Chronic ocular diseases and patient psyche
Recently, Dr. Klein asked me to examine one of his long-term rigid gas permeable (RGP) lens-wearing patients. For 2 months, her RGPs became heavily coated after application. Of course, her vision was compromised with debris build-up on her lenses, and her eyes irritated as she cleaned and re-applied the lenses multiple times a day.
Charles Klein, OD, is one of my favorite colleagues. I calculate that he opened his practice when I was in 4th grade. In my role as center director at Omni Eye Surgery in New York, I have had the supreme privilege to share in the care of a number of his patients. Most often, I am preparing and counseling his patients for cataract surgery; generally these patients have been under the careful care of Dr. Klein for decades.
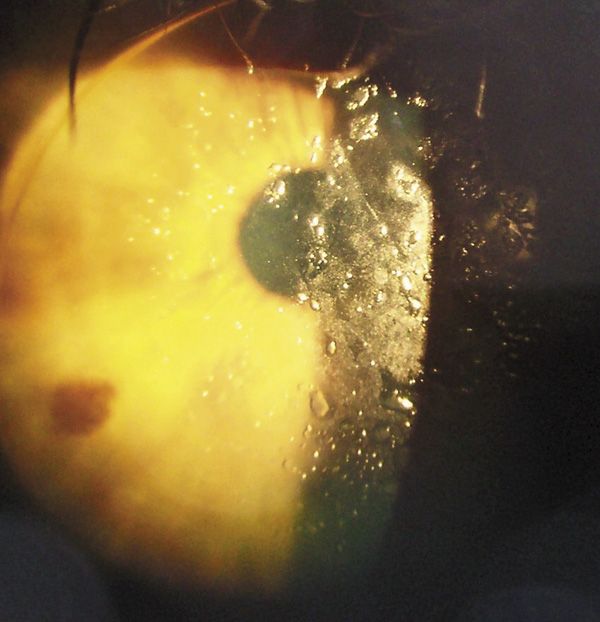
Recently, Dr. Klein asked me to examine one of his long-term rigid gas permeable (RGP) lens-wearing patients. For 2 months, her RGPs became heavily coated after application. Of course, her vision was compromised with debris build-up on her lenses, and her eyes irritated as she cleaned and re-applied the lenses multiple times a day.
Naturally, Dr. Klein addressed each possibility on his clinical checklist to quell the deposition of debris on his patient’s lenses. He replaced her lenses (twice), changed her lens care solutions, changed the lens material, treated her blepharitis and enhanced her tear film with lubricants, and added aggressive lid hygiene.
Yet, on the day she first visited my office, her lenses, wearing them only since that morning, looked as if they were in her eyes for weeks, and her vision hovered around a poor 20/50. She was extraordinarily frustrated and, more importantly, frightened because she had a family history of blindness and significant eye disease.
My examination mirrored Dr. Klein’s. There was no obvious reason that this patient should be having such trouble. Was it meibomian gland dysfunction? Was it allergy? Was it RGP related? Was it something else?
Beauty products, ugly side effects
I surmised that either one, or more likely a combination of these factors, instigated the delicate conjunctiva resulting in mucin deposition. Alternately, this lady did have bilateral ptosis and was rather fond of mascara that settled on her lid margin.
She had been using her current mascara for about 4 months. Mascara can contain different oils and waxes: sesame oil, mineral oil, linseed oil, castor oil, eucalyptus oil, lanolin, or oil of turpentine can be found most frequently among the many formulas. Waxes usually found in mascara are paraffin wax, carnauba wax, and beeswax.
So, long story short, I treated her for “inflammation/irritation” of the ocular surface. For one week’s time I prescribed prednisolone acetate 1%, discontinuation of RGP wear (which made this hyperope very unhappy), and a change of mascara. She returned in 2 weeks 100% better and with crystal clear RGPs.
I still am not sure what was core to this patient’s problem, or if it will return. What I do know is what she said when things had improved-for the past few months with her variable vision and vague discomfort she was extraordinarily irritable and depressed.
She retired early each night to avoid her eye problem or to obviate a short-tempered, inappropriate remark to her significant other. She was frustrated and disagreeable. Additionally, she suffered from uncharacteristic frequent headaches.
Something was acutely amiss with this patient’s ocular surface-imagine the patient with chronic disease. Headaches and depression have been documented in ocular surface disease (OSD) patients. This patient’s case was a dramatic reminder of the impact of dry eye disease and OSD on a patient’s psyche.ODT
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.