Experiencing retinal detachment as an OD
When the retina in my left eye detached in early October 2013, I was on a tour bus, somewhere between Canter’s Deli and Griffith Observatory, in Los Angeles. There was a series of flashes, like warning flares, and then a black tide, an oil slick of a blind spot that started down and to the left and crept toward the center of my vision, arcs of lightning heralding its advance. I knew what was happening, but I didn’t want to believe it.
“‘Tell us please, what treatment in an emergency is administered by ear?’....I met his gaze and I did not blink. ‘Words of comfort,’ I said to my father.”
--Abraham Verghese, Cutting for Stone
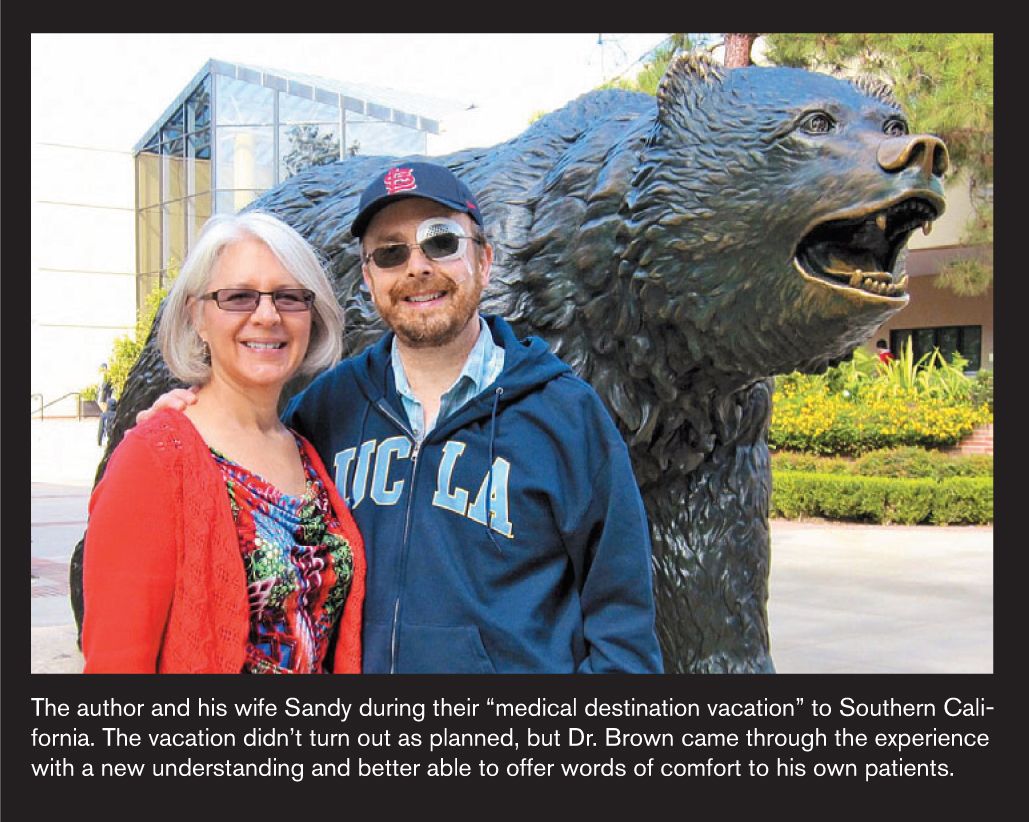
When the retina in my left eye detached in early October 2013, I was on a tour bus, somewhere between Canter’s Deli and Griffith Observatory, in Los Angeles.
Non-stop texting caues a case of retinal detachment, says Chinese media
There was a series of flashes, like warning flares, and then a black tide, an oil slick of a blind spot that started down and to the left and crept toward the center of my vision, arcs of lightning heralding its advance. I knew what was happening, but I didn’t want to believe it. My wife and I had snuck out to California from Alabama for some much needed R&R-and now this.
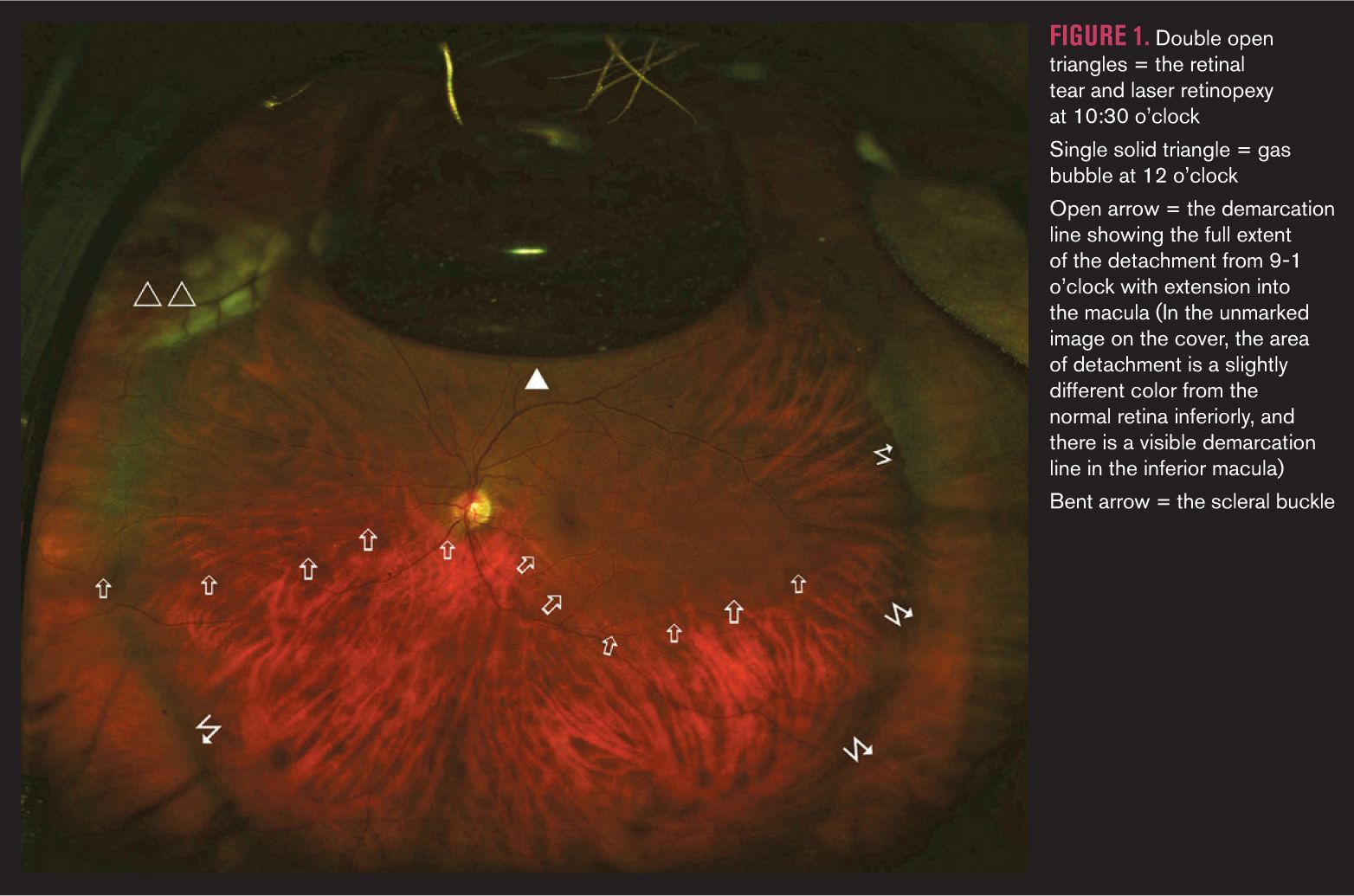
No stranger to ocular procedures
It was little wonder that I’d arrived at this point, though. After many years of diagnosing eye disease and battling vision loss in others, I had, from June 2012 until May 2013, experienced in order: a posterior vitreous detachment; retinal tear; and vitreous hemorrhage in the right eye which had been treated with laser retinopexy and vitrectomy; a myopic shift from rapid-onset nuclear sclerosis following the vitrectomy which caused several diopters of anisometropia; another retinal tear in the left eye (at 10:30 o’clock) with laser repair; an epiretinal membrane in the right eye; and finally, cataract surgery in both eyes.
That’s a lot of ICD-9s and RVUs that simply don’t do the experience justice.
From the location of my scotoma, I reasoned that the laser repair in my left eye had failed for some reason. It was late on a Friday afternoon, and I didn’t want to be that patient who rushes into the office at the end of the week with a major problem. I judged that my macula was still on, and I knew that if I had surgery within a couple of days, my prospects remained good. I tried to enjoy the rest of the tour as much as possible, and later that evening we met up with our friends in Malibu.
I decided not to totally ruin the grand reunion by telling them right away. We had dinner, and afterward, I closed my eyes in an effort to quiet the currents of liquefied vitreous that pulled on the retinal tear and held my head to down and to the right, enlisting gravity as my ally to prevent my macula from unraveling.
Eventually, they noticed. “You must really be tired,” one of them observed.
“Yes,” I replied, “but my retina is also detaching.”
Seeking treatment
We spent the rest of the evening planning for the day ahead. I knew my best bet was an academic medical center that could scramble the resources necessary for major eye surgery on a Saturday. Only one question remained: Would I go with the Bruins or the Trojans? UCLA was closer than USC, so the plan was hatched.
After going NPO after midnight, I presented to the emergency department at Ronald Reagan UCLA Medical Center at 9 a.m. the next morning. The waiting room was calm and empty. A security guard greeted us warmly and offered his assistance. He ushered us to the front desk where the triage nurse was waiting. I explained to her who I was and what was happening. She took my blood pressure (it was high), but moreover, she took me seriously.
The ER doctor had already been briefed on my situation by the time he walked into the exam room pushing the B-scan cart. He listened to my story, squirted some gel on my left eye, and placed the probe gently. He took a brief glance at the screen and then turned it toward me.
Reviewing an optic pit in a glaucoma suspect
“What do you think?” he asked.
I looked at the bulging, reflectile arc in mid-vitreous and shook my head. “It’s even worse than I thought,” I said.
I remembered what it had been like to be the neophyte doctor with a wrinkleless face who no one took seriously, so I didn’t dare ask the young resident who escorted us to the eye exam lane how old she was. Instead I asked, “What year are you?”
She knew exactly what I was getting at. “I’m a first year-but don’t worry, Dr. Brown, I’m just going to get things started. I’ve already called the retina fellow. He’s totally awesome.”
She was a little nervous, which I found both endearing and appropriate considering that I’d seen over 70,000 patients in my career and she was barely out of the gate.
Once I was dilated and behind the slit lamp, she quickly found the bullous retinal detachment that spread from 9-1 o’clock in my left eye. But she seemed just as fascinated with my right macula.
“Look’s like you’ve got…drusen,” she said.
I decided she needed a little help. “What you’re seeing is an epiretinal membrane. Try using the red-free filter; it’ll really pop out then.”
She did and was pleased. A professor’s work is never done.
The retina fellow who ambled into the room wasn’t much older than the first-year resident, but with his morning stubble and tired, puffy eyes, he appeared a bit more grizzled. He found the tear on the anterior side of the detachment near the vitreous base. A bare slit, it was only visible with the gaping that comes from scleral indentation.
He excused himself to talk with the retina chief and plan my surgery. I knew what was likely coming, and when he returned, he confirmed that they planned to do a scleral buckle, vitrectomy with gas tamponade, and laser retinopexy-the proverbial “kitchen sink.”
Throttling down while face down
“You’re not going to be able to travel for several weeks,” he said. I held my head in my hands as a vision of all the work that I “needed” to do back home flashed before me. The fellow was young and still searching for the right words of comfort to match his prodigious surgical skills, but in the long pause that followed, he reached down deep and found them.
“Dr. Brown,” he said, “you’ve spent your life taking care of others, and now it’s time to let someone else take care of you.”
What followed in the next few days was, well, a blur. For 25 years, almost half my life, I had run full throttle. But after my surgery, it was as if someone had pulled the plug. Face down in the world, with my eyes closed, I was forced to become a good listener.
I listened to good books and old music. Through the screen door of the Pepperdine University condo where I was holed up, I could hear the howls of coyotes and the click-clack of mule deer hooves echoing off the rocks of the craggy Santa Monica Mountains. Sea breezes blew in from the Pacific, cooling my skin and massaging my ears. I heard the playful banter of our hosts’ young daughters and tapped my foot to the beat of the domestic routine. At other times, the darkness and silence enveloped me like a womb.
Stem cells used to grow light-sensitive retina in lab
Our friends and my wife (when she wasn’t busy spotting some of her favorite stars at local Malibu haunts) brought me good food-and lots of wine! The chief of retina at Jules Stein Eye Institute, Dr. Stephen Schwartz, became both my doctor and my friend. He reassured me at my follow-up visits that things were going well, but he held me in a hard gaze when I admitted that I was cheating on my “face-down” time.
“We gave you a ‘smart person’-sized gas bubble for compliant patients-maybe we were wrong!” he scolded.
I obeyed, and things went well. The large gas bubble, which had filled my vitreous cavity and jiggled with every micro-movement, grew smaller each day, eventually shrinking to a single dot. One morning I woke up, and it was completely gone.
I grabbed some scissors and clipped the green warning bracelet from my wrist as if I was unlocking a shackle. I was now free to move about the country. We booked a flight home, and when it came time to call airport taxi service, we spent the extra $20 for a Lincoln Town Car and traveled down PCH toward LAX in style.
It’s been a year now. My left eye aches when the weather changes, but I count myself a fortunate man. I have some micropsia and metamorphopsia in my left eye, but it’s become less noticeable, and I’m correctable to 20/20. The induced myopia from the scleral buckle is only about 1.50 D, and much to my surprise, I’ve adapted well to the unplanned monovision. The mild vision loss I’ve suffered is nothing compared to that of many of my patients, and I’m thankful that I can still do the work I love.
Recently, one of my patients presented with a fresh retinal tear and detachment in the exact same location as mine. I explained to her what was happening and what needed to be done. I saw her eyes well with tears as reality hit home.
I leaned forward slightly, the veteran welcoming the new initiate with words of comfort, and spoke softly. “I’ve been where you are. You’re going to get through this, and you’re going to be okay.”