The connection between dry eye and eyelashes
While there are a myriad of associated concerns due to ocular surface inflammation, a few eyelash-related complications of note are trichiasis, acquired distachiasis, local madarosis, and poliosis. Each of these is in some way connected to dry eye.
Inflammation. Seemingly the culprit of the times, fingers increasingly point at its connection to everything from heart disease to arthritis. In the eyes, inflammation can lead to tear film instability that can contribute to dry eye. While there are a myriad of associated concerns due to ocular surface inflammation, a few eyelash-related complications of note are trichiasis, acquired distachiasis, local madarosis, and poliosis. Each of these is in some way connected to dry eye.
More dry eye: Treating dry eye with lipid-based eye drops
Trichiasis
A common clinical encounter, trichiasis is usually accompanied by a foreign body sensation. This eyelash abnormality occurs when the cilia arise from the correct anatomical position but are misdirected posteriorly. The etiology of trichiasis include age-related tissue changes and close companions of ocular surface disease-that is, inflammation and the lid margin’s changes in response to it.
More dry eye: Using warm compresses to treat MGD
Mal-positioned eyelashes can lead to ocular irritation, punctate epithelial erosions, corneal thinning, scarring, corneal pannus, decreased vision, and, although rare, corneal perforation.1
For mild cases of trichiasis and ocular inflammation, regular lubrication with artificial tears, lid hygiene, omega supplements, and MiBoFlo ThermoFlo can be considered to restore lid and gland health. For more severe cases, additional therapies such as epilation, anti-inflammatory therapy and other surgical procedures may be required.
Next: Acquired distachiasis
Acquired distachiasis
Acquired distachiasis presents as stunted and flimsy eyelashes originating from the meibomian glands.2 This condition can develop because the meibomian glands and lash follicles differentiate from a common pilosebacious unit, and it is often caused by chronic inflammation.3,4
These sebacious glands are fundamental to preventing tear film evaporation, which is directly related to dry eye. Extended contact lens wear, inflammation, and chronic irritation have all been shown to decrease the number and length of meibomian glands, exacerbating the problem.3
More dry eye: 5 things you don't know about punctal plugs
Specific provoking causes include trauma, chronic irritation to the eyelid margin, chemical injury, Stevens-Johnson syndrome, and ocular cicatricial pemphigoid.1,5
These abnormal lashes can easily be epilated, and the underlying condition should be treated appropriately. Rarely, surgical intervention may be required to relieve patient symptoms.
Next: Local madarosis
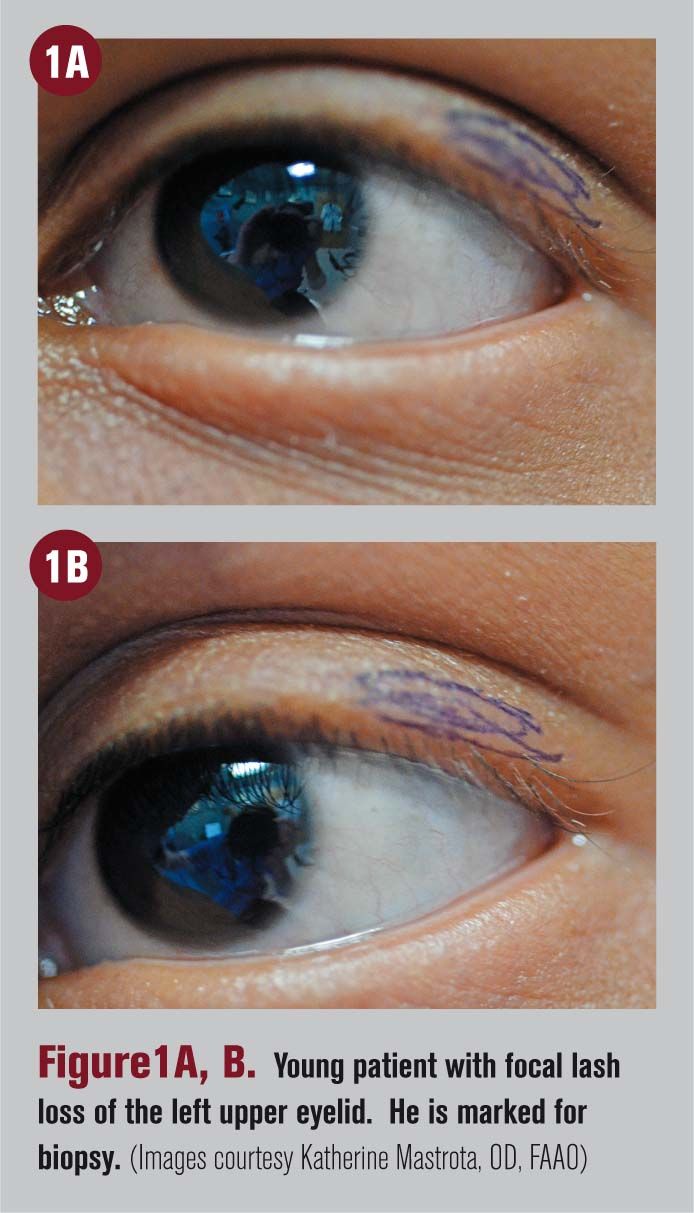
Local madarosis
The term madarosis originates from the Greek word, “madaro,” which means “to fall off.”5 Clinically, madarosis is missing eyelashes in a localized area. Causes of madarosis include chronic blepharitis, atopic keratoconjunctivitis, surgery, and destructive tissue conditions including neoplasms, systemic lupus, icthyosis, endocrine dysfunction, trauma, alopecia, medications, toxicity, drug abuse, radiation, or chemotherapy. 2,4,5
When evaluating hair or lash loss in patients, it is important to determine whether or not the hair loss is localized to the eyelids. In this way, underlying pathology can be more accurately diagnosed.
More dry eye: A stepwise approach to treating MGD
Ocular poliosis
This cilia abnormality describes premature, localized, whitening of the eyelashes. Ocular poliosis is caused by chronic anterior blepharitis, idiopathic uveitis and sympathetic ophthalmitis.2
Take a good look
Early identification and management of eyelash abnormalities can improve the patient's quality of life. Successful treatment will ultimately decrease inflammation, improve tear film quality, and reduce the occurrence of dry eye.
Click here to read the latest dry eye advice from your colleagues
References
1. Bartlett JD, Jaanus SD. Clinical Ocular Pharmacology. 3rd ed. Butterworth-Heinemann, Boston; 1995.
2. 4. Kanski JJ. Clinical Ophthalmology: A Systematic Approach. 6th ed. Elsevier Limited, Edinburgh; 2007.
Remington LA. Clinical Anatomy and Physiology of the Visual System. 3rd ed. Butterworth-Heinemann, St. Louis;2012.
3. Kaiser P, Friedman N. The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. 4th ed. Lippincott Williams & Wilkins;2012.
5. Kumar A, Karthikeyan K. Madarosis: A marker of many maladies. Int J Trichology. 2012 Jan;4(1):3-18.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.