Comparing laser-assisted vs. conventional refractive cataract surgery
Cataract surgery is one of the most commonly performed medical procedures and the leading diagnosis for outpatient surgery visits (3 million) in the U.S. In the past decade, the introductions of presbyopic and toric intraocular lenses (IOLs) have elevated cataract surgery into a refractive procedure. The latest introduction of femtosecond laser-assisted cataract surgery may further improve the predictability and safety of refractive cataract surgery and enhance refractive outcomes.
is one of the most commonly performed medical procedures and the leading diagnosis for outpatient surgery visits (3 million) in the U.S.1 In the past decade, the introductions of presbyopic and toric intraocular lenses (IOLs) have elevated cataract surgery into a refractive procedure.
The latest introduction of femtosecond laser-assisted cataract surgery may further improve the predictability and safety of refractive cataract surgery and enhance refractive outcomes.
Numerous studies have documented that laser-assisted cataract surgery can increase precision and reproducibility of the anterior capsulotomy,2-4 reduce effective phacoemulsification time,2,5,6 cause less anterior chamber inflammation post-operatively,7 and potentially lessen surgically induced endothelial cell damage8 as compared with conventional cataract surgery.
All these factors associated with laser-assisted cataract surgery may further enhance the safety profile and visual outcomes of the current conventional cataract procedure.
Any new medical technology needs to be vetted in a real-life clinical setting to see if the results justify the extra out-of-pocket fees patients incur for the elective laser-assisted refractive portion of the surgery.
One study found no difference in visual outcomes between laser and conventional cataract surgery with the ReStor (Alcon) IOL.9 Another study found statistically significant improvement in mean spherical equivalent after implantation of different monofocal IOLs with laser vs. conventional surgery.10
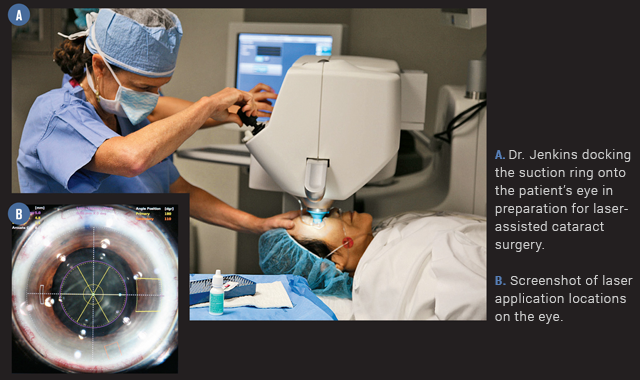
For this study, we compared a single surgeon’s post-operative refractive outcomes of premium patients six months prior to the availability of laser-assisted surgery (August to December 2011) and six months after starting laser-assisted cataract surgery (August 2012 to January 2013).
Study method
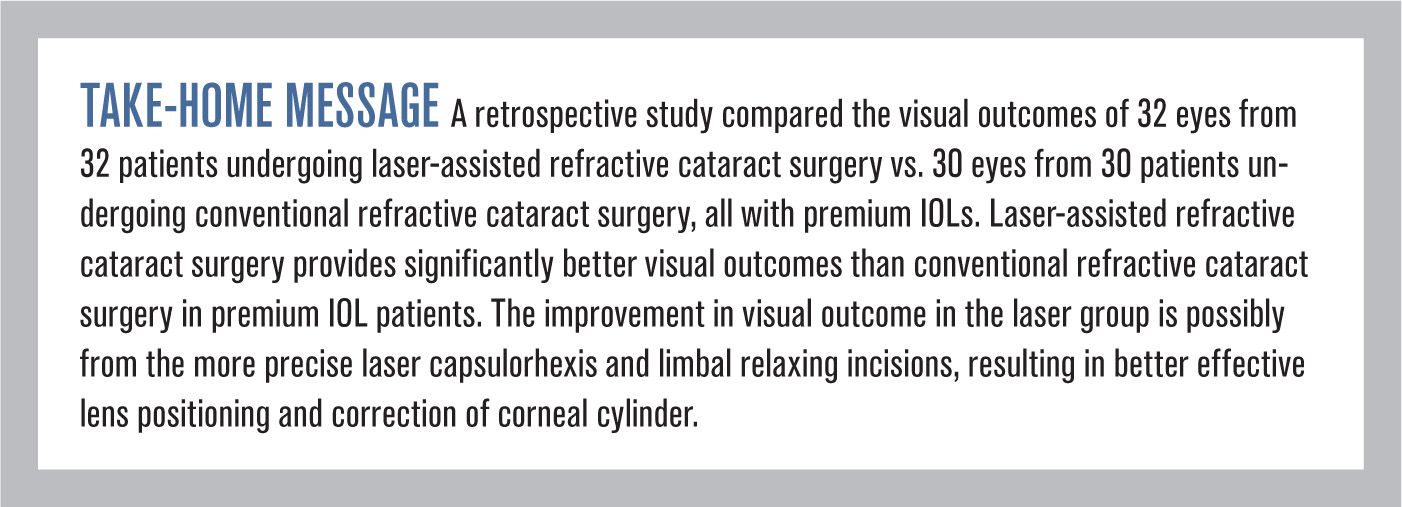
This was a retrospective study that compared the visual outcomes of 32 eyes from 32 patients undergoing laser-assisted refractive cataract surgery with Alcon LenSx (laser group) vs. 30 eyes from 30 patients undergoing conventional refractive cataract surgery (conventional group), all with implantation of premium IOLs-e.g. Alcon AcrySof IQ Toric IOL (Toric), Alcon ReStor IOL (ReStor), and AMO Tecnis Multifocal IOL (TMF)-by the same surgeon, TJ. The primary outcomes were refractive measures mean spherical equivalent (MSE) and uncorrected logMAR acuity at one-month post-op.
Factors such as age, sex, axial length, pre-operative corneal keratometry, and IOL types were assessed to ensure similarity between the two groups. Statistical analysis was performed using the two-sample T-test and Mann-U test.
Inclusion criteria were only one eye per subject was eligible, only subjects who received a premium IOL were included, and their target distance correction had to be plano.
Exclusion criteria were the presence of any macular abnormality, corneal dystrophy or degeneration, pseudoexfoliation, or a history of corneal surgery-LASIK, PRK, CK, or RK/AK.
Results of the study
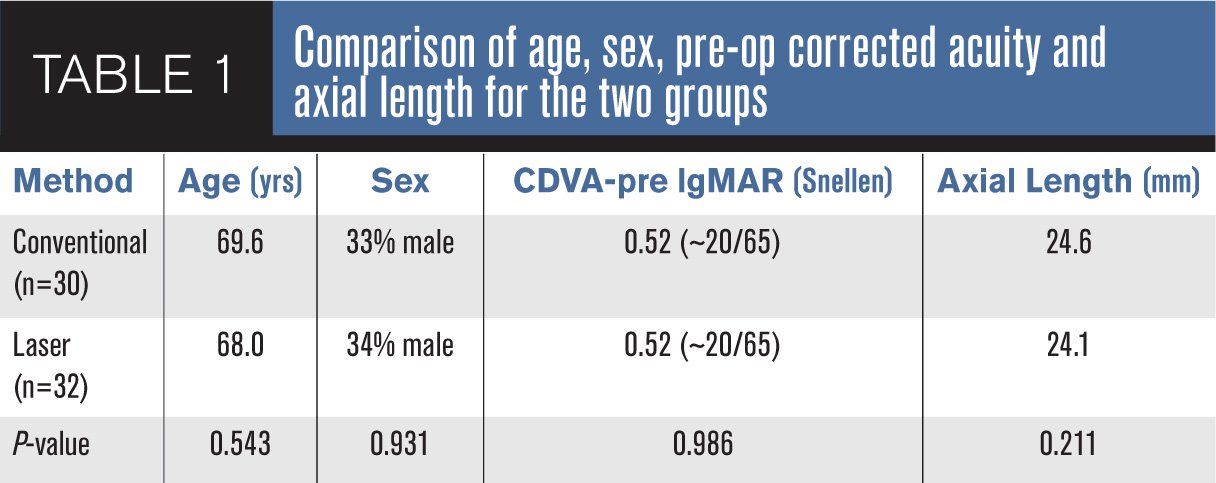
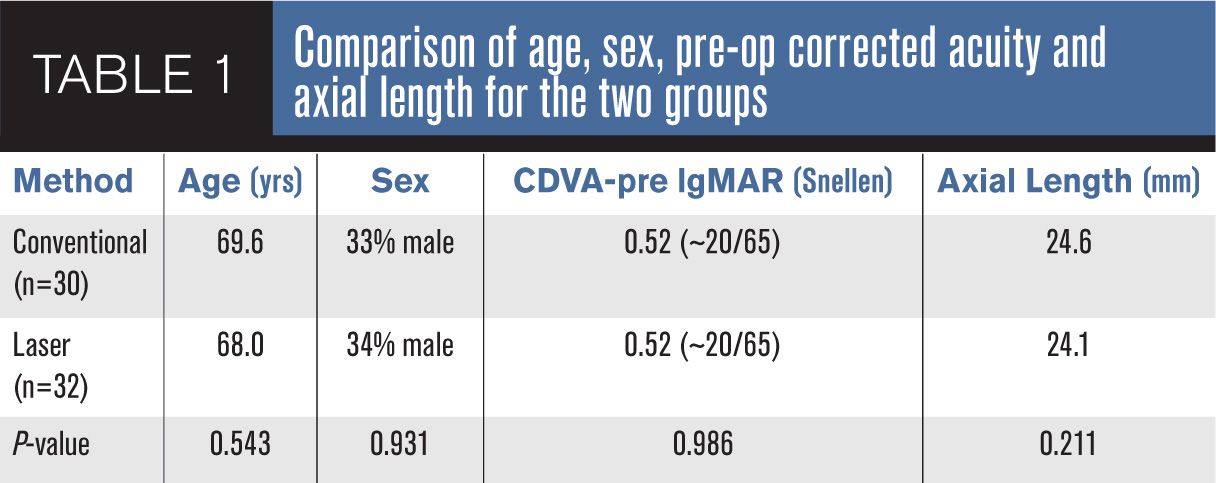
No significant difference was found in age, sex, axial length, or corrected visual acuity prior to surgery (CDVA-pre) between the laser and conventional groups (p-value > 0.05) (Table 1).
One month after surgery the residual manifest refraction, as measured by MSE, was statistically significantly less in the laser group at +0.02+0.33 D as compared with the conventional group at -0.19+0.43 D (p-value = 0.032). Similarly, the uncorrected visual acuity as measured with logMAR was overwhelmingly better in the laser group at 0.06+0.06 (approximately 20/20-3 Snellen) vs. 0.17+0.13 (approximately 20/30 Snellen) for the conventional group (p-value < 0.001).
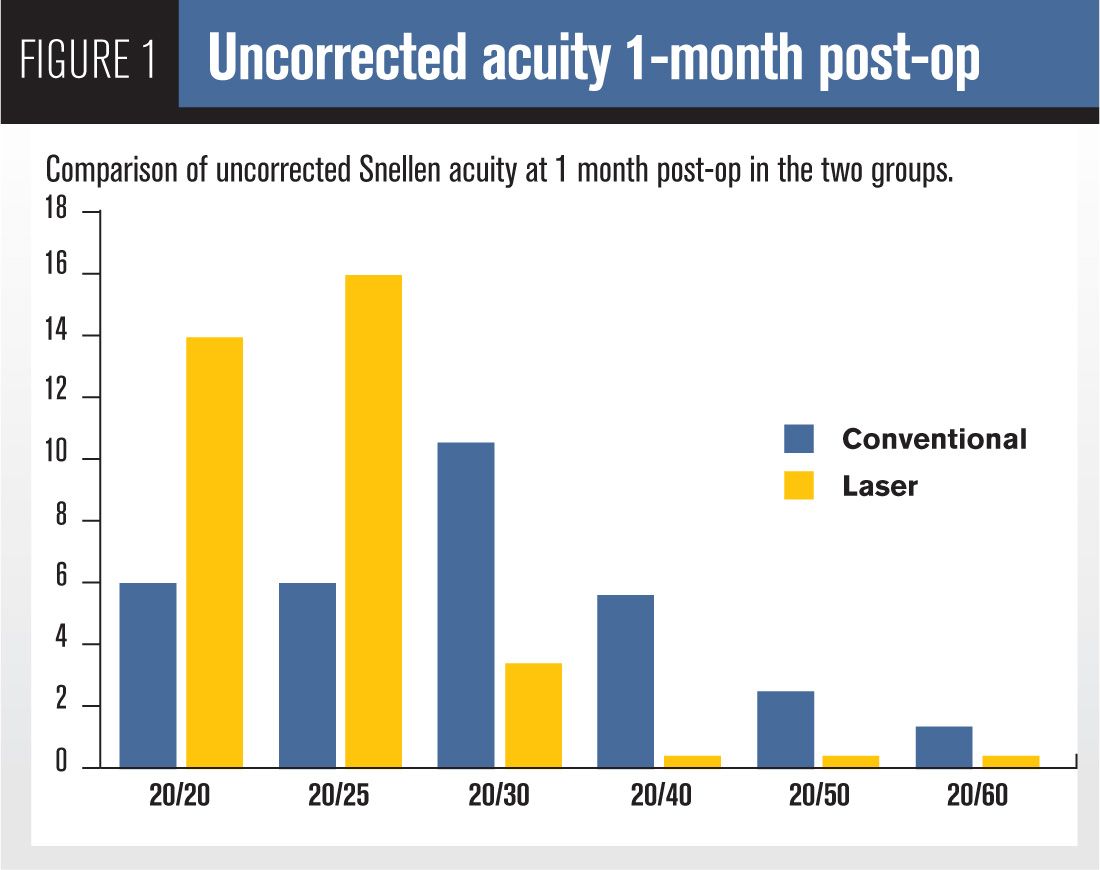
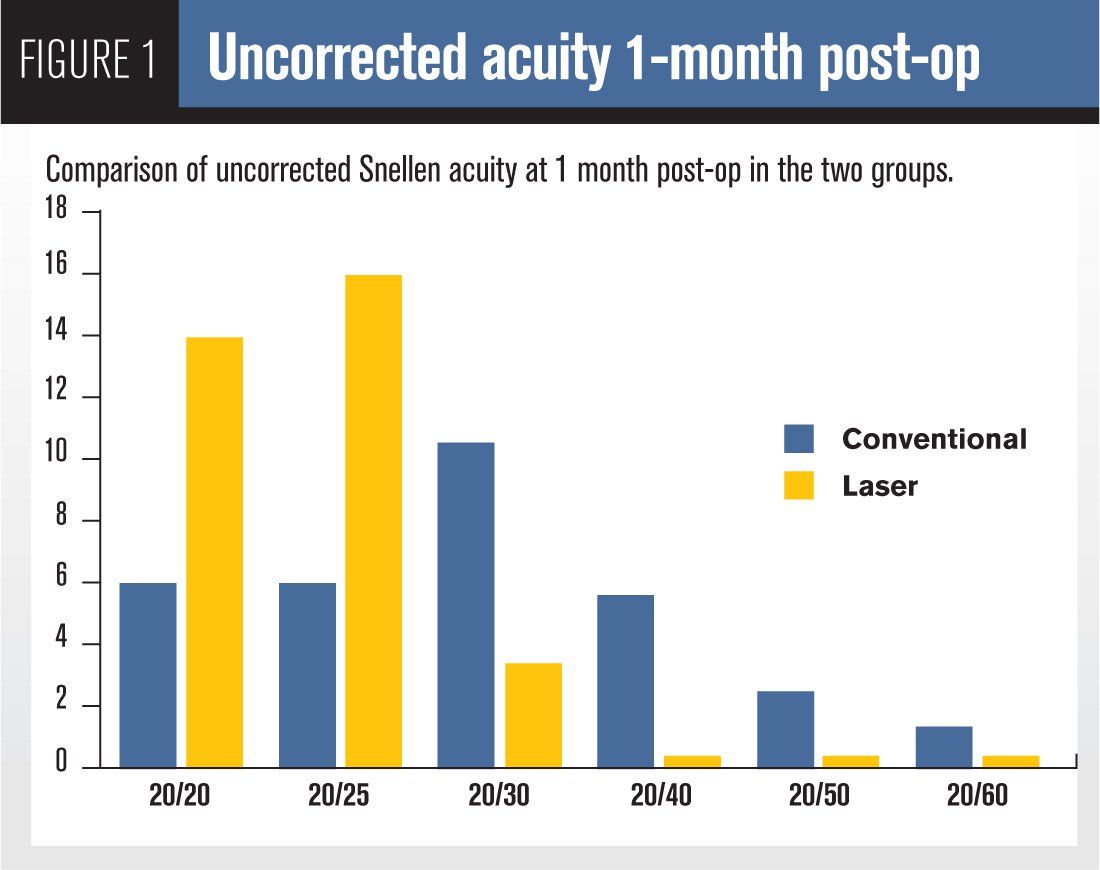
More than twice as many patients achieved 20/25 and 20/20 uncorrected vision at one-month post-op in the laser group as compared to the conventional group (Figure 1).
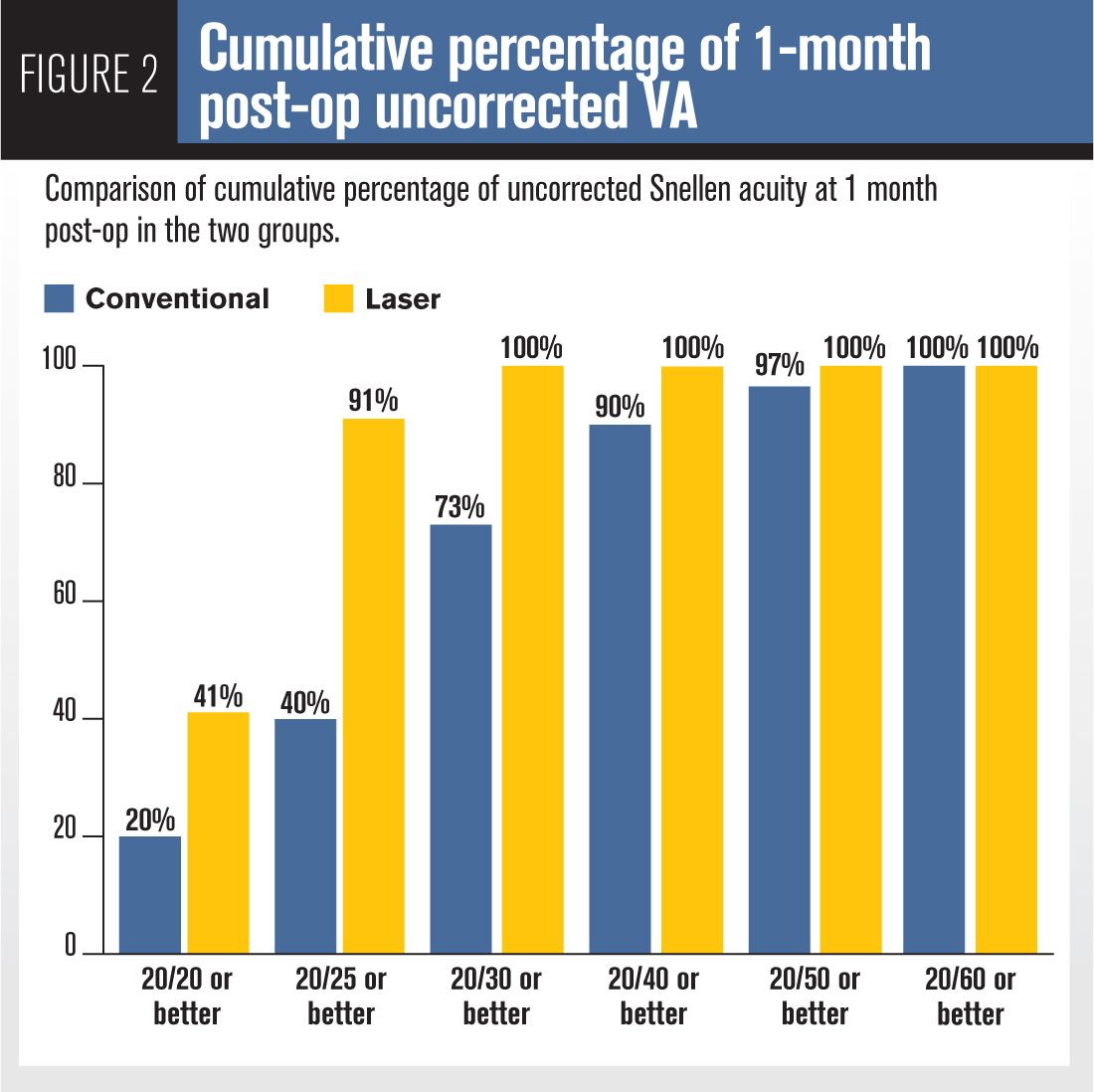
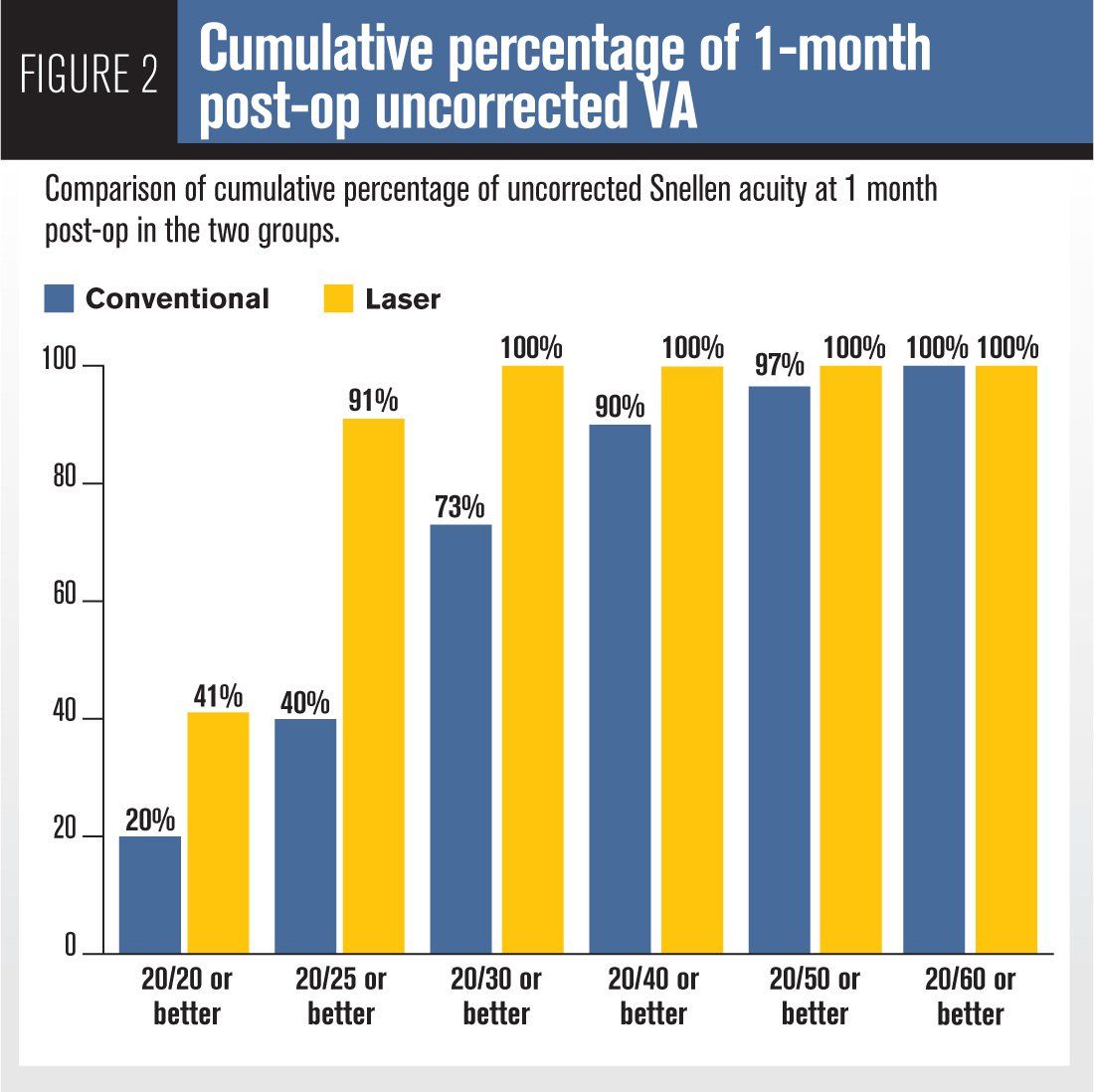
Ninety one percent of the laser group achieved 20/25 or better vision at one-month post-op as compared to only 40 percent in the conventional group (Figure 2).
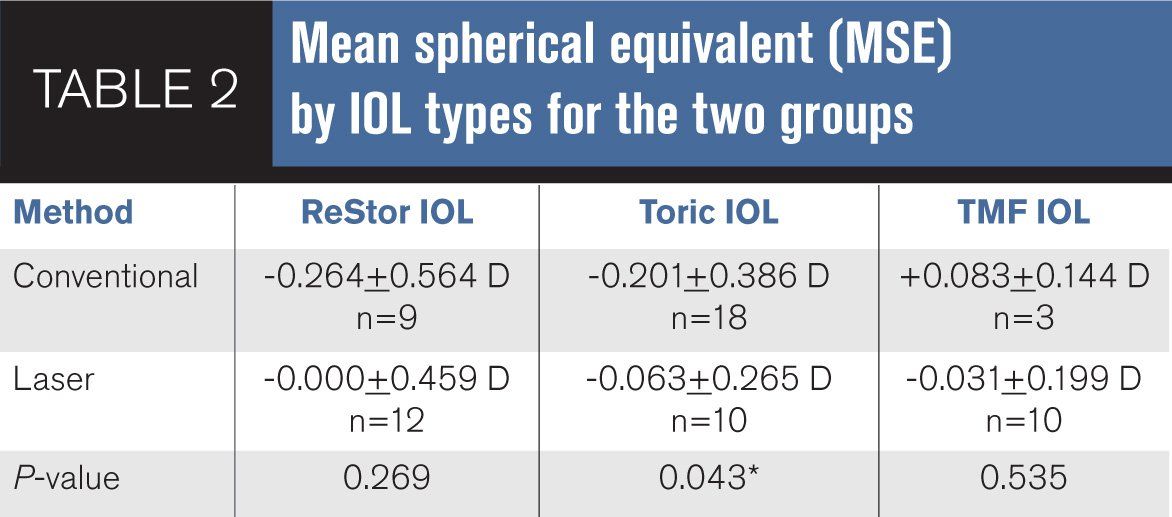
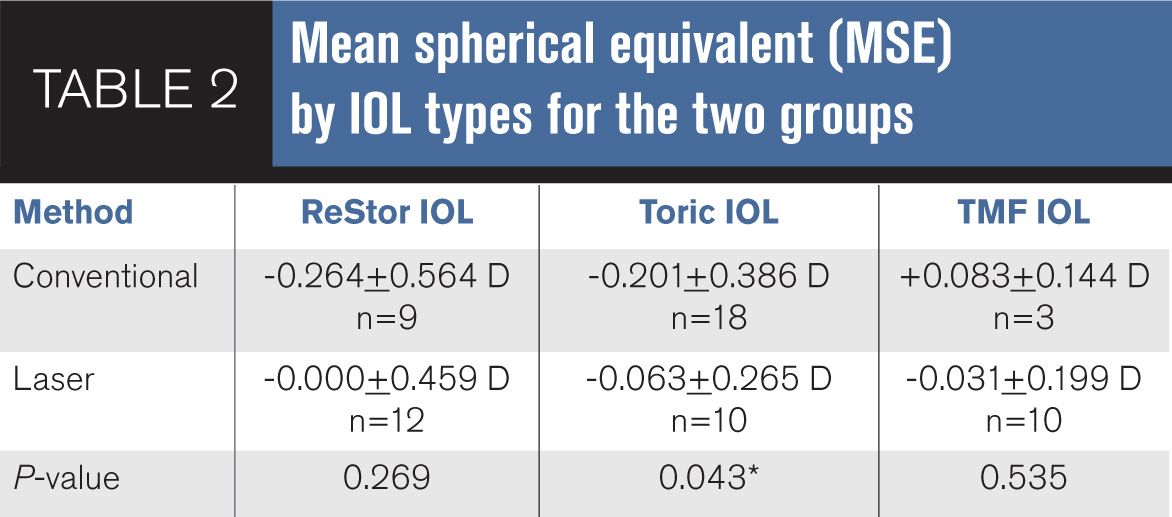
Analysis by IOL type elucidated that the toric IOL subgroup drove the difference found in visual outcome (MSE) between the laser and conventional groups (Table 2).
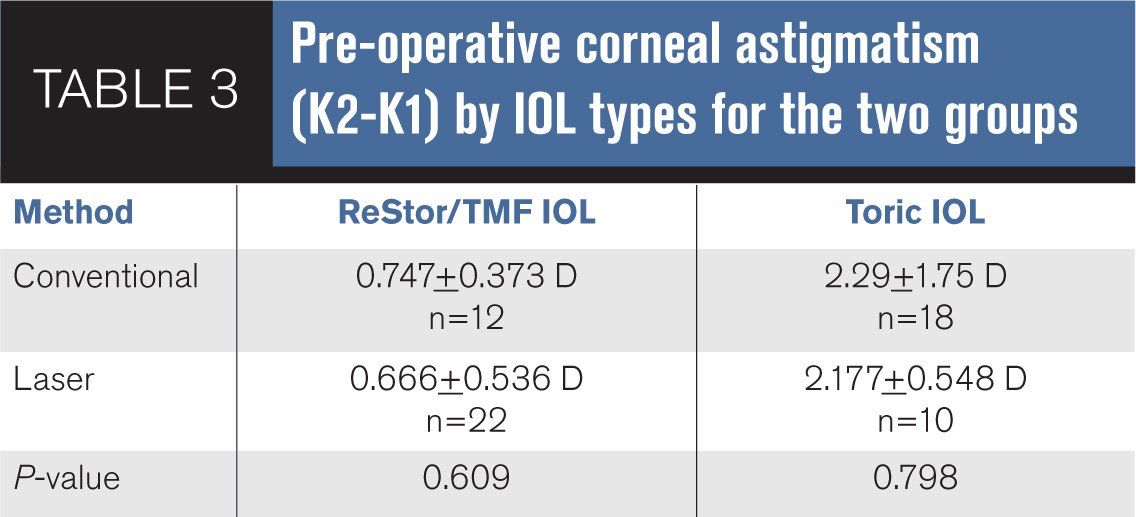
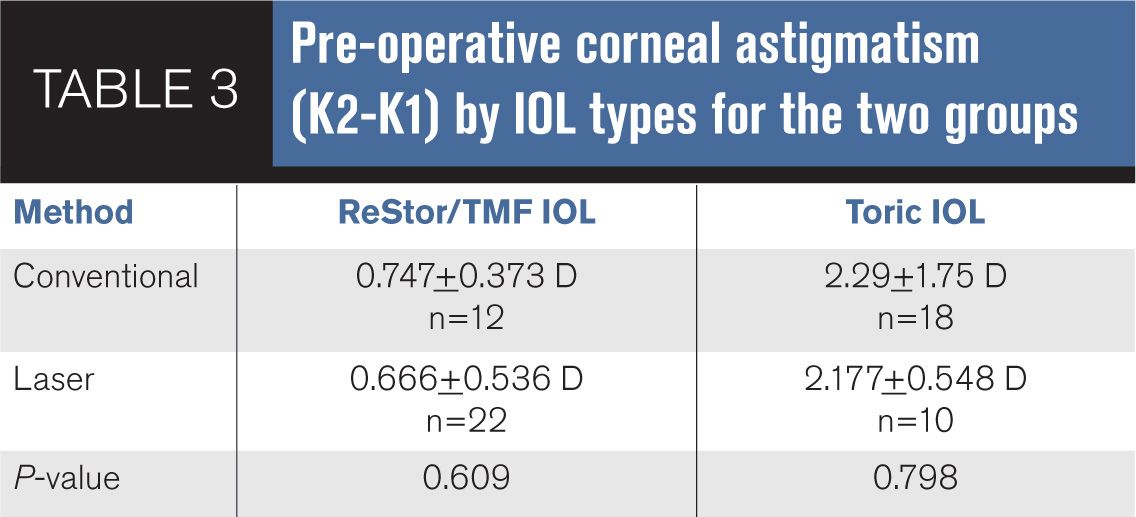
Pre-operative corneal astigmatism, K2-K1, was not significantly different between the two groups within the same IOL category (Table 3).
Because only three patients in the conventional group chose TMF, the ReStor and TMF groups were combined for this analysis.
Discussion
Evidence has been mounting since the introduction of femtosecond laser-assisted cataract surgery surrounding its superiority compared to conventional surgery in the creation of a more precise capsulotomy,2-4 reduced intraoperative ultrasound energy use (equivalent phacoemulsification time),2,5,6 reduced anterior chamber cells and flare post-operatively,7 and potentially lessened surgically-induced endothelial cell damage.8
However, there has been less consistent evidence regarding the visual outcomes of the femtophaco procedure, with some studies citing little to no improvement in refractive outcomes with femtophaco vs. conventional cataract surgery.9,10
In our study, the visual and refractive impact of laser-assisted cataract surgery was evaluated only in patients who elected to have refractive cataract surgery as confirmed by their choice of a premium IOL.
We did not want to accidentally compare non-refractive patients in the control group, who had a standard IOL, and compare them to those who had laser-assisted surgery with standard IOLs in the study group. By comparing only patients who elected for premium IOLs in both the control and laser groups, this eliminated a potential source of error.
This study’s design reflected the real-life application of laser-assisted technology in our clinic. This was in contrast to Filkorn et al’s study that looked at refractive outcomes after laser-assisted (LenSx) vs. conventional cataract surgery in patients who had monofocal IOLs (and some toric IOLs).10
Their study was standardized so all patients had the same corneal incision size and placement regardless of the patient’s own corneal cylinder and axis. No astigmatic keratometry or limbal relaxing incisions were performed on any of their patients.
Thus their refractive outcomes do not fully reflect the capabilities of laser-assisted cataract surgery because corneal cylinder correction was not even attempted.
Despite this limitation, their study still found statistically significant better refractive outcomes as measured by mean absolute error (difference between the predicted and achieved post-op spherical equivalent refraction) in the laser group than the conventional group at six-weeks post-op.
This was in contrast to our study during which the surgeon customized each patient’s corneal incisions to minimize residual corneal cylinder in in both control and study groups.
Because this was a retrospective study, the case and control groups were selected to minimize bias. Analysis of the two groups by age, sex, axial length, and corrected visual acuity prior to surgery (CDVA-pre) found them to be statistically identical.
Only consecutive patients with the required inclusion criteria and none of the exclusion criteria were enrolled during the six months before and after the availability of the femtosecond laser.
The first six months of laser-assisted patients were not included because they reflect data during the surgeon’s learning curve while developing surgical technique, experience, and nomogram with the new technology.
This was in contrast to Lawless et al study that reported on the first 61 consecutive eyes treated with LenSx system as compared to a retrospective control group.9
They found no significant post-operative refractive difference between the two groups but did report, “a greater percentage of eyes achieved 20/25 or better UDVA in the laser cataract surgery group as compared to the manual phacoemulsification group.”
Our study improved on the design of Lawless et al’s by comparing a single surgeon’s results after the first 100 laser cases, well past her learning curve on the laser system.11
This study confirmed that femtosecond laser technology significantly enhanced the visual outcomes of patients undergoing refractive cataract surgery with premium IOLs.
As the improvement was mainly seen in the toric IOL group, it is likely that the increased precision associated with laser limbal relaxing incisions played a large role in the improved visual and refractive outcomes. It has been reported that femtosecond laser-created limbal relaxing incisions are more stable due to a more reproducible generation of squared incisions and multiplanar configuration.12
The documented improved IOL centration and less IOL tilt associated with femtosecond laser-created continuous curvilinear capsulorhexis vs. a manually made capsulorhexis may play a secondary role in the better visual outcome.2-4,13
This finding of more predictable astigmatism correction with laser-assisted cataract surgery has changed our clinical guidelines when offering a multifocal IOL option for patients with higher corneal cylinder.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.
