Faster epithelial healing for patients with corneal abrasion and PRK
Shifting the treatment paradigm can lead to less pain, inflammation
Image Credit: AdobeStock/andranik123

The recovery processes are similar for patients who present with a large corneal abrasion or undergo photorefractive keratectomy (PRK; laser ablation to remodel the corneal stroma). The wound is often very painful until the corneal epithelium has healed, which can take up to a week. Our goals are to control pain, prevent infection, and achieve epithelial healing as rapidly as possible, in turn further reducing infection risk and pain.
Recently, I have altered my treatment paradigm for these patients, after seeing an artificial tear promote faster healing.1-4 A colleague used a tear that contained trehalose as part of corneal cross-linking recovery, and we saw an amazing improvement in how quickly the patients healed. So when a new tear with trehalose became available last year, I added it to my regimen for patients with large corneal abrasions and PRK. I have seen re-epithelialization time improve by several days—from an average of 5 days to just 3. When the epithelium heals more quickly, the inflammatory process moderates, the patient’s pain diminishes sooner, and the epithelium can begin the process of becoming smoother and more regular—a significant change for patients going through this painful healing process.
Battling inflammation, pain, and potential infection
The treatment regimen for these patients has a lot of variability, depending on the individual surgeon. Like most surgeons, I apply a bandage contact lens over the cornea to promote comfort and healing. I prescribe an antibiotic until the wound has healed, at which point I remove the contact lens. My patients also get a topical steroid to control inflammation and reduce haze. I taper the steroid slowly over 4 to 6 weeks, depending on how the surface is doing after the epithelium heals.
To manage the pain, I give patients a diluted proparacaine drop, which I ask them to bring back after the first week to ensure they don’t accidentally use it after the epithelium has healed. I also prescribe oral gabapentin to reduce nerve pain as needed.
If we can get the abrasion to heal faster, we can reduce pain, improve patients’ experience, and prescribe less medication for pain control. This is especially important because the pain can be severe—in some cases, so acute that doctors may prescribe narcotics. This pain makes some patients wary about getting PRK, and it makes some doctors wary of performing it. In my experience, the pain gets worse on the second or third day, so if the epithelium can heal in a few days, we can significantly change the recovery process.
Healing the epithelium in days
In the past, I gave patients with large corneal abrasion and PRK artificial tears to use as needed, but I never focused on tears having a significant role in therapy. That changed when I saw my colleague’s results.
I started giving patients the new high-quality, preservative-free, brand-name artificial tear (iVizia; Thea Pharma) in mid-2022. Using a preservative-free tear is essential for these patients, who need frequent dosing and already have an inflamed ocular surface.
Since I started having my patients use iVizia 4 times per day, I have seen significant improvement in healing time. Instead of the average patient achieving full closure in 5 days, I am seeing full closure around day 2 or 3, and the epithelium is starting to smooth out by day 5. Faster wound healing is reducing patients’ pain, lessening their need for anesthetic and pain medications, and decreasing their chances of developing haze. Recently, I have begun telling some patients to use iVizia as frequently as every 2 to 3 hours to maintain consistent comfort, and it is safe to do so because the drop is preservative free.
Case study: Large corneal abrasion after corneal transplant
Figure 1. Large Corneal Abrasion. Patient aged 67 years with a previous corneal transplant exhibiting a large corneal abrasion. (Image courtesy of Leela V. Raju, MD)
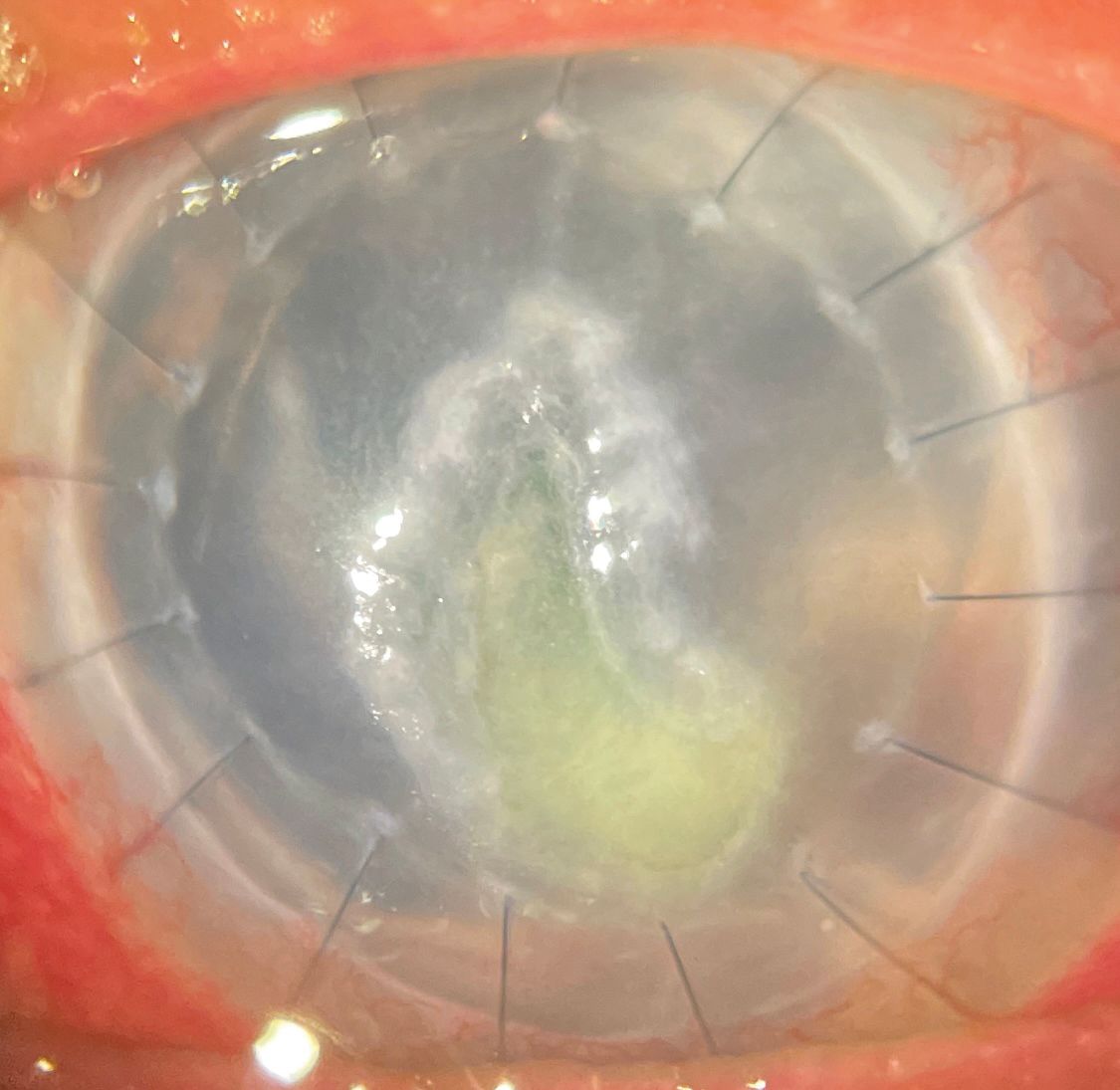
A 67-year-old woman with a previous corneal transplant complained that she had been experiencing tearing and redness for the last 5 days. She did not have a lot of pain. On examination, I found she had a large corneal abrasion (Figure 1). This would normally cause severe pain, which suggested there was a component of neurotrophic keratopathy. After placement of a bandage contact lens, I prescribed an antibiotic eye drop and iVizia.
Figure 2. Abrasion With Treatment. Significant improvement with no evidence of thinning after using an antibiotic and iVizia for 4 days. (Image courtesy of Leela V. Raju, MD)
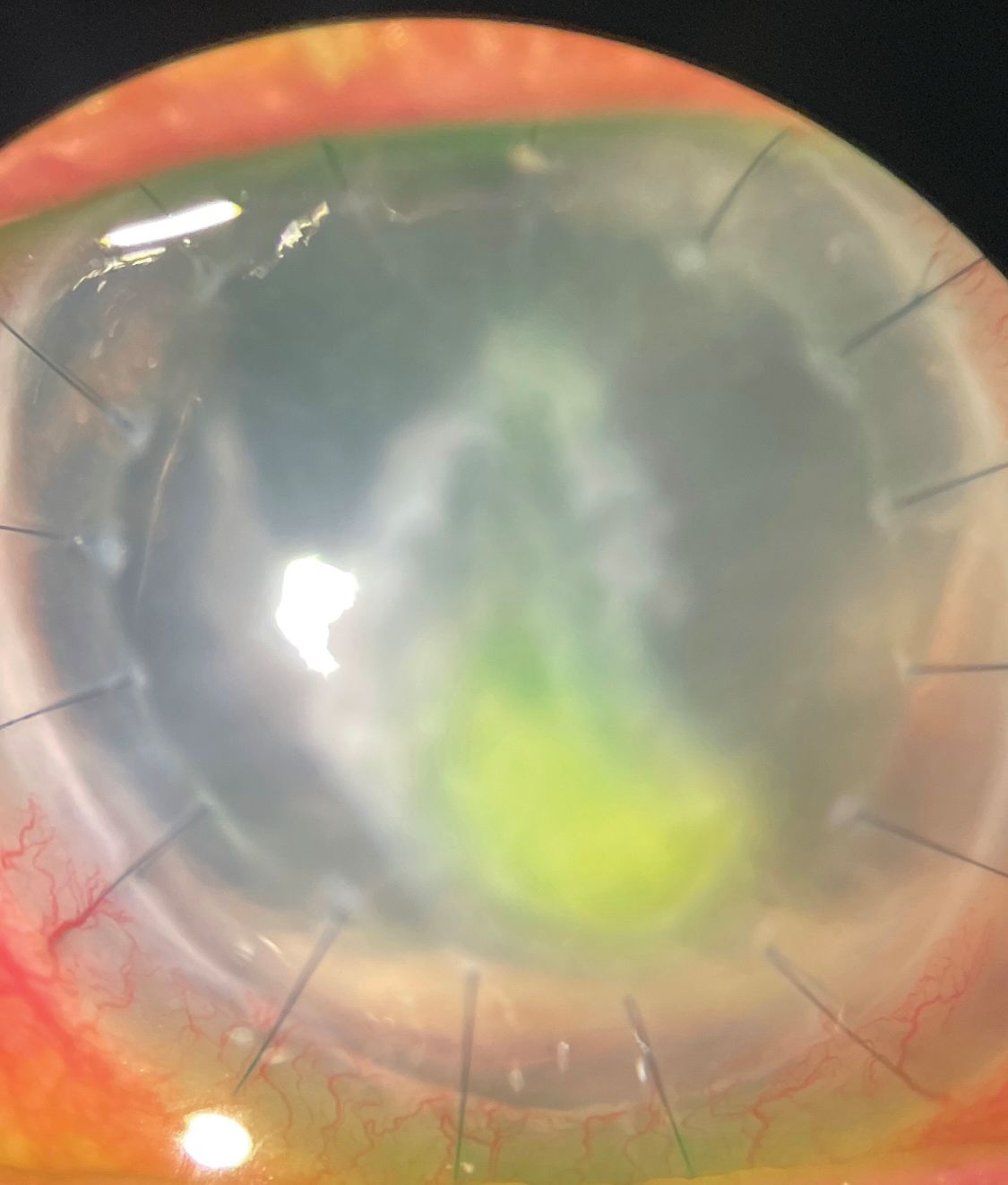
When the patient returned for a follow-up visit 4 days later, the abrasion showed significant improvement without any evidence of thinning (Figure 2). The patient is continuing to wear the bandage contact lens and use the antibiotic and iVizia until the abrasion fully heals.
Faster healing changes everything

Now that I have seen the results of using this tear to promote epithelial healing, I continue to use these drops and recommend them to others. In addition to patients with PRK or corneal abrasions, I am now using these tears for my patients who have had laser-assisted in situ keratomileusis and those who undergo corneal cross-linking. In the future, I would be excited to see clinical studies of the effects of artificial tears with trehalose on epithelial healing from corneal abrasions.
References:
Matsuo T. Trehalose protects corneal epithelial cells from death by drying. Br J Ophthalmol. 2001;85(5):610-612. doi:10.1136/bjo.85.5.610
Chen W, Zhang X, Liu M, et al. Trehalose protects against ocular surface disorders in experimental murine dry eye through suppression of apoptosis. Exp Eye Res. 2009;89(3):311-318. doi:10.1016/j.exer.2009.03.015
Hovakimyan M, Ramoth T, Löbler M, et al. Evaluation of protective effects of trehalose on desiccation of epithelial cells in three dimensional reconstructed human corneal epithelium. Curr Eye Res. 2012;37(11):982-989. doi:10.3109/02713683.2012.700754
Li J, Roubeix C, Wang Y, et al. Therapeutic efficacy of trehalose eye drops for treatment of murine dry eye induced by an intelligently controlled environmental system. Mol Vis. 2012;18:317-329.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.