Expanded surgery options address limitations of trabeculectomy
The glaucoma surgery armamentarium has increased in recent years to include several alternatives to trabeculectomy with potential safety advantages.

Key Points
Boston-The glaucoma surgery armamentarium has increased in recent years to include several alternatives to trabeculectomy with potential safety advantages. Trabeculectomy, however, remains the gold standard, as surgeons await more robust outcomes data for the newer techniques, said Kathy Williams, OD, at the annual meeting of the American Academy of Optometry.
"Trabeculectomy continues to be the preferred procedure when glaucoma patients need surgical intervention, and particularly when more aggressive IOP lowering is needed," said Dr. Williams, a private practitioner in Seattle.



Dr. Williams noted that the procedure for implantat ion of the minishunt has evolved over time. It was originally implanted under the conjunctiva, but now the device is placed under a scleral flap. This approach has been associated with a high success rate, along with a reduced chance of postoperative hypotony and device erosion compared with the earlier technique.
Canaloplasty opens Schlemm's canal to restore circumferential flow of aqueous from the canal to the collector channels. It is performed using a flexible microcatheter (iTrack 250A, iScience Interventional) that goes circumferentially around Schlemm's canal. Then, the canal is dilated using a viscoelastic agent (Healon GV, Abbott Medical Optics). Next, the surgeon passes a 10-0 polypropylene tensioning suture through the circumference of the canal to create tension on the inner wall of the canal for sustained IOP reduction.
"Although the rationale for the suture placement during canaloplasty is to stent open Schlemm's canal in order to reduce IOP, its mechanism of IOP-lowering action is still not completely understood," Dr. Williams said.
She added that there is a signif icant learning curve involved in performing successful canaloplasty in terms of identifying the entrance into Schlemm's canal during dissection of the deep scleral flap and exposure of Descemet's window.
"The technically challenging nature of the procedure has been a factor limiting its adoption despite data demonstrating its efficacy and safety," Dr. Williams noted.
Positive 3-year outcome data from a prospective, international clinical trial of canaloplasty were recently reported showing sustained IOP control with reduced patient dependence on medications, a low rate of complications, and minimal need for postoperative intervention [J Cataract Refract Surg 2011;37:682-690].
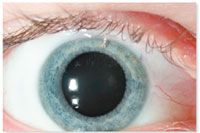
Ab interno trabeculectomy is performed using a proprietary electrocautery device to selectively ablate trabecular meshwork tissue and the inner wall of Schlemm's canal in order to restore aqueous outflow.
The ablation targets the juxtacanalicular region that is considered the site of greatest resistance to aqueous outf low in patients with primary open angle glaucoma, Dr. Williams explained.
The procedure is based on goniotomy, which historically has been the treatment of choice for pediatric patients with congenital glaucoma, and it is performed using a direct goniolens to identify the surgical site. Data from postmarketing studies show that IOP can be maintained in the 15 to 17 mm Hg range over a period of 5 to 6 years after surgery.
"Ab interno trabeculectomy has significant advantages in that it is essentially a blebless procedure without risk of bleb infection, and it also spares the conjunctiva in the event that additional surgery will be required at a later date," Dr. Williams said. In conclusion, she said, "Compared with canaloplasty, the ab interno trabeculectomy procedure has a steeper learning curve and, for that reason, it has been relatively well adopted not only by glaucoma surgeons, but also by cataract surgeons. For patients with cataract who require a moderate reduction in IOP, a combined procedure with phacoemulsification and ab interno trabeculectomy can be done through the same clear corneal temporal incision."

FYI
Kathy Williams, OD
E-mail: kyangwilliams@gmail.com
Dr. Williams has no relevant financial disclosures.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.