Central serous retinopathy helped by NSAIDs
A 27-year-old male whose last eye examination was seven years earlier in India presented to University of Alabama at Birmingham Eye Care for a comprehensive eye examination.
A 27-year-old male whose last eye examination was seven years earlier in India presented to University of Alabama at Birmingham Eye Care for a comprehensive eye examination. He wore no refractive correction but complained of blurry vision at distance for an undetermined period as well as headaches related to prolonged computer activity. He denied eye irritation, burning, itching, watery eyes, flashes, and floaters, as well as diplopia. Review of systems (ROS) was non-contributory. He was oriented to time, place, person with mood and affect appropriate. Family and personal medical histories were similarly noncontributory. He takes no medications and neither smokes nor drinks alcohol. He is currently enrolled in a graduate degree program.
More retina: Diagnosing retinal artery occlusions
Visual acuity without correction was 20/20-2 and 20/25+2 in the right and left eyes, respectively. With minimal myopic refractive correction, visual acuity improved to 20/20 in the right eye but did not improve in the left eye. Applanation pressures were 14 mm Hg in each eye at approximately 11:15 a.m.
Central serous chorioretinopathy

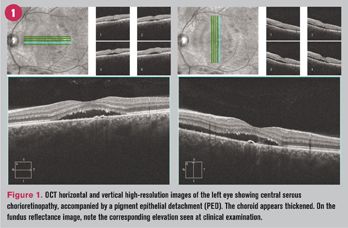
Dilated fundus examination revealed clear lenses and a well-perfused optic nerve head in each eye. The foveal reflex was present in right but replaced by a subtle elevation approximately 2 disc diameter in size in the left eye. The vitreous, vessels, and periphery were unremarkable in each eye. Optical coherence tomography was ordered to determine the extent of the serous elevation in the left eye (see Figure 1). A diagnosis of central serous chorioretinopathy (CSC) was made. Consistent with reported imaging studies of CSC, there is accumulation of material on the detached outer retina. This is thought to represent shed photoreceptor outer segments, engorged macrophages, and other inflammatory debris such as fibrin.1
More retina: Misdiagnosing macular degeneration
The patient was offered a treatment recommendation of a topical non-steroidal anti-inflammatory drug (NSAID) Prolensa (bromfenac ophthalmic solution 0.07%, Bausch & Lomb) for administration once daily to the left eye. Our clinical experience with CSC has been that resolution is hastened by this management strategy. The off-label application was explained to and accepted by the patient. He was asked to return in six weeks.
At the return visit approximately six weeks later, the patient reported good adherence with the treatment regimen and subjective improvement in vision. Visual acuity was 20/20 in each eye, and optical coherence tomography (OCT) demonstrated anatomically resolving serous elevation of the left macula and some diminution of the PED (see Figure 2).
The pathophysiology of CSC is complicated and incompletely characterized.2,3 Numerous risk factors and hypotheses have been advanced and are summarized for the interested reader.3 Although, no consistent management has been demonstrated to be effective in shortening the course,2 our clinical experience has been positive using topical NSAIDs. While it is speculative that this case responded more quickly than spontaneous resolution, offering the patient a potentially beneficial treatment was chosen.
Click here to check out the latest retina news and advice
References
1. Nicholson B, Noble J, Forooghian F, et al. Central serous chorioretinopathy: update on pathophysiology and treatment. Surv Ophthalmol. 2013 Mar-Apr;58(2):103-26.
2. Mrejen S, Spaide RF. Optical coherence tomography: imaging of the choroid and beyond. Surv Ophthalmol. 2013 Sep-Oct;58(5):387-429.
3. Daruich A, Matet A, Dirani A, et al. Central serous chorioretinopathy: Recent findings and new physiopathology hypothesis. Prog Retin Eye Res. 2015 Sep;48:82-118.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.