Acanthamoeba keratitis: high index of suspicion is key
Acanthamoeba keratitis can be challenging to diagnose, but early detection is critical to prevent severe vision loss. High index of suspicion and use of confocal microscopy are important tools for evaluating patients with keratitis of unexplained origin.

Key Points

"Acanthamoeba keratitis is a sight-threatening infection, but the visual prognosis is improved by early diagnosis. There is a good chance of achieving resolution without corneal scarring if appropriate anti-amoebic treatment can be initiated while the infection is still anterior to the basement membrane," Dr. Sindt said.
The case of a patient with Acanthamoeba keratitis diagnosed after delayed presentation to the University of Iowa Hospitals and Clinic highlights the possibly subtle and nonspecific nature of the early signs and symptoms of the infection and the importance of maintaining a high index of suspicion to facilitate timely intervention in order to achieve a good outcome.
The exam revealed good visual acuity, normal IOP, a clear cornea, 3+ papillae, and 1+ flare. A diagnosis of uveitis was made and treatment with a topical corticosteroid was initiated.
Eluding detection
Over the next week, the patient's condition continued to worsen, despite an increase in the frequency of administration of the topical corticosteroid and initiation of topical antibiotics and a topical antiviral as the diagnosis was eventually changed to bacterial keratitis, punctate keratitis secondary to a foreign body, and herpetic keratitis. Acanthamoeba keratitis was not suspected even though the patient told her optometrist she had been using the recalled contact lens solution and topping off the solution in her lens case.
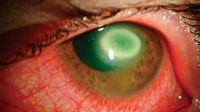
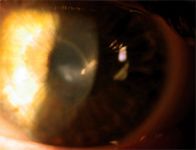
When the patient presented to the university clinic, her findings included limbal flush, 3+ injection, a central stellate lesion with a dendritic pattern, irregular epithelial surface, and Cochet-Bonnet aesthesiometer score of 0.5 cm. The diagnosis of infectious keratitis consistent with Acanthamoeba was made based on the finding of double-walled cysts in the cornea using confocal microscopy. Although included in the differential because of the dendritic pattern and history of relatively long-term corticosteroid treatment, herpetic keratitis was ruled out by polymerase chain reaction testing of a corneal specimen, and the identification of Acanthamoeba cysts on corneal scraping confirmed the diagnosis of Acanthamoeba keratitis.
Despite intensive anti-amoebic treatment, the patient developed a ring infiltrate within several months and progressed to corneal transplantation. After two graft rejections, her final vision was 20/40.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.