4 steps to care for ophthalmic instruments
Proper care and handling of ophthalmic instruments is essential in decreasing the risk of healthcare-acquired infections.
Proper care and handling of ophthalmic instruments is essential in decreasing the risk of healthcare-acquired infections. Whether instruments are processed in clinic, surgery, or a surgical center, the same critical steps apply: cleaning/decontamination, sterilization, quality control, and storage. Each step plays an important role in infection prevention. Below are some guidelines to help guide you through each step.
1. Cleaning/decontamination
The cleaning of instruments should begin immediately during the procedure to prevent drying of blood, soil and debris on the surface and within lumens. Debris that remains on instruments can block the sterilizing agent from making complete contact with the surface.
Manual cleaning includes wiping instruments clean using a sterile, water-moistened sponge. A soft toothbrush can also be used to clean instruments. Instruments with lumens should be flushed with distilled water followed by compressed air. About 120 cc of fluid is recommended.
More from iTech: How to create a happy patient
If you are using mechanical cleaning, such as an ultrasonic cleaner, the water in the ultrasonic cleaner should not exceed 140ðF/60ðC. Prior to exposing instruments to the ultrasonic cleaner, instruments should be completely opened or disassembled in order to expose all parts of the instrument. Needle holders, forceps, and scissors must be completely opened to clean inside the jaws. Key characteristics of a cleaning agent are:
̢ۢ Low sudsing/foaming
̢ۢ Biodegradable
̢ۢ Easily rinsed off
̢ۢ Non-abrasive
̢ۢ Disperse organic soil
̢ۢ Non-toxic
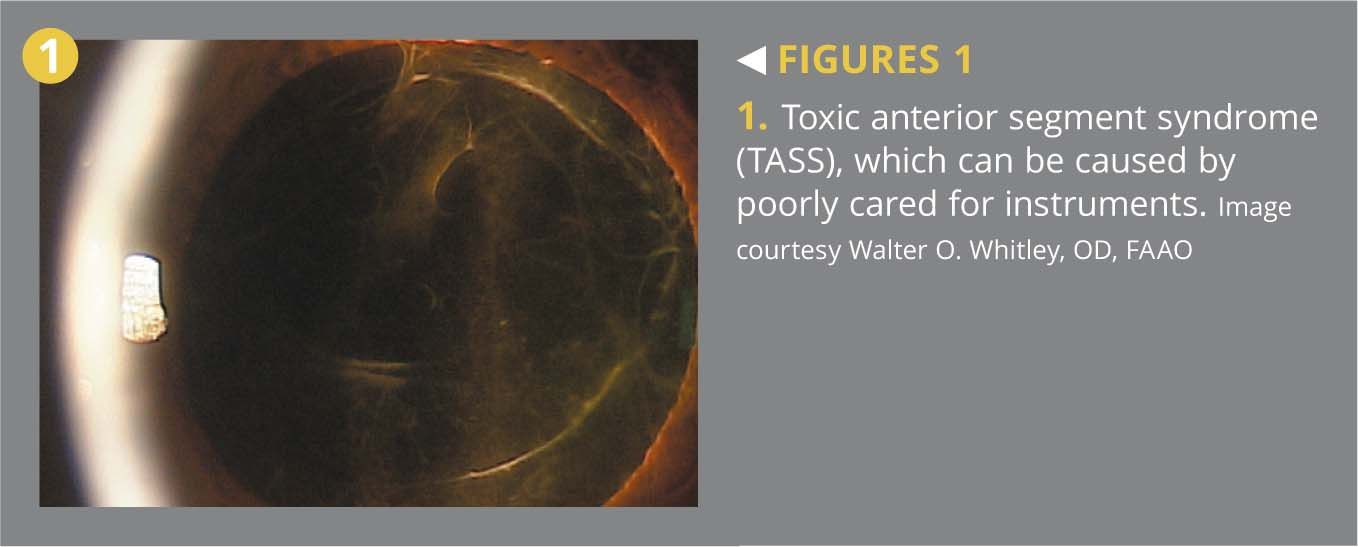
Cleaning solution should be mixed with measured amounts of water and detergent—do not guess. To decrease the risk of toxic anterior segment syndrome (TASS), do not expose lumens to detergent. Instruments must be thoroughly rinsed with copious amounts of water, distilled water preferred, for adequate removal of detergent. If rinse volumes are specified, the volume represents the minimum volume. If you are using tap water for rinsing, be sure it is compatible with the manufacturer’s recommendations for detergent and equipment. Always follow the manufacturer’s recommendation for the care and handling of each instrument and the instructions for use of the ultrasonic cleaners.
More from iTech: Clinic safety: Incidents, medication, and consent
For stiff instruments, lubricant can be used. Lubricant is recommended for hinged instruments only, such as scissors, needle holders, and forceps. Lubricant prevents the development of stiff joints and inhibits the development of corrosion. The instruments are dipped, one by one, into the lubricant; do not soak instruments in lubricant or expose lubricant to instruments containing a lumen.
Before storing instruments, be sure they are thoroughly dried. Instruments stored wet or damp will rust.
Next: Sterilization
2. Sterilization
Sterilization can be achieved through many different methods. Common methods in the sterilization of ophthalmic instruments include chemical sterilization (liquid, gas) and heating (moist heat).
Heat. Although heating provides the most reliable way to rid objects of transmittable agents, it is not always appropriate. Heating can cause damage to heat-sensitive materials, including fiber optics, electronics, and some plastics.
Steam sterilization is the oldest, cheapest, and best understood method of sterilization. Steam sterilization is achieved through the use of an autoclave. The autoclave acts as a large pressure cooker. It operates by using steam under pressure as the sterilizing agent. High pressures enable the steam to reach high temperatures, increasing its heat content and killing power. Moist heat kills microorganisms by causing coagulation of proteins. The vibration of each molecule of a microorganism causes splitting of hydrogen bonds between proteins. Death is caused by irreversible damage to all metabolic functions of the organism. The more moisture present, the more heat can be carried, making steam one of the most effective carriers of heat and effective methods of sterilization.
Steam sterilization is achieved through various methods and cycle parameters. It is important to follow the sterilizer̢۪s manufacturer̢۪s recommendations when making a selection.
Chemical. For heat and moisture sensitive items, liquid sterilants can be considered. Liquid sterilants include oxidizing agents (aldehyde). Glutaraldehyde has many uses, including a leather tanning agent, fixative for electron microscopy, tissue fixative, resin or dye intermediate, embalming fluid, preparation of dental materials, X-ray film processing, and surgical grafts and bioprostheses. Glutaraldehyde works as a high-level disinfectant and sterilizing agent by completely immersing items in the solution for an extended period of time.
More from iTech: How techs should handle ocular emergencies
Familiarize yourself with the potential hazards of glutaraldehyde prior to use. Glutaraldehyde releases toxic fumes, especially when heated. These fumes have a pungent odor and are irritating to the eyes, nose, throat, and respiratory tract. Residual solution can also be extremely toxic to intraocular and extraocular tissue. It is essential to practice thorough rinsing of all instruments exposed to glutaraldehyde, assuring all solutions are removed from the instruments. Refer to the safety data sheet (SDS) for glutaraldehyde for complete information regarding its use. Information can also be found through the Centers for Disease Control and Prevention (CDC) , Workplace Safety & Health Topics; and Occupational Safety and Hazard Administration (OSHA), Best Practices for the Safe Use of Glutaraldehyde in Health Care.
Another alternative method for sterilizing heat sensitive items is the use of ethylene oxide (EO). Ethylene oxide is an organic chemical and a member of the ether group. EO completely permeates porous materials and is compatible with packing material that prolong storage life. It is noncorrosive, doesn̢۪t damage items, and it is safe for lensed instruments. Disadvantages for EO is that EO equipment can be expensive and cycles can be expensive to run. EO requires aeration and can be harmful to the operator. EO is carcinogenic and mutagenic. It has a long, slow, and complex process. EO in its pure form is extremely flammable, requiring special precautions when determining storage. As in all hazardous chemical products, please refer to the product SDS for complete information regarding its use.
Next: Quality control
3. Quality control
The proper use of sterilization is an important and crucial aspect of infection control and prevention. Quality control methods must be used to assure effective management of the sterilization process. Quality control can be achieved through monitoring devises. These are tools to validate the autoclaving process.
Mechanical or physical monitoring includes printouts, charts, gauges, and digital displays. These measure time, temperature, and pressure and provide real-time evaluation of the sterilization conditions, resulting in a permanent record. At the end of each sterilization cycle, the operator should verify the correct parameters were met using physical monitoring before the items are removed.
Chemical monitoring includes chemical indicators or indicator strips. These indicator strips react to change in the physical conditions in the sterilizer. It comes as treated paper that changes color when exposed to certain sterilization parameters. There are six classes of chemical indicators. The classification structure is used to denote the characteristics and intended use of each type of indicator.
More from iTech: Identifying malignant eyelid tumors
For example, Class 1 indicators are process indicators and serve to differentiate processed packs from unprocessed ones. They are designed to react to only one critical process variable and can be used as an external indicator to verify the items were processed. A Class 5 indicator reacts to all critical process variables (time, temperature, and saturated steam) and can be used as an internal indicator to verify the sterilant penetrated the inside of a package or container.
Biological monitoring, more commonly known as a bug test, includes self-contained spores in a vial with a sealed ampule of growth medium. The biological indicator is exposed to a sterilization process. It is then activated by crushing the ampule, allowing the medium to create a growth environment for the bug. The indicator is then incubated to allow the growth of microorganisms. The incubation process produces acid byproducts, causing the medium to change color. Spores that were exposed to a sterilization process are killed, unable to produce acid, thus producing no color change. A control should always be used each time a biological indictors is used. The control bug is not sterilized. It is activated and incubated. The spores not exposed to a sterilization process and killed produce a color change, resulting in a positive test. This color change provides the operator a comparison for the sterilized bug.
Sterilizers that fail a quality control test should be taken out of service. The results should be reported immediately to a supervisor or appropriate person.
Testing read by an outside third party company is also recommended. Third-party testing provides results from an outside source. During outside testing, a spore strip and control strip are exposed to a sterilization process. The cycle parameters are documented and sent to an outside company for testing and the results are returned.
Next: Sterile storage
4. Sterile storage
A commonly used product for sterile storage is sterilization peel pouches. Peel pouches are appropriate for small, lightweight instruments. An appropriate size pouch should be chosen to allow for circulation of steam. Tip protectors should be used to prevent the tips from damage and to prevent compromising the package. Tip protectors should be steam permeable and fit loosely. Pouches should contain a chemical indicator inside the package to assure the sterilant penetrated the package.
More from iTech: Running a perfect clinic
Packages should be labeled for accurate identification and tracking. Label should include the sterilizer number (if using more than one sterilizer), cycle or load number, date of sterilization, description of contents, and assembler identification (initials of who packed the pouch).
When storing packages, items should not be stored on floors or windowsills or areas other than designated shelves or counters. Do not use elastic bands or paper clips to secure packages together. These items can compromise the integrity of the package. The shelf life of a package does not expire—rather it is event related. The shelf life depends on the quality of the packaging material, storage conditions during transport, and the amount of handling.
Prior to use, packages should be visually inspected for integrity and labeling.
Take the time to do it right
Proper handling and processing of ophthalmic instruments is crucial to infection control and prevention and the safety of your patients.
A good friend once told me it takes just as much time to do it wrong as it does to do it right. Be your patient̢۪s advocate. Take the time to do it right.
Click here to check out more from iTech
References
1.Ingrid Cox, RGN KRN COA ENB 176 and Sue Stevens, RGN RM OND FETC. (n.d.). Care of ophthalmic surgical instruments. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1705974
2.American Society of Ophthalmic Registered Nurses. (2006). Care and handling of ophthalmic surgical instruments
3.ANSI / AAMI ST 79. (2006). St79.comprehensive guide to steam sterilization. Retrieved from 2006 http://marketplace.aami.org
4.AST: Association of Surgical Technologists. (2009). recommended standards of practice for the decontamination of surgical instruments. Retrieved from http://www.ast.org/pdf/Standards_of_Practice/RSOP_Decontamination
5.Nick Mamalis, MD, Carolee Cutler, MD, MPH. (2010). Flushing: The best way to prevent tass. Retrieved from http://www.optisurgical.com/downloads/AOI-QR-Advertorial-April-2010.pdf
6.Steam Sterilization. Continuing Education Study Guide Presented by Steris
7.Howard Judelson. (2004, June 28). Operation of the autoclaves. Retrieved from http://oomyceteworld.net/protocols/autoclave operation.pdf
8.Kenneth Todar, PhD. (2011). Online textbook of bacteriology. Control of microbial growth. Retrieved from http://textbookofbacteriology.net/control
9.VERIFY̢㢠Steam Integrator Strips. (2014, January 1). Retrieved August 2, 2014, from http://www.steris.com/products/chemical-indicators/verify-steam-integrator-strips
10.Steam Chemical Indicator Classifications. (n.d.). Retrieved August 2, 2014, from http://multimedia.3m.com/mws/mediawebserver?mwsId=66666UF6EVsSyXTtnXT6nxMEEVtQEVs6EVs6EVs6E666666---strips
11.Change in Terminology and Update of Survey and Certification (S&C). (2014, April 29). Retrieved September 25, 2014.
12.Central Sterile Processing. (2012, July 18). . Retrieved August 2, 2014, from http://en.wikipedia.org/wiki/User:Vincentisapirate
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.