Comparison of visual, optical acuity in monofocal IOLs
Investigators analyzed IOLs based on optical and visual quality to determine how well patients can function during challenging visual tasks, dim lighting, glare conditions, or reduced contrast.

Special to Optometry Times®
Contemporary monofocal intraocular lenses (IOLs), which are implanted in the vast majority of cataract surgery cases performed in Spain and throughout Europe, provide excellent visual results for our patients.
Historically, these IOLs have been evaluated based on their safety index, predictability, and efficacy in achieving 6/6 visual acuity.
Poyales

However, it is no longer sufficient to simply compare acuity or the quantity of vision. All of these IOLs perform well for viewing a high-contrast eye chart under photopic conditions in the clinic.
To determine how well patients will function during more challenging visual tasks or in dim lighting, glare conditions, or reduced contrast, we must also evaluate IOLs based on their optical and visual quality.
Optical quality and visual quality, while related, are different concepts. Optical quality is an objective metric that refers to the quality of the retinal image; it can be affected by light scatter, diffraction, or ocular aberrations.
Although optical quality is often evaluated in vitro in optical bench testing, newer tools such as the Optical Quality Analysis System (OQAS, Visiometrics) make it possible to assess it in vivo.
Visual quality is a subjective metric linked to the patient’s perception of their vision and visual functioning. Visual quality is influenced by both visual quantity and optical quality, but also by psychological factors and neural characteristics.
My colleagues and I recently compared two contemporary monofocal IOLs, the well-established Tecnis ZCB00 (Johnson & Johnson Vision) and the new Clareon CNA0T0 (Alcon), in a randomized, prospective study conducted at our private clinic in Madrid, Spain.1
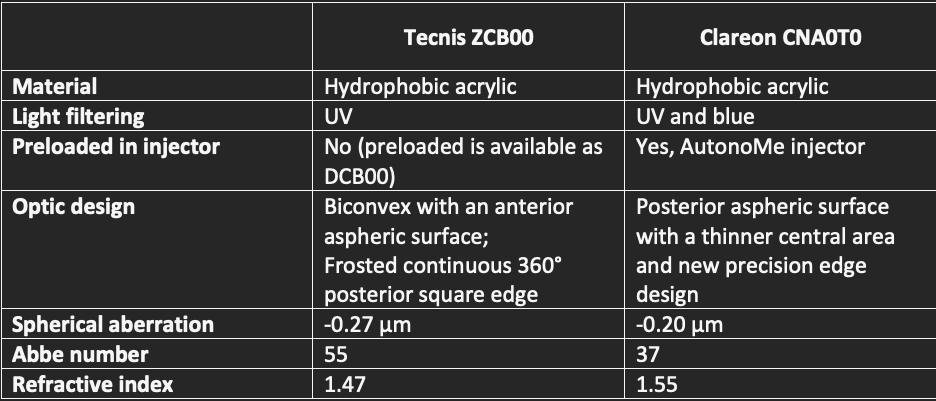
The IOL characteristics of these two lenses are described in Table 1.
Table 1. Lens Features
To be enrolled in the study, subjects had to be at least 50 years old, with good visual potential, no history of eye surgery or trauma, and no comorbidities or abnormalities that might compromise postoperative vision.
All subjects had <1.50 D of with-the-rule (WTR) astigmatism or <1.00 D of oblique or against-the-rule (ATR) astigmatism.
Thirty patients were bilaterally implanted with ZCB00 and 30 with the CNA0T0. There were no significant differences between the two groups preoperatively, except that the ZCB00 group had a slightly deeper anterior chamber depth (ACD) of 3.10 mm versus a 2.94-mm mean ACD in the CNA0T0 group (p=0.040).
For both groups, IOL power was calculated with the Barrett Universal II formula; anterior capsulotomies and nuclear fragmentation were performed with the Catalys femtosecond laser (Johnson & Johnson Vision); phacoemulsification was performed with the Centurion Vision System (Alcon); and the surgeries were computer-assisted with the Callisto Eye System (Zeiss).
Although patients were implanted bilaterally, all postoperative testing (except for a patient questionnaire) was performed monocularly, on right eyes only. There were no surgical or postoperative complications in either group.
Both groups had excellent uncorrected visual acuity but the ZCB00 eyes achieved better distance-corrected acuity (Table 2, see below).
Optical quality
Optical quality was measured in a variety of ways to obtain as complete an understanding as possible.
These included measurement of longitudinal chromatic aberration (LCA) and spherical aberration (SA), the objective scatter index (OSI), Strehl’s ratio (SR), modulation transfer function (MTF) cut-off, and contrast sensitivity (CS) defocus curves. The results are summarized in Table 2.
Table 2: Comparison of Visual Quantity and Optical Quality Results
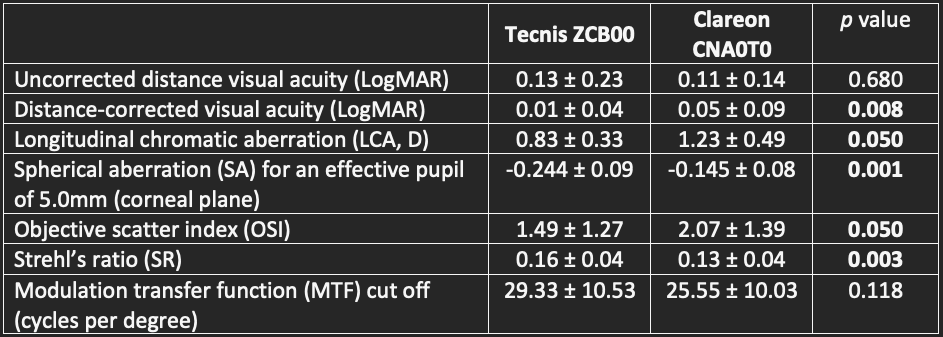
In general, the higher the Abbe number, the lower the chromatic dispersion, so it is not at all surprising that we found lower LCA in the eyes implanted with the ZCB00 lens (Abbe number 55) compared to those implanted with the CNA0T0 lens, which has an Abbe number of 37.
SA varies by pupil size. At a wider pupil of 5.0 mm, there is a statistically significant difference in SA between the two lenses tested; at smaller pupil sizes, this difference is not significant.
Several OQAS measurements, including a high OSI, or a low SR or MTF cutoff, are correlated with patient perceptions of poor visual quality. We found statistically significant differences between the two lens groups on OSI and SR, favoring the ZCB00 lens, but no difference on MTF cutoff.
When we graphed CS defocus curves for 3.0 and 4.5 mm pupils, there was a reduction in CS in the CNA0T0 group at the larger pupil size, whereas in the ZCB00 group, no change was seen from 3.0 to 4.5 mm.
Visual quality
Patients in our study were asked to respond to the CatQuest-9SF questionnaire, which asks questions about their satisfaction with their vision and ability to function for everyday tasks.
While the ZCB00 group rated their satisfaction and function higher than the CNA0T0 group in every category, the differences were only statistically significant for a question about “reading text on television.”
Visual quality is also affected by pupil size, which changes with age. As such, perceptions of quality may change over time with fluctuations in pupil-dependent measures such as SA and CS as patients age.
In summary, while contemporary monofocal IOLs generally provide surgeons with excellent predictability and safety, there are important differences in optical quality and visual quality that should be evaluated and considered for IOL selection.
This study was partially funded by an unrestricted research grant from Johnson & Johnson Vision.
--
About the author
Francesco Poyales, OD
is medical director of Miranza IOA in Madrid, Spain. Contact him at Francisco.poyales@miranza.esm
Reference
1. Poyales F, Garzón N, Rico L, et al. Comparison of visual performance between two aspheric monofocal intraocular lens models. Clin Exp Optom. 2022;Online ahead of print.