired refractive target.
It is also worthwhile to note that the anterior chamber depths of the two phakic eyes are normally symmetric. If not, bring this information to the surgeon’s attention.
This is especially important if the patient has pseudoexfoliation or a history of blunt trauma because an anterior chamber depth asymmetry in these situations can indicate that the lens zonules are affected and the lens is loose. Eyes that are pseudophakic have a much deeper anterior chamber.
Measurements are important
The surgeon performs the final evaluation of eye measurements prior to cataract surgery and determines the appropriate IOL power for the patient. But the technician plays a key role in making sure the measurements are accurate and should know what questions to ask if the measurements show an irregularity.
Obtain additional patient history when appropriate, repeat measurements, or ask for assistance as needed.
Above all, communicate unusual measurements to the surgeon so the surgeon is able to counsel the patient and determine the best surgical plan.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.