How techs should handle ocular emergencies
When a patient experiencing an ocular emergency walks through the door, it is vital that every member of the team knows what to do in order to save the patient’s sight-and in some cases, his life. (Editor's note: This article contains some graphic images of ocular trauma that may be disturbing to some readers.)
When a patient experiencing an ocular emergency walks through the door, it is vital that every member of the team knows what to do in order to save the patient’s sight-and in some cases, his life.
“The wrong time to train your staff on an emergency is during the emergency,” says Lynn Lawrence, CPOT, ABOC, COA. “They must be trained prior to the emergency walking in the door for the best outcome.”
Lawrence is an ophthalmic technician in Pensacola, FL, but he served for 30 years in the U.S. Air Force, during which time he was appointed ophthalmic career field manager, overseeing 540 optometric and ophthalmic technicians at 90 locations around the world. Throughout his career, Lawrence has treated countless ocular emergencies, and he now teaches other techs how to recognize and address these high-stakes cases.

Defining an ocular emergency
According to the U.S. Department of Labor, there are an estimated 1,000 eye injuries occurring every day in workplaces in the United States.1 While patients often think of their current problem or condition-regardless of what it is-as an emergency, a true ocular emergency is a condition that can cause sudden loss of or decrease in vision that could lead to a permanent condition.
As soon as possible, your team needs to be able to assess the situation before taking action. Techs should be able to classify ocular presentations based on their need for medical attention:
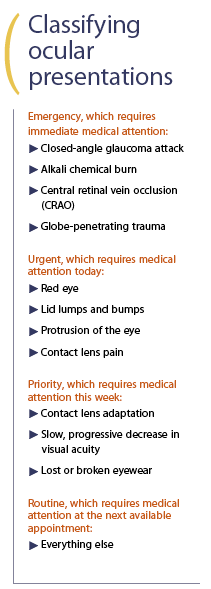
*Correction: Central retinal vein occlusion (CRVO)
While some emergencies will be obvious upon presentation, a number of signs and symptoms could signify a true ocular emergency:
• Sudden increase in ocular pain
• Sudden blurred or loss of vision
• Bleeding in or around the eye
• Trauma
• Flashes or floaters
Other symptoms of an urgent condition are:
• Photophobia
• Pain
• Foreign body: organic or non-organic
• Redness
• Abrasions
Next: Have a plan for emergencies
Have a plan for emergencies
Now that you know you have an emergency on your hands, you better have a plan for what to do next.
What will you do if an emergency case presents, but the doctor isn’t there? What will you do if a patient who suffered significant ocular trauma comes in? How would you handle a patient who calls and describes symptoms of an ocular emergency?
In order to handle an emergency situation, your practice must have a plan before that patient ever walks through the door.
“Staff training. Staff training. Staff training-I cannot emphasize that enough,” says Lawrence. “Training has to start long before the staff ever encounters an emergency.”
Every practice should have a unique emergency plan. Emergency protocols should vary on the practice’s vicinity to the next level of care, whether that means an ophthalmology practice, emergency room, trauma center, or oculoplastic surgeon.
“If a practice has four locations, for example, the practice that’s 50 miles from the next level of care should have a very different plan from the practice that’s five miles away from the next level of care. Each location needs its own training regimen on how to handle a particular emergency,” Lawrence says.
A team at a rural practice will likely require more training and a more extensive plan than a practice in a suburban or urban setting, where a patient would have better access to emergency care.
Lawrence says that regardless of your practice’s location, have a list of emergency contacts ready so everyone knows whom to contact when an urgent case walks through the door (see page X for Lawrence’s emergency phone protocol).
Once the situation is handled, go back as a team and assess the performance. What did you do right? What did you do wrong? What will you do next time? Use the case as a way to prepare for the future.
Next: Putting the plan into practice
Putting the plan into practice
If the most dangerous case you’ve encountered as a tech was a mean case of glaucoma, then it would be understandable if the idea of a trauma case coming through the door causes you to panic. But don’t worry-your whole team has a plan, you’ve practiced, and you know what to do.
And step one? Remain calm, and do your best to keep the patient calm. (Note: Lawrence says that in general, techs at optometry practices shouldn’t even invite the patient back into the exam area if they are bleeding. It is usually more important that the patient get to an emergency room so a doctor can stop the bleeding.)
More tips for handling trauma:
• Make sure the patient sits or lies down immediately. While trauma cases can vary widely, it’ll only get worse if the patient falls.
• Never leave the patient. If you have to make a call, bring the phone to the patient’s location. You need to be there with him in case the situation escalates.
• If the doctor is available, inform her immediately.
• Know whom you need to call. Have your phone list ready at various spots in your practice with all the emergency phone numbers.
• If possible, attempt to assess visual acuity and intraocular pressure.
Like any emergency situation, the person with the most experience should take the lead and communicate instructions to the rest of the team.
Next: Looking at real-life cases
Looking at real-life cases
When he lectures around the country on this topic, Lawrence shares a variety of real-life cases he’s encountered during his career. While Lawrence’s lectures certainly aren’t for the faint of heart or those who are easily bothered by the sight of blood, these cases are just a snapshot of what walks into eyecare practices around the country every day.
Quick action saves stroke victim
A patient presents with a sudden decrease in vision. During the triage process, Lawrence and his team identified that the patient was experiencing a stroke.
“It wasn’t just a threat to the patient’s eye health, it was a threat to his overall health,” he says.
After explaining his concerns to the doctor, the doctor agreed, and the staff called 911 for an ambulance to transfer the patient to the emergency room.
“The outcome was positive because of the fast response of the staff,” says Lawrence. “People come in thinking, ‘The problem is my eye because my vision is going bad,’ but the thing about the eye is it’s one of the smallest organs in your body-but inside that organ, you have the smallest blood vessels, the smallest nerves, the smallest muscles, so disease and other emergencies will manifest in the eye.”
Blurry vision hints at new mother’s life in danger
Two weeks after giving birth, a woman wakes up with blurry vision that gets worse throughout the day. Around 11 a.m., her husband contacts the practice and is instructed to bring her in immediately.
“We dilate and look in the back of her eye, and all of the blood vessels in the back of her eye are rupturing,” Lawrence says. “We’re seeing all this bleeding going on in the back of her eye, but what was really going on was she had complications from her pregnancy.”
The woman’s blood pressure shot up to over 200/90. The staff acted immediately, and the woman had to spend two weeks in the hospital to treat her blood pressure.
“We had to turn her over to a higher level of care, of course, because of the significant level of bleeding in the back of her eye, but we believe that because of the way we acted, we saved her life-not just her eye,” says Lawrence.
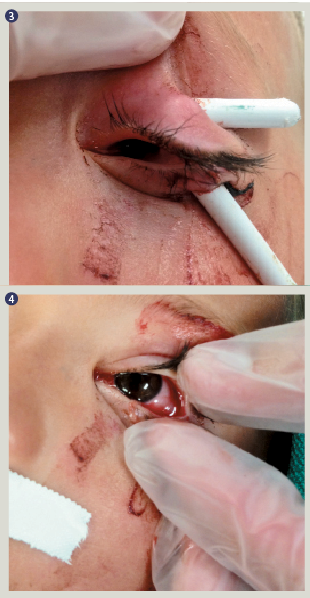
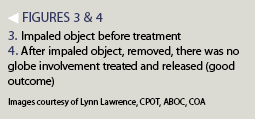
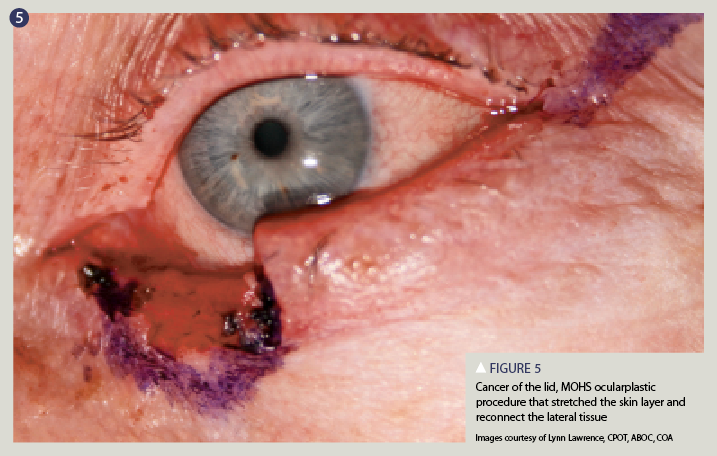
Man’s eyelid gets hooked
A man who worked for a moving company was moving furniture when a hook at the top of a screen door became attached onto the man’s eyelid.
“It looks pretty bad when he walks in the door, and that’s why it’s important to know what level of care he’s going to need next,” says Lawrence. “Not everyone is going to be able to sew that up-if it’s available, you’re going to want to get that patient to an oculoplastic surgeon as soon as possible.”
Reference
1. U.S. Department of Labor. Program Highlights: Fact Sheet No. OSHA 92-03. Eye Protection in the Workplace. Available at: https://ehs.okstate.edu/training/oshaeye.htm. Accessed 11/19/2015.