10 reasons contact lens care is important
We often put all the emphasis on the contact lens itself. It’s the first thing we change when things aren’t right, but it may be an unnecessary change if we consider the impact lens care has on the overall wearing experience. Because lens care products differ in how they clean, disinfect, and wet the lens, it is essential that we differentiate among them.
We often put all the emphasis on the contact lens itself. It’s the first thing we change when things aren’t right, but it may be an unnecessary change if we consider the impact lens care has on the overall wearing experience. Because lens care products differ in how they clean, disinfect, and wet the lens, it is essential that we differentiate among them. And having the lens care discussion can be just as important as the brand itself. It elevates patients’ awareness-and hopefully attentiveness-in how they care for and wear their lenses, thereby adding a layer of protection from complications or failure.
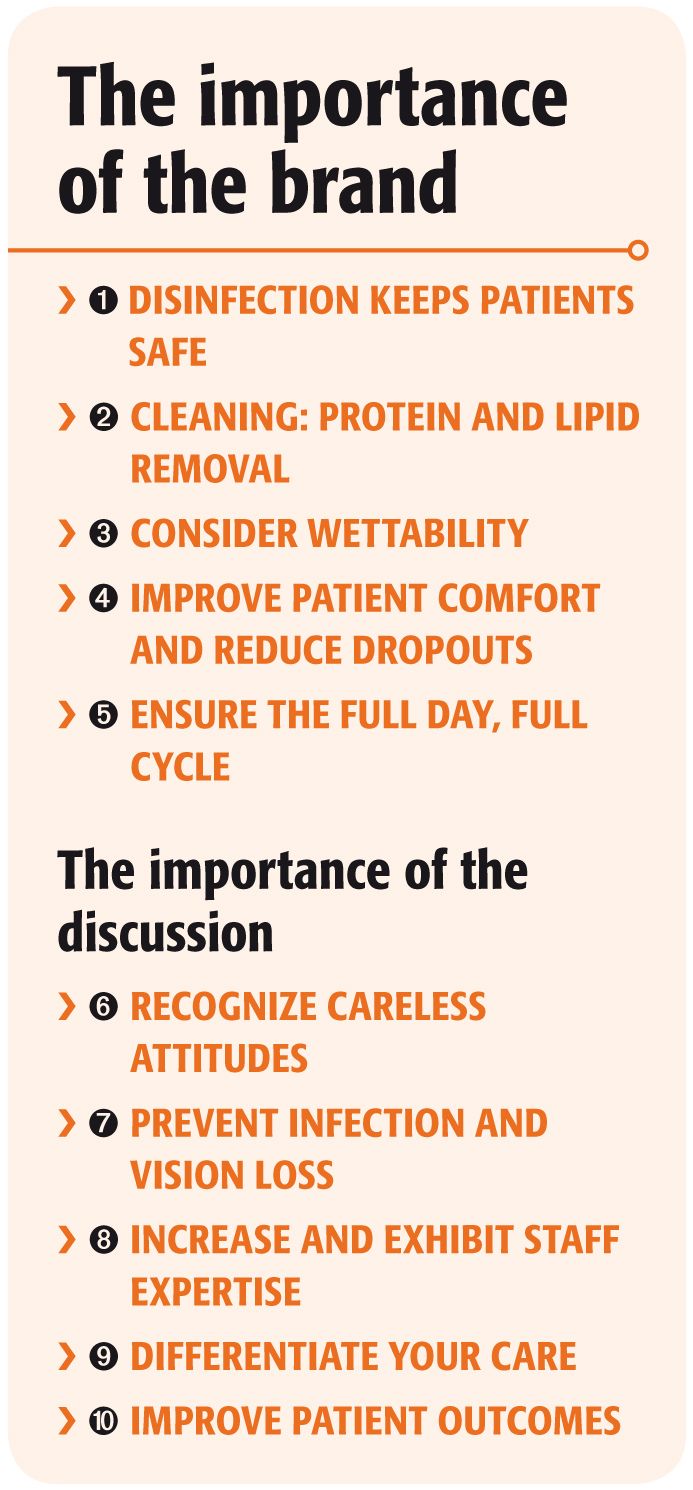
The importance of the brand
1. Disinfection keeps patients safe. Years ago, we used a separate lens cleaner, rinse, enzyme, and heating device to keep our lenses safe. For most patients, that laborious regimen has been reduced to an all-in-one multi-purpose or peroxide-based solution.
While the multi-purpose solution has to be strong enough to disinfect the lens for patient safety, it also has to be gentle enough to go straight into the eye without harming the epithelial cells. This is no simple accomplishment.
For multi-purpose disinfectants to be safe in the eye, it is assumed that the disinfectant concentration is much lower than the separate bottles from the years past. Therefore, it is important that the disinfectant remain in the solution at full concentration.
Recently, the U.S. Food and Drug Administration (FDA) drew our attention to preservative uptake into the lens and the resultant reduction of the antimicrobial capacity of the residual solution in the case.1,2 This could impact patient safety for the many who habitually top off or reuse their solution.
2. Cleaning: protein and lipid removal. Fortunately, with the progress of technology, the wear cycle that was once a full year for most has been reduced to as little as one day. Because of that, protein removal and giant papillary conjunctivitis (GPC) are certainly a smaller concern than in days past, but we may underestimate the wear cycle’s influence. Any deposition on the lens can cause a reduction of lens wettability and disruption of the tear film, which can have negative effects on patient comfort and vision. And once the lens begins to deposit, it can accumulate more quickly. Out of convenience, we often schedule our contact lens follow-ups at 1 week-instead of 2 or 3-and may fail to even identify build up as a problem. A peroxide-based system, such as Alcon Clear Care or recently launched Bausch + Lomb PeroxiClear, is often considered the go-to product for removing build up from the lens, but many reserve it for “problem patients.”
3. Consider wettability. Limiting lipid and protein accumulation can aid in preserving a wet lens surface, but it takes more than that to truly deliver elevated comfort to the patient. Most solutions utilize some sort of wetting agent, but they vary widely in their sophistication and efficacy. This is an essential solution component because when a dry patch disrupts the tear film, it causes reduced comfort but also poorly sustained vision and frequent blinking.
In some cases, the additive is a simple moisturizing agent. Other solutions incorporate advanced molecules designed to attach and maintain moisture on the lens surface throughout the day. The success of the surfactant will have a significant impact on the patient’s wearing experience.
Even though some patients may seem comfortable on the surface and report being “fine” with their lenses, they often appreciate the difference an effective surfactant can make.
4. Improve patient comfort and reduce drop outs. The number of patients who drop out of contact lens wear is astonishing-reportedly more than20% of wearers.3 Admittedly, this is difficult to track in our offices because we don't realize the patient has quit until he finally decides to return for new glasses. But this means we have to gain at least that many new wearers just to sustain our contact lens business.
Regardless of the study, discomfort is usually documented as the number one reason a patient drops out.3,4 It is reasonable to assume that if we are intentional in recommending a solution that improves comfort throughout the year, it may help patients push through challenging times, and thereby improve patient retention. The solution’s biocompatibility, its surfactant, and its ability to limit deposition are all solution-dependent factors that affect patient comfort and success.
5. Ensure the full day, full cycle. No patient is pleased when she has to discard her lenses early; however, it is a harsh reality for some. Ideally, these patients are transitioned into a daily disposable lens, but that’s not always possible. If the patient insists on or is limited to a reusable lens, it is essential that we actively manage what solution she is using.
If we recommend a solution known to better reduce and remove deposition, it will ensure a longer and more comfortable wearing cycle for the patient. Not only can this affect how often the lens is discarded, it can mandate how many hours a lens can be comfortably worn in a day. And adding even 2 hours wear time to a patient’s day can significantly impact her quality of life.
The importance of the discussion
6. Recognize careless attitudes. It is important that we know what our patients are thinking (stop laughing). When we have a discussion about which solution they use and how they care for their lenses, we can often identify those with lackadaisical attitudes toward lens wear.
Once these patients are identified, we can attempt to better educate them but also remain on high alert regarding their current and future behaviors. At one time or another, we have all been concerned with patient liability, even when it’s secondary to irresponsibility. This particular discussion can raise our awareness and potentially change the tone and type of conversations we have with this patient.
7. Prevent infection and vision loss. Some patients skirt lens care responsibilities knowingly, and others do it out of absent or misguided direction. By having the conversation, we can actively improve the cleaning regimen and habits of our patients. Just by enlisting the work-up technician to review proper cleaning techniques with every new and established wearer, we can drastically improve the safety of our patients.
More often than not, cases of contact lens-related microbial keratitis (MK) and vision loss are linked to noncompliance with lens care and wear.5 We can potentially reduce the chance of MK in our chair if we take the time to instill better cleaning habits in our patients.
8. Increase and exhibit staff expertise. It is essential that the staff know which solution you recommend and why. This is an easy opportunity to expand the knowledge and expertise of your staff. It also helps them realize the importance of lens care and the emphasis that is needed. As an added benefit, the patient will perceive the staff as being well trained and knowledgeable in all the details affecting her care.
9. Differentiate your care. In today’s market, competition and insurance plans are making it harder to capitalize. One thing that is not comparable from one practice to the next is the care you give and the patient experience you offer. If we are to survive and succeed in this climate, it is essential that we differentiate our service.
By having the lens care discussion, we are essentially tailoring our care to the individual patient and offering him complete contact lens care. The patient will likely perceive that we have gone out of our way to detail everything that might influence his wearing experience, which enhances the patient experience and develops loyalty.
10. Improve patient outcomes. I have come to believe that if a patient doesn’t have to hide his habits from the doctor, he will be more likely to return sooner with a problem. If the lens care discussion is done correctly, it should establish a sense of consequence for the patient.
If he realizes what a difference something seemingly little, like lens care, makes on healthy lens wear, it may increase his overall awareness and willingness to return quickly with the slightest red eye or discomfort. And early detection improves outcomes. Not only would this be helpful in an infectious course, but in the case of nagging discomfort, that return visit may ensure retention.
Too many times lens care products are clumped together as being the same. It is important for us, as physicians, to differentiate the disinfectants, cleaners, and surfactants between products, educate our patients, and recommend specific brands according to each patient’s needs. This will not only improve the patient’s comfort, vision, and habits, but also his perception of the care that’s delivered.ODT
References
1. Shoff ME, Lucas AD, Brown JN, et al. The effects of contact lens materials on a multipurpose contact lens solution disinfection activity against staphylococcus aureus. Eye Contact Lens. 2012 Nov;38(6):368-73.
2. Clavet CR, Chaput MP, Silverman MD, et al. Impact of contact lens materials on multipurpose contact lens solution disinfection activity against Fusarium solani. Eye Contact Lens. 2012 Nov;38(6):379-84.
3. Dumbleton K, Woods CA, Jones LW, Fonn D. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens. 2013 Jan;39(1):93-9.
4. Rumpakis J. New Data on Contact Lens Dropouts: An International Perspective. Review Optom. 2010;147(11):37-42.
5. Stapleton F, Edwards K, Keay L, et al. Risk factors for moderate and severe microbial keratitis in daily wear contact lens users. Ophthalmology. 2012 Aug;119(8):1516-21.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.