Corneal inlay technology offers new advantages
Corneal inlays to correct refractive errors are not new-various materials have been tried for more than 50 years to correct blurred vision. The greatest barriers to success of corneal inlays have been a lack of biocompatibility with the cornea, the difficulty of placing them within the corneal stroma safely, and refractive predictably.
Corneal inlays to correct refractive errors are not new-various materials have been tried for more than 50 years to correct blurred vision. The greatest barriers to success of corneal inlays have been a lack of biocompatibility with the cornea, the difficulty of placing them within the corneal stroma safely, and refractive predictably.1
More recently, several attempts at correcting hyperopia with corneal inlays failed primarily due to difficulty changing the anterior curvature of the cornea while maintaining a healthy cornea. Deep placement of the inlays was able to maintain corneal physiology but had little to no effect on anterior curvature.2
New technology, presbyopia focus
Femtosecond lasers have revolutionized the ability to create smooth precise pockets into the corneal stroma at specific depths to place corneal inlays. Additionally, advances in material biocompatibility and manufacturing technology to produce highly permeable hydrogel polymers and ultra-thin corneal inlays have contributed to the success of current generation corneal inlays.
More from Dr. Tullo: Quality of life after LASIK
Presbyopia is the most common refractive error with an estimated more than 2.1 billion people affected worldwide by 20202 with 80 million adults between 45 and 64 years old in the U.S. There are more than 11 million estimated emmetropic presbyopes currently in the U.S.3
Corneal inlays are placed in the non-dominant eye at a specific depth within a femtosecond laser created pocket in the corneal stroma. The surgical procedure is fast, typically less than 10 minutes, and is performed under topical anesthesia. The inlay is carefully centered over the visual axis to maximize the optical effect and minimize visual side effects such as blur, diplopia, and loss of best-corrected vision.
Next: 3 approaches to reading correction
3 approaches to reading correction
The first approach is found in the investigational device called the Raindrop Near Vision Inlay (ReVision Optics). Raindrop is a transparent plano non-refractive hydrogel inlay, 2.0 mm in diameter and 32 µm thick, that is inserted in the anterior corneal stroma (130-150 µm deep) under a flap created with a femtosecond laser. It alters the eye’s refractive power by increasing the central radius of curvature of the anterior cornea. The goal of this inlay is to produce a hyperprolate shape, which results in an aspheric multifocal effect with minimal disruption to distance vision.
More from Dr. Tullo: Identifying candidates for non-corneal refractive surgery
The second approach uses concentric optics and is called Flexivue Microlens (Presbia Cooperatief U.A.) Flexivue is still investigational in U.S. A small 1.8 mm diameter, 15-20 µm thick transparent methacrylate copolymer with a central plano zone and peripheral annular near zone of specific power (+1.25 D to +3.00 D) is implanted in an intrastromal pocket 280-300 µm deep. It incorporates a central 0.15 mm hole to facilitate the transfer of oxygen and metabolites to maintain normal corneal physiology. Similar to concentric design contact lenses, patients must adapt to the simultaneous images on the retina of the non-dominant eye.
The third approach is the only U.S. Food and Drug Administration (FDA)-approved device for the correction of near vision blur called the Kamra Inlay (AcuFocus). AcuFocus uses a hyperthin microperforated aperture to increase depth of focus. Kamra is a single piece of polyvinylidene fluoride (PVDF), with 3.8 mm diameter opaque (carbon black) annulus, a 1.6 mm transparent central hole, and is 6 µm thick. The inlay is perforated with 8,400 holes randomized from 5.5 to 11.5 µm in size to allow for transport of metabolites to maintain the health and integrity of the cornea.
Next: More on Kamra
More on Kamra
Recent U.S approval specifies that the Kamra inlay is indicated for the improvement of near vision by extending the depth of focus in the non-dominant eye of phakic presbyopia patients between the ages of 45 and 60 years old with refractive error +0.50 D to -0.75 D with ≤ 0.75 D of refractive astigmatism.3 Additionally, patients must not be wearing glasses or contact lenses for distance vision and have near correction between +1.00 D and +2.50 D. Kamra is placed in a femtosecond laser-created intrastromal pocket 220 µm or deeper. Outside the U.S., it is not uncommon to create a pocket 100 µm below a previously created LASIK flap for Kamra. Patients with a refractive error of -0.75 D to -1.00 D seem to have the best results due to optimal placement of the range of depth of focus provided by the artificial pinhole.
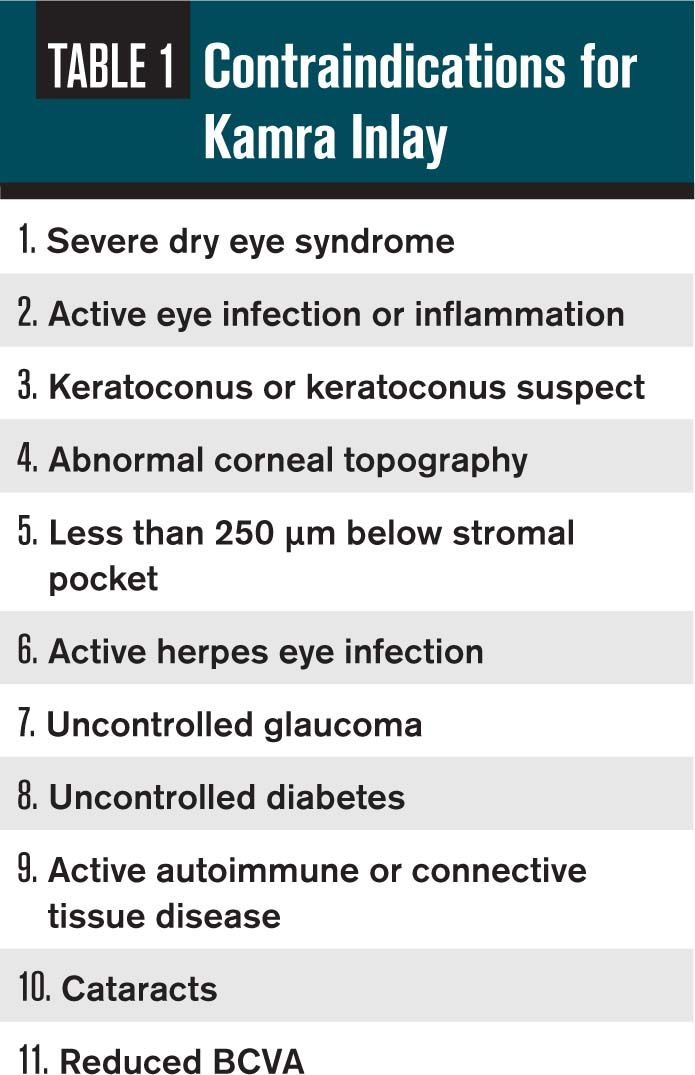
Contraindications and complications of the Kamra inlay are summarized in Tables 1 and 2. Because Kamra does not split light, it does not interfere with normal binocular summation, requiring less neuroadaptation than monovision correction.
While approved only for natural emmetropes in the U.S., more than 20,000 Kamra inlays have been implanted in pseudophakes and post-LASIK emmetropes, and performed in combination with other refractive surgeries to provide improved near vision in more than 50 countries outside the U.S.
More from Dr. Tullo: Comanaging non-corneal refractive surgery
Very little peer-reviewed literature is available for Flexivue Microlens and Raindrop. More than 29 clinical studies are currently published on Kamra, showing:
• Reading speed and acuity are significantly improved after inlay implantation6
• Post-inlay implantation patients are able to read at a significantly closer reading distance6
• Visual field is unaffected6
• Kamra doesn’t affect ocular assessments6
• Cataract surgery is possible with the inlay in place7
Next: Inlay advantages and disadvantages

Inlay advantages and disadvantages
The biggest advantage of corneal inlays is the reduction of dependence on reading glasses. The fact that they are additive and do not remove any tissue from the cornea enhance their safety profile as compared to ablative laser vision correction procedures. Other key advantages include:
• Easy removability
• Not an intraocular procedure
• Maintenance of contrast acuity
• Extended range of vision.
The biggest disadvantage of corneal inlays is the mild-moderate loss of distance vision (one to two lines uncorrected distance vision (UCDV) that can occur in the non-dominant eye. Additionally, the dry eye that often accompanies the inlay can lead to fluctuating vision and patient dissatisfaction. Some patients also require prolonged use of topical steroids, increasing the risk of IOP spikes.
In the FDA study of 508 eyes implanted with the Kamra inlay, 83.5 percent achieved uncorrected near visual acuity (UCNVA) of 20/40 (eight-point font) or better at 12 months in the implanted eye, representing an average of three lines of vision improvement.3 About three percent of the enrolled patients with a modern femtosecond pocket had the inlay removed, mostly due to a hyperopic refractive shift affecting distance vision in the implanted eye.3
Next: Patient selection, follow up
Patient selection, follow up
An ideal patient has mild myopia (-0.75 D to -1.00 D) with -0.50 D or less astigmatism, a good tear film with no dryness symptoms, and an easy-going personality willing to tolerate common visual symptoms associated with inlay. AcuTarget HD, a new device from AcuFocus, may also assist with patient selection by measuring intraocular light scatter and evaluating subtle lenticular opacities not evident on slit lamp examination that may cause reduced patient satisfaction with Kamra. AcuTarget HD also helps determine visual axis and pupil center, allowing precise centering of the Kamra inlay, necessary for best visual performance.
Post-operative medications include topical antibiotics for one week (similar to LASIK) and topical steroids for one-month taper (similar to PRK). Additional testing includes checking uncorrected near vision OD, OS, OU, and distance corrected near vision OD, OS, OU. AcuFocus also recommends a midpoint refraction-midpoint between maximum plus to blur and maximum minus to blur at distance-in the implanted eye.
More from Dr. Tullo: Measuring LASIK patient satisfaction
Other surgical options for the correction of presbyopia in the U.S. include LASIK or PRK monovision and multifocal/accommodating IOLs. Problems such as reduced distance and near vision, reduced stereopsis, reduced contrast sensitivity, and poor quality of vision has limited these options for our patients.
Hopefully, the addition of the first corneal inlay will expand the options for patients with blurred near vision. Due to the less invasive nature of the corneal inlay procedure and its reversibility, it is even possible that corneal inlays may serve as a bridge for patients who are not ready for the intraocular placement of an IOL.
References
1. Binder PS, Lin L, van de Pol C. Intracorneal Inlays for the Correction of Ametropias. Eye Contact Lens. 2015 Jul;41(4):197-203.
2. Lindstrom RL, Macrae SM, Pepose JS, et al. Corneal Inlays for presbyopia correction. Curr Opin Ophthalmol. 2013 Jul;24(4):281-7.
3. AcuFocus KAMRA Inlay US FDA Ophthalmic Devices Committee June 6, 2014. Available at http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/MedicalDevices/MedicalDevicesAdvisoryCommittee/OphthalmicDevicesPanel/UCM400439.pdf. Accessed 07/13/2015.
4. Alarcon A, Anera RG, Villa C, et al. Vision Quality after Monovision LASIK in presbyopic patients. J Cataract Refract Surg. 2011 Sep;37(9):1629-35.
5. Yilmaz OF, Alagoz N, Azman E, et al. Intracorneal Inlay to Correct Presbyopia: Long-term Results. J Cataract Refract Surg. 2011 Jul;37(7):1275-81.
6. KAMRA. Available at kamra.com. Accessed 07/14/2015.
7. Tan TE, Mehta JS. Cataract Surgery following KAMRA presbyopic implant. Clin Ophthalmol. 2013:7;1899-1903.
8. Dexl AK, Jell G, Strohmaier C, et al. Long-term outcomes after monocular corneal inlay implantation for the surgical compensation of presbyopia. J Cataract Refract Surg. 2015 Mar;41(3):566-75.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.