Effective treatments for presbyopia, myopia, demodex
Pipeline treatments for presbyopia, myopia, and demodex are expanding rapidly
The pharmacologic options in the pipeline for treating presbyopia, myopia, and demodex are expanding rapidly. Milton M. Hom, OD, shared information about the latest advances in these arenas. He is in private practice in Azusa, CA.
Presbyopia
Improving near vision may be the final frontier for vision specialists and the number of patients affected each year is growing by leaps and bounds, with almost 2 billion affected globally. Patients have a number of treatment options currently that include spectacle and contact lens correction and surgical and laser approaches.
The movement now is toward the use of pharmacologics to achieve near vision.
Related: Is presbyopia the newest specialty?
Vuity (Allergan) has recently been approved. Vuity, as well as other drugs in the pipeline, rely on miosis. Smaller pupil increases depth of field and allows presbyopes to see at near.
Some pearls regarding use of this drug are that patients should wear distance correction for the best results; the effect takes place over time, with the initial effect at 15 minutes, a better effect at 1 hour after instillation, and the best effect at 2 weeks. Side effects may include transient headache or ocular redness. The drop can be used with contact lenses.
Another drug with a different mode of action is UNR844 (Novartis), a lipoic acid choline ester, that is a potential first-in-class treatment for presbyopia via lens modulation. The data gathered from the formulation’s use in humans and mice indicate that twice daily administration increases lens elasticity, a key factor in presbyopia.1
Related: New research addresses contact lens myths, misconceptions
Myopia
Myopia is a global epidemic and about 1 billion individuals are at the high end of the myopia spectrum. This is especially concerning with children and the use of electronic devices. Increased outdoor activity may delay myopia onset.
A commonly used treatment that has been receiving attention is instillation of atropine, a nonselective muscarinic that has stopped axial elongation; the mechanism of this activity is unknown.
A number of clinical trials testing different drugs and concentrations have been conducted.
The drugs include NVK002 (Nevakar, Vyluma Inc.), MicroPine (atropine ophthalmic solution, Eyenovia) in concentrations of 0.1% and 0.01%, and SYD-101 (Sydnexis) in concentrations of 0.01% and 0.03%).
While atropine is most effective at high doses, resultant photophobia reported in 100% of patients results in patient dropout rates of 16% to 58%2 and in very low concentrations the drug can be unstable.
Early studies found that atropine reduces axial length progression by 80% and compared with controls, the mean myopia progression was significantly lower with atropine use.3
Evidence supports the use of atropine in conjunction with multifocal contact lenses, orthokeratology, and spectacles.4
Related: Welcoming myopia modalities into optometric practice
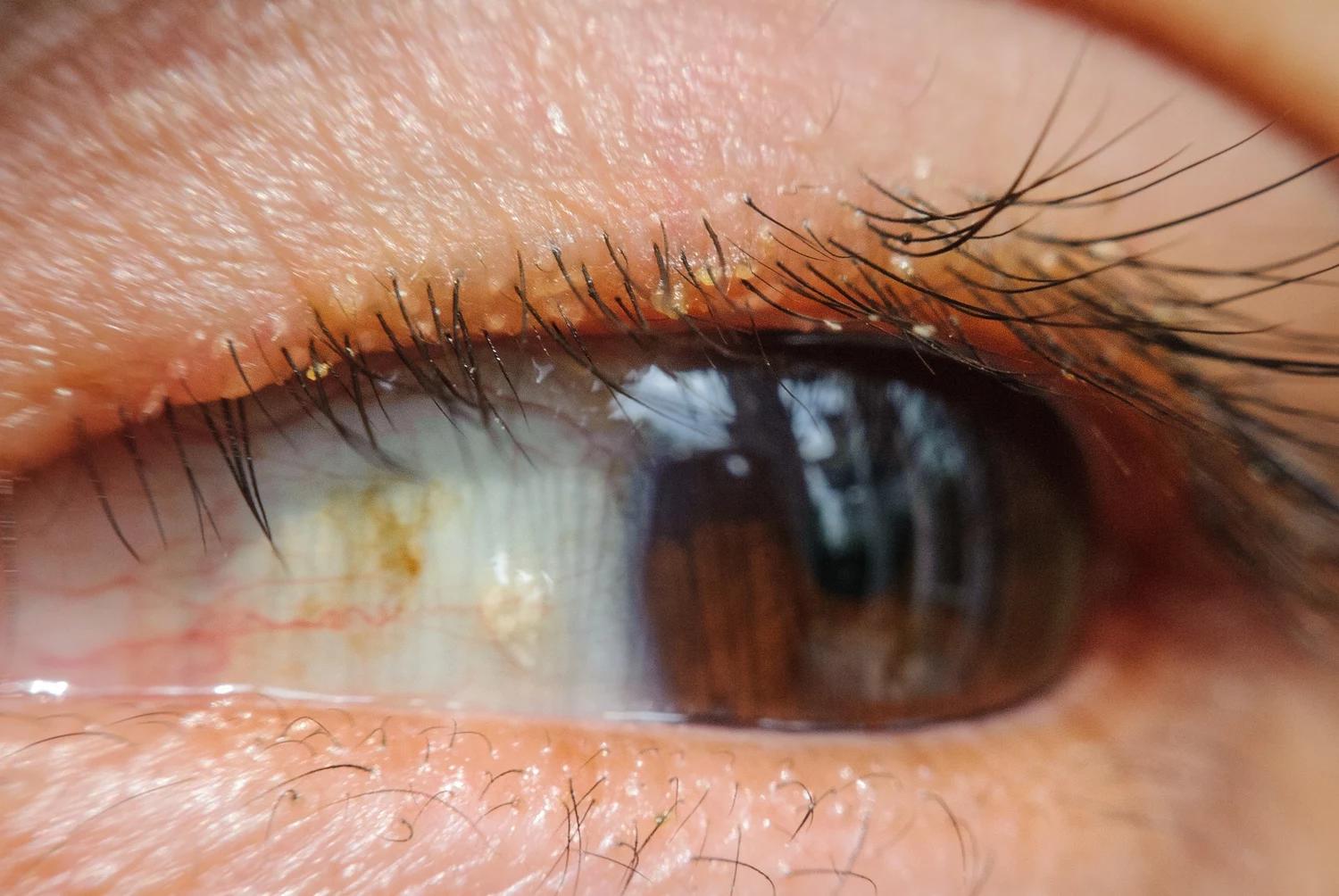
Demodex and blepharitis
This is a very common parasite in humans, with 100% of patients 70 years and over having this parasite on their bodies. One area of controversy the nature of relationship between Demodex and humans. Are mites parasitic, commensal or mutualistic? Mites can live harmlessly in the skin or become a pathogenic agent, depending on how high the population is.
A number of treatments are available to treat mites. These include Lotilaner ophthalmic solution, 0.25% (Tarsus Pharmaceuticals) applied twice daily; spinosad (APT-001, Aperta Biosciences), an unguent for blepharitis; ivermectin, a topical possibly weekly application, for Demodex.
Selenium sulfide (Azura Ophthalmics) has a positive effect on meibomian gland obstruction and was reported to improve the glands by more than 30% in contact lens wearers following treatment for 6 weeks.5 It is an unguent applied twice weekly for blepharitis, meibomian gland dysfunction and contact lens dryness.
This article was adapted from Dr. Hom’s presentation at the Southern Congress of Optometry International. Dr. Hom is a consultant to numerous drug manufacturers.
Related: Blepharitis requires patient education
References
1. https://protect-us.mimecast.com/s/0-BeC2kEoESVqgPRCnFDCB?domain=modernod.com
2. Wu PC, Chuang MN, Choi J, et al. Update in myopia and treatment strategy of atropine use in myopia control. Eye (Lond) 2019;33:3-13; doi: 10.1038/s41433-018-0139-7
3. https://reviewofmm.com/vyluma-leading-with-innovation/
4. Lee JJ, Fang PC, Yang IH, et al. Prevention of myopia progression with 0.05% atropine solution. J Ocul Pharmacol Ther 2006;22:41
5. https://azuraophthalmics.com/scientific-meetings
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.





.png&w=3840&q=75)










