MGD redux
Meibomian gland dysfunction never went away, but current interest by researchers has put MGD on the front burner.
It has a been a little more than 2 years since the Tear Film & Ocular Surface Society (TFOS) released its report on the International Workshop on Meibomian Gland Dysfunction (MGD). This comprehensive report, written by leading experts around the world on dry eye, summarizes the knowledge at that time regarding MGD-definition, classification, anatomy, physiology, pathophysiology; tear film lipids, epidemiology, risk factors, diagnosis; management, treatment, and clinical trials.

Dr. KwanIf anything, the field of MGD is just now picking up steam, as evidenced by the sheer number of MGD specific peer-reviewed publications since March 2011 (99), and more than 40 posters presented at this year’s ARVO meeting. The fact remains that better understanding MGD for the benefit of our patients will take worldwide teamwork.
It is crucial to let our patients know that 86% of all dry eye demonstrates signs of MGD.1 Doing so isn’t always as simple as breaking down a patient’s dry eye to an exclusive oil problem or water problem because the two groups overlap. As clinicians, it’s also vital to put aside poor diagnostic tests and focus on tests that are more sensitive, specific, and correlate well to symptoms. For example, Rahman et al2 found that the sensitivity of fluorescein break-up time to be quite low, 21.42%. A battery of tests may be better suited for an initial work-up, whereas other tests may be better suited for follow-up visits. For example, meibomian gland atrophy and Schirmer are not expected to change over time, even with treatment, but are critical to gauging which dry eye sub-type is likely contributing most to symptoms.

Figure 1. Corneal staining with diffuse and partially coalesced punctate epithelial erosions.Symptom-specific testing
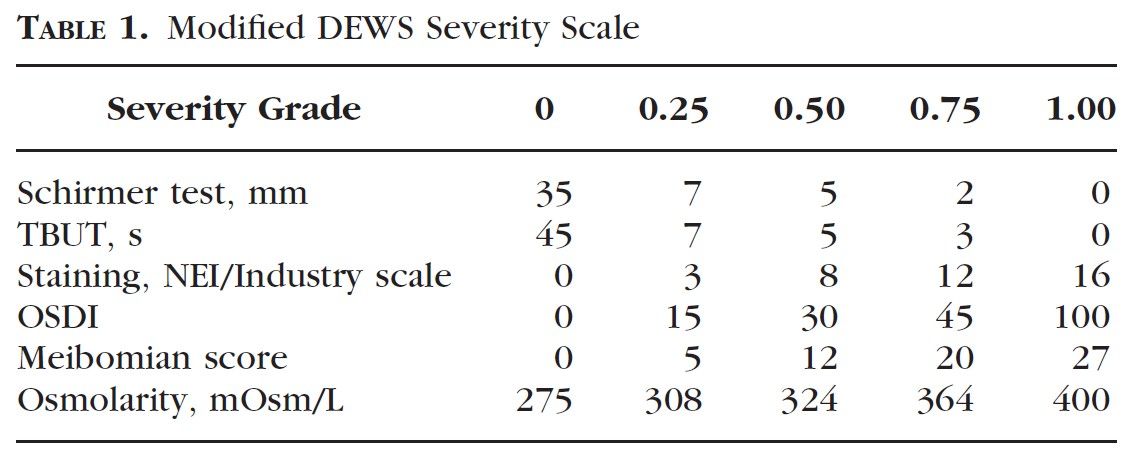
Staging severity (see Table 1) is best done from the multicenter work of Sullivan et al,3 in which precise, consistent, and solid methodology proceeded from least invasive to most invasive testing. Specific concentrations and volumes of liquid fluorescein and lissamine green were also used along with a designated wait time post instillation before evaluation. Sullivan et al4 also found little correlation between standard dry eye tests. However, meibomian gland function, corneal staining, and conjunctival staining correlated mildly to symptoms per OSDI: 0.17, 0.15, and 0.14 r2 values, respectively. Evaluating the lid wiper is critical because this may be the only sign that raises a red flag in symptomatic individuals with otherwise normal tear break-up time (TBUT), normal Schirmer, and no fluorescein staining. In fact, Korb5 found that lid wiper epitheliopathy was present in 76% of patients with symptoms, 6 times more frequently than asymptomatic patients. Pult et al6 found that checking for lid parallel conjunctival folds (LIPCOF) is also a more sensitive and more specific test than non-invasive break-up time (NIBUT) and approached the utility of OSDI.
According to TearScience, the degree of meibomian gland atrophy affects whether a patient may or may not benefit from the company’s Lipiflow treatment. It makes sense that the success of melting and expressing the meibum depends on how many meibomian glands remain. Repairing the physiology is effective only if there is sufficient anatomy to start with. With commercially available instruments easily able to image meibomian gland structure, clinicians can better triage or adjust the aggressiveness and timing of first-line treatments vs. advanced treatments. This is a significant opportunity for optometrists to refer to other optometrists and ophthalmologists with the Keratograph 5M (Oculus Inc.) or the Lipiview interferometer (TearScience). Similar to glaucoma management, if a practice is unable to invest in an OCT of its own but wants to manage the patient, then the practice would refer out to obtain the scan. Also, if a younger patient has moderate atrophy, then more aggressive treatment would be warranted to minimize dryness and further atrophy over the next few decades.
As with most healthcare models, a shift has taken place toward preventative medicine so conditions can be addressed early on to save downstream costs and co-morbidities. A few groups have recently re-examined the link between hypercholesterolemia and MGD since the Beaver Dam Eye Study found no association. Pinna et al,7 and Bukhari,8 among others, all report that HDL, LDL, and triglyceride levels are elevated in MGD and correlate to MGD severity. With the Affordable Care Act upon us, it makes a lot of sense for primary-care providers and optometrists to synergistically deliver care in this area. Patients with hypercholesterolemia tend to be in an age group where dry eye increases in prevalence. Just as a dilated eye exam is a standard of care in the management of patients with diabetes, perhaps a baseline MGD evaluation should also be part of hypercholesterolemia.
High-dose omega 3 regimen
For quite some time, omega 3 fatty acids have been known to decrease inflammation, but still unknown is at what dosage. Their clinical applications range from treating hypercholesterolemia to depression. Doses in the literature start at 0.5 grams per day and, at times, exceed 6 grams per day. To our patients’ benefit, a daily dose of 1000 mg total of EPA and DHA or greater can easily be achieved from online retailers for less than $10 per month. This is three times the amount typically available per softgel in standard over-the-counter preparations. For patients unable to intake a large softgel, fruit-flavored liquid fish oil at high levels of EPA and DHA is also available. Labbe et al9 found that among 1,957 northern Chinese, the Zung self-rating depression scale was significantly correlated to dry eye symptoms. Perhaps both conditions can simply be treated with high dose omega 3 fatty acids. An important reminder is to tell our patients that the body’s enzymes convert flaxseed oil, a rich source of alpha-linolenic acid, to the anti-inflammatory eicosapentanoic (EPA) and docosahexanoic (DHA) acids. However, because the body’s conversion process is so inefficient, patients would get more benefit from taking EPA and DHA directly and in high doses.

Figure 2. Moderate to severe eyelid inflammation evidenced by dilated vessels.The use of topical and oral azithromycin has been shown to provide relief and can be pulsed during periods of high symptoms. Nichols et al10 reported on its benefits for decreasing contact lens discomfort, compared with QID dosing of hypromellose and glycerin rewetting drops. Igami et al11 devised a novel, off-label use of oral azithromycin in the form of three Tri-Paks, which decreased eyelid debris, telangiectasia, redness, ocular mucus, TBUT, and, most importantly, symptoms. Care must be taken with patients with macrolide allergies and those on warfarin (Coumadin), even though the risk for gastrointestinal bleeding and increased international normalized ratio has largely been disproved.12 Liu et al13 were able to show that azithromycin stimulates accrual of lipid-containing vesicles; the effect appears to maximize at days 5 to 7 in an animal model. This mechanism should drive an increased volume-and perhaps a better quality-meibum secretion, leading to a more stable tear film.
Diquafosol is a P2Y2 purinergic receptor agonist found in the palpebral and bulbar conjunctival epithelium, goblet cells, and adipocytes and ductal epithelial cells in the meibomian gland. Its believed mechanism of action is to promote mucin secretion. Arita14 reported that topical diquafosol improved tear film and ocular surface parameters as well as meibomian gland anatomy and physiology in 10 patients after 4 months of therapy. Takamura et al also15 found that diquafosol and hyaluronate ophthalmic solution (a natural lubricant) performed similarly and benefited both groups of subjects. Diquafosol was found to be superior to sodium hyaluronate in decreasing rose bengal conjunctival staining and sodium fluorescein corneal staining.
Eyelash, eyelid maintenance
Korb and Blackie16 found it highly therapeutic to debride the eyelid margin of built-up skin cells that have covered the meibomian gland orifices. Using a blunt golf spud or similar instrument, have the patient look in the opposite direction and systematically work your way across the lower eyelid margin. The uppers are a bit more challenging ergonomically but are doable. This procedure is simple, easy, and does not require anesthetic. Patients experience a mild tickling sensation. After 1 month, symptom scores improved per the standard patient evaluation of eye dryness (SPEED) questionnaire, and more meibomian glands yielding liquid secretion (MGYLS) compared with pre-treatment. Patients with obstructive or chronic MGD who have not responded well to lipid-based tears and warm compresses may benefit from this new treatment.
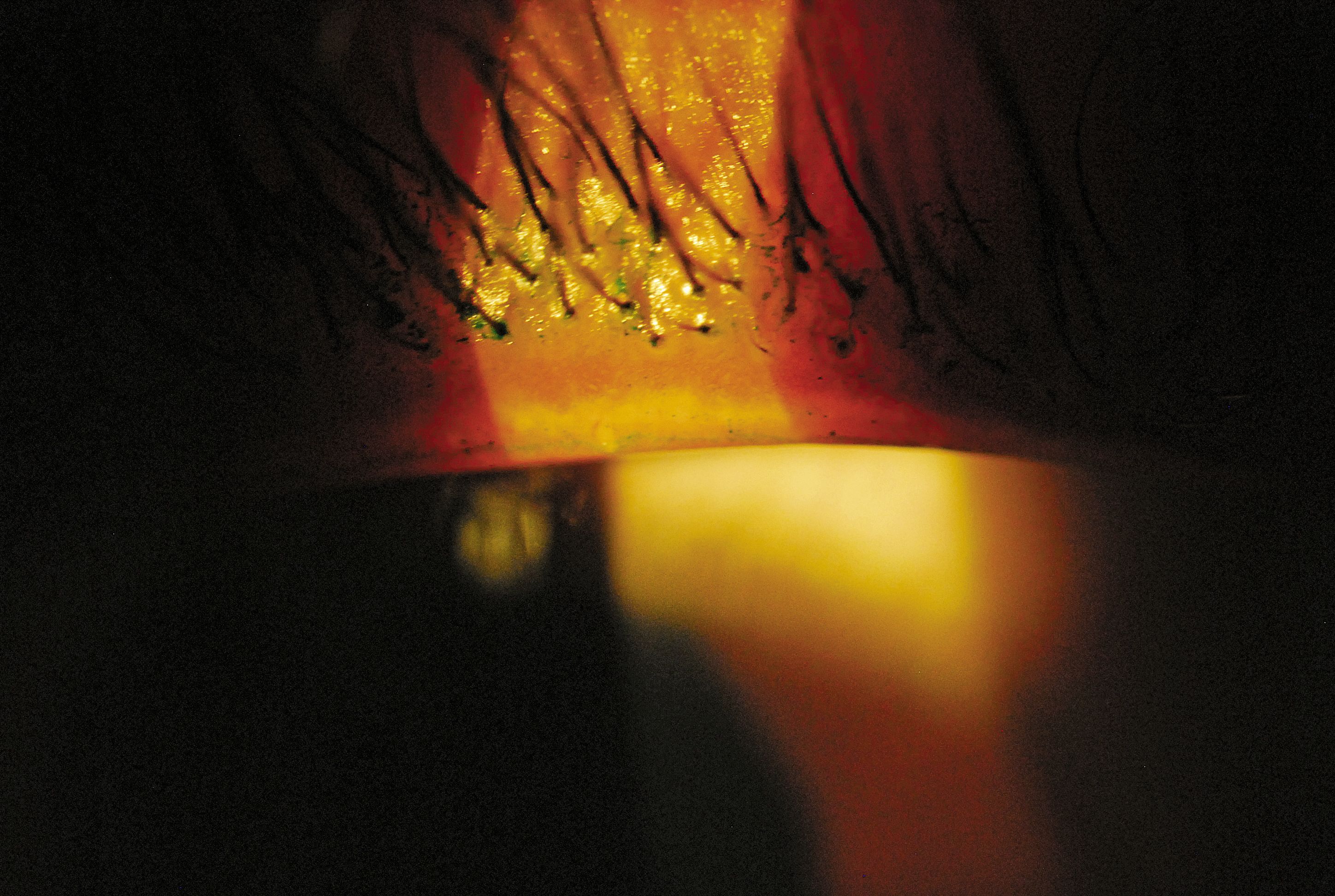
Figure 3. Upper eyelid margin staining of the Line of Marx with a single inspissated meibomian gland. (Images courtesy Justin Kwan, OD)The presence of Demodex mites within our eyelash follicles cannot be overlooked, especially in elderly persons. The mites’ activity likely exacerbates dryness, foreign body sensation, and itchiness. Be sure to ask your patient which itches more-the eye or the eyelid. Upon slit lamp examination, look for cylindrical cuffs at the base of the eyelashes. Tea tree oil is currently the only available treatment other than eyelid scrubs, which may be minimally effective because the mites are buried deeper as opposed to superficial. Koo et al17 found tea tree oil to be effective in reducing Demodex count (p=0.004). Cliradex (BioTissue) and Sterilid (Advanced Vision Research) are commercially available formulations of tea tree oil along with other ingredients, but a higher concentration for in-office treatment may be prudent to more rapidly reduce the infestation.
What can’t be overemphasized is the importance of lipid-based artificial tears. Our current options include Systane Balance (Alcon), FreshKote (FOCUS Laboratories), Refresh Optive Advanced (Allergan), and Retaine (Ocusoft Inc.). The latter two products are available in preservative-free formulations. Patients must understand that, if tears haven’t worked in the past, these specific products may work now if, in fact, there is a diagnosis of MGD. Connor et al18 found that lipid-based artificial tears in a cohort of MGD patients extended the non-invasive TBUT, while the control did not.
Numerous resources are available online, such as the extensive reports of the dry eye (2007) and MGD workshops (2011). What I also find enlightening is to periodically visit dry eye forums to see what patients are talking about. The individuals who actively participate in these forums tend to be our moderate to severe-and consequently-most desperate patients. The hope is that patients have a place to learn, vent, and find a doctor who is knowledgeable and willing to diagnose and treat to the highest level.
A London-based research firm and consulting group, GlobalData, projects that the dry eye therapeutic market will grow by $4 billion in the next 10 years.19 Now is the time to take the latest and greatest treatments to strategize a plan that will deliver relief and return quality of life to our patients. Stay on the lookout for drugs nearing approval such as lifitegrast and rebamipide.
Start moving beyond warm compresses, artificial tears, and steroids. Dry eye will continue to be one of the most dynamic fields in optometry.ODT
References
1. Lemp MA, Crews LA, Bron AJ, Foulks GN, Sullivan BD. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: A retrospective study. Cornea. 2012;31(5):472-478.
2. Rahman A, Yahya K, Ahmed T, Sharif-ul-Hasan K. Validity of symptoms as screening tool for dry Eeye. Pak J Ophthalmol. 2007;23 (4):198-203.
3. Sullivan BD, Whitmer D, Nichols KK, Tomlinson A, et al. An objective approach to dry eye disease severity. Invest Ophthalmol Vis Sci. 2010;51(12):6125-6130.
4. Sullivan BD, Crews LA, Messmer EM, Foulks GN, et al.. Correlations between commonly used objective signs and symptoms for the diagnosis of dry eye disease: Clinical implications. Acta Ophthalmol. 2012 Dec 28. [Epub ahead of print.]
5. Korb DR, Herman JP, Greiner JV, Scaffidi, RC, et al. Lid wiper epitheliopathy and dry eye symptoms. Eye Contact Lens. 2005; 31(1):2-8
6. Pult H, Purslow C, Murphy PJ. The relationship between clinical signs and dry eye symptoms. Eye (Lond). 2011; 25(4):502-510.
7. Pinna A, Blasetti F, Zinellu A, Carru C, Solinas G. Meibomian Gland Dysfunction and Hypercholesterolemia. Ophthalmology. 2013 Jun 6. pii: S0161-6420(13)00411-9
8. Bukhari AA. Associations between the grade of meibomian gland dysfunction and dyslipidemia. Ophthal Plast Reconstr Surg. 2013 Mar-Apr;29(2):101-103.
9. Labbe A, Wang YX, Baudouin C, Jonas JB, Xu L. Association between depression and dry eye disease in an adult population. Poster presented at the Association for Research in Vision and Ophthalmology, May 5-9, 2013, Seattle, WA.
10. Nichols JJ, Bickle KM, Zink RC, Schiewe MD, Hague RM, Nichols KK. Safety and efficacy of topical azithromycin ophthalmic solution 1.0% in the treatment of contact lens-related dry eye. Eye Contact Lens. 2012 Mar;38(2):73-79.
11. Igami TZ, Holzchuh R, Osaki TH, Santo RM, Kara-Jose N, Hida RY. Oral azithromycin for treatment of posterior blepharitis. Cornea. 2011; 30(10):1145-1149
12. Shrader SP, Fermo JD, Dzikowski AL. Azithromycin and warfarin interaction. Pharmacotherapy. 2004 Jul;24(7):945-949.
13. Liu Y, Kam WR, Ding J, Sullivan DA. Impact of azithromycin on lipid accumulation in immortalized human meibomian gland epithelial cells. Poster presented at the Association for Research in Vision and Ophthalmology, May 5-9, 2013, Seattle, WA.
14. Arita R, Suehiro J, Haraguchi T, Maeda S, Maeda K, Tokoro H, Amano S. Topical diquafosol for patients with obstructive meibomian gland dysfunction. Br J Ophthalmol. 2013; 97(6):725-729.
15. Takamura E, Tsubota K, Watanabe H, Ohashi Y. A randomised, double-masked comparison study of diquafosol versus sodium hyaluronate ophthalmic solutions in dry eye patients. Br J Ophthalmol. 2012 96(10):1310-1315.
16. Blackie C, Korb D. Debridement of the lower lid margin and line of marx is effective in increasing meibomian gland function and patient comfort. Poster presented at the Association for Research in Vision and Ophthalmology, May 5-9, 2013, Seattle, WA.
17. Koo H, Kim TH, Kim KW, Wee SW, Chun YS, Kim JC. Ocular surface discomfort and Demodex: effect of tea tree oil eyelid scrub in Demodex blepharitis. J Korean Med Sci. 2012;27(12):1574-1579.
18. Connor CG, Ottenbreit RA, Schroeder LK, Rabin JC, Narayana S. Comparison of three commercially available tear substitutes designed for evaporative dry eye treatment. Poster presented at the Association for Research in Vision and Ophthalmology, May 5-9, 2013, Seattle, WA.
19. GlobalData. Dry Eye Syndrome Treatment Market to Grow by Nearly $4 Billion in the Next Decade. 12 Jun 2013. http://healthcare.globaldata.com/media-center/press-releases/pharmaceuticals/dry-eye-syndrome-treatment-market-to-grow-by-nearly-4-billion-in-the-next-decade. Accessed August 26, 2013.
Author Info
Justin Kwan, OD, graduated from University of California, Berkeley School of Optometry in 2009. Dr. Kwan went on to complete a dry eye and contact lens research fellowship at Southern California College of Optometry (SCCO) at Marshall B. Ketchum University. He currently teaches full time at SCCO, oversees the dry eye clinic, and also teaches in the contact lens clinic. His areas of interest include irregular corneas, refractive surgery, orthokeratology, , and dry eye. E-mail Dr. Kwan at jkwan@scco.edu.
Take-Home Message
Interest in meibomian gland dysfunction (MGD) is high, judging by the volume of lectures delivered, articles published, and posters presented on the subject. Reinforcing the interest: A research and consulting group projects that the dry eye therapeutic market will grow by $4 billion in the next 10 years.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.





.png&w=3840&q=75)