10 tips to enhance scleral contact lens success
Improve your scleral fitting skills and your patients’ quality of life



Scleral contact lenses can be a positive, life-changing experience for our patients.
For example, envision a young man with keratoconus who would like to pursue a career but is unable to see in order to study, or a middle-aged female with Sjogren’s syndrome who is unable to drive or work due to the severity of her ocular discomfort.
Scleral lenses have demonstrated a significant improvement in quality of life for patients who had failed or are intolerant to conventional rigid gas permeable (GP) contact lenses.1
Related: Addressing scleral lens clinical concerns
Successful practitioners have embraced the intricacies of scleral lens fitting. Let’s focus on 10 clinical pearls to enhance scleral lens success.
1. Master handling
In order to succeed with scleral lenses, successful scleral lens handling is imperative. Verify that each patient understands that scleral lenses differ from soft or standard GP lenses and require specific care products and techniques.
Scleral lens dropout rates can be high, ranging from 25 percent to 49 percent.2-4 Handling is the most common reason for scleral lens dropout.
For each patient, it is critical to review specific care, cleaning, and handling procedures. Using detailed written, verbal, and demonstrated care and cleaning procedures will lead to short- and long-term success with scleral lenses. Staff members are key to teaching patients how to apply, remove, and care for scleral lenses. Even with an ideal fit, improper care can negate the entire scleral lens process.
Related: Using toricity with scleral lenses
Some patients may have difficultly seeing or handling the lens for application, including patients with high refractive error, rheumatoid arthritis, tremors and dexterity hand challenges, or missing digits. In these cases or for those who need extra help, additional tools may be used to successfully handle scleral lenses.
Several tools have helped many of my patients. One is See Green Lens Inserter by Dalsey Adaptives, which is available with and without a stand (Figure 1). The lighted plunger helps center the device for application. The stand holds the plunger and lens in place prior to application, which is helpful for patients who have unsteady hands or for those who need both hands to hold their eyelids open.
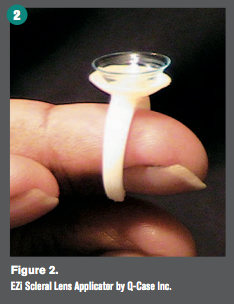
Another tool is EZi Scleral Lens Applicator by Q-Case Inc. (Figure 2). This device is placed on the finger like a ring and features a base for scleral lens application. This design provides stability and allows patients to apply scleral devices with one finger.
A third option is a #8 O-ring that is available at any hardware store (Figure 3). O-ring dimensions are 3/8” x 9/16” x 3/32”. The scleral lens rests on the O-ring on a patient’s finger, which can allow for stable application.
An additional option for scleral lens application is a sterile orthodonic ring placed on a patient’s hand. These come in packages of 100 and may be used for single-use insertion of scleral lenses.
2. Educate prior to dispensing
The Scleral Lens Education Society (SLS) video “Scleral Contact Lens Insertion, Removal, Troubleshooting, and Lens Care” (http://www.sclerallens.org/how-use-scleral-lenses) is a useful resource for both practitioners and patients alike.5
In my practice, patients watch this video prior to their scleral lens dispense and training appointments. Not only does the video help to put my patients at ease, it reduces the amount of time my staff spends with each patient.
The Gas Permeable Lens Institute (GPLI) is another organization to provide practitioners with tools for success. Both the SLS and GPLI provide useful tools such as calculators, peer-reviewed literature, frequently asked questions (FAQs), free webinars, along with the option to “Ask an Expert.”
3. Improve wettability
Surface wettability on scleral lenses can be frustrating for both the patient and practitioner. Poor wettability has the potential to decrease vision, diminish lens comfort, increase chair time, and increase costs for both the patient and practitioner.
Patients at high risk for surface wettability challenges include those with ocular surface disease, including ocular rosacea and meibomian gland dysfunction.
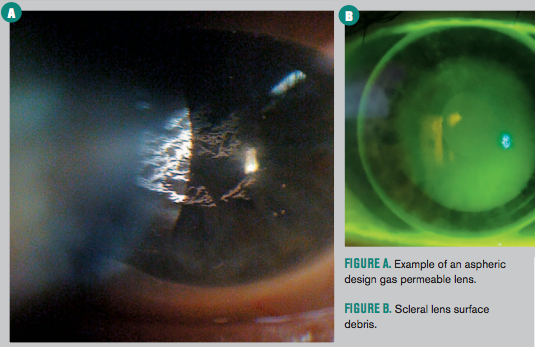
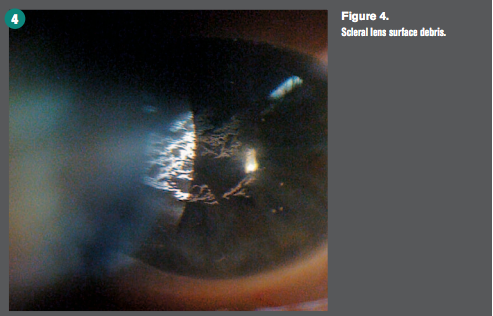
Lipids and mucins are attracted to the hydrophobic GP material, causing an uneven surface (Figure 4). Dry eye that includes filamentary keratitis can lead to poor surface wettability. Exposure from a cranial nerve palsy or lagophthalmos can also be risk factors for poor surface wettability. Treatment and management of ocular surface disease is imperative.
Prior to handling scleral lenses, all patients must wash hands with a mild, basic hand soap, contact lens hand soap, or acne treatment hand soap.
Related: Optimize patients' CL experience by avoiding 3 bad habits
Inform patients to apply face, eye creams and makeup after lens application. Patients should avoid oil-based moisturizers on the eyelids and avoid applying makeup to the inside area of the eyelid margin.
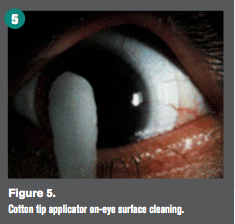
Management strategies include removing, cleaning and re-applying lenses midday; using on-eye surface cleaning techniques (Figure 5); or adding another cleaner added to nightly disinfection.
Lens coating Tangible Hydra-PEG was FDA approved in 2016. Tangible Hydra-PEG is made from the lubricant polyethylene glycol (PEG) and is a 90 percent water polymer mixture that is permanently bonded to the surface of the scleral lens. It encapsulates the lens, creating a mucin-like wetting surface which minimizes friction and surface deposition, shielding the lens from the ocular surface and tear film. Tangible Hydra-PEG improves wettability, lubricity, surface water retention, and tear break-up time.
Coated lenses are cleaned daily with a multi-purpose or peroxide-based solution. It is important to avoid abrasive or alcohol-based solutions. Tangible Hydra-PEG may last permanently, but duration is variable. Patients who are heavy depositors or have lagophthalmos may experience a shorter duration of effectiveness.
Because coated lenses will be more slippery, educate patients that the Tangible Hydra-PEG surface will result in a slicker lens. They may require a brief adjustment period for handling, applying, and removing lenses.
To obtain Tangible Hydra-PEG, contact a Tangible Hydra-PEG certified laboratory at www.tangiblescience.com. No changes to the scleral lens fit, prescription, or design are required when ordering lenses with Tangible Hydra-PEG.
4. Utilize back surface toricity
Back surface toricity incorporated into the scleral lens design may improve lens comfort.
In a 2006 study of 27 eyes wearing a spherical scleral lens, subjects experienced improved comfort and wearing time after being refit with a back toric design.6
In 2013, Visser et al evaluated 213 eyes fit with bitangential peripheral landing zones. This study confirmed the findings of the 2006 study. Lenses with bitangential peripheries provided good fitting characteristics (lens movement and position), improved visual acuity, and patient satisfaction.7
A 2015 study demonstrated that three lens stabilization methods incorporated into the posterior periphery of a scleral lens provided better stability than lenses with spherical peripheries.8
Related: Upgrade your patients to new technology
5. Allow scleral lenses to settle
Scleral lenses need time to settle into the scleral conjunctiva over time. Although the exact mechanism is unknown, settling results in reduced post-lens fluid reservoir depth.
During the scleral lens fitting process, allow lenses 20 to 30 minutes to settle prior to lens evaluation and over-refraction.
A 2016 study of 16 patients that evaluated how the change in fluid reservoir depth affects the total refractive power of the scleral lens/reservoir system determined that settling appeared to have a relatively small impact (0.25 D) on lens power needed to provide optimal visual acuity in this group of patients.9
Keep in mind that many factors that can lead to variability in settling amounts can occur during scleral lens wear.
6. Incorporate multifocal optics
Shortly after age 40, the most significant contact lens dropout rate occurs.
In patients under age 45, comfort concerns are the main reason for contact lens dropout. After age 45, vision and comfort are almost equally stated as the reason for contact lens dropout.10 Interestingly in the soft contact lens population, 93 percent of patients were not wearing multifocal contact lenses at the time of dropout.
Patients, especially those with astigmatism, often discontinue contact lens wear due to poor vision and are unaware that multifocal options exist.
Many novel multifocal scleral lens designs have been introduced to the market in the last few years.11 Multifocal scleral lenses can be used for both irregular and healthy/normal corneas. There is massive potential market growth for scleral multifocal lenses.
To be successful with multifocal lenses, scleral lenses should be precisely centered on the cornea. With smaller diameter scleral lenses, spherical peripheries may be used. However, if a larger lens is needed, toric peripheral curves may aid with lens centration.
If lens misalignment is present, the optics of the lens may be decentered to match the visual axis, enhancing the visual outcome. This process requires increased chair time and laboratory consultation. Your laboratory consultant can help determine the ideal multifocal design each patient.
7. Enhance performance with solutions
In order to optimize corneal health, utilize preservative-free solutions in the bowl of the scleral lens. Because solutions are in contact with the cornea for the length of scleral lens wear and there is minimal tear exchange with scleral lenses, preservative-free solutions help to maintain a healthy cornea.
LacriPure (Menicon) is an FDA approved solution for use as an application solution for scleral lenses after disinfection. LacriPure can also be used to rinse lenses prior to application and to rinse lens cases or lenses as needed during the day. This solution is a 5 mL sterile single-use unit dose preservative-free non-buffered, 0.9% NaCl (normal saline) solution.12
ScleralFil (Bausch + Lomb) is an FDA-approved preservative free, sterile, buffered isotonic saline solution that can be used for rinsing and applying scleral lenses. This solution is a 10-mL single-use dose. The solution contains boric acid, sodium borate, and sodium chloride in purified water.
Related: 7 strategies for fitting keratoconus patients
Prior to FDA-approved solutions, standard of care in the United States was non-FDA approved preservative-free 0.9% non-buffered sodium chloride inhalation solution in a single-use vial. Sodium chloride 0.9% inhalation solution may be obtained with a prescription from a pharmacy or purchased without a prescription online.
According to the SCOPE study, the majority of prescribers recommended preservative-free single use vials of 0.9% sodium chloride (60.2 percent) and sterile preservative-free saline (57.4 percent) to fill and apply lenses.13 Of note, participants could select multiple solutions in this study.
Hydrogen peroxide solutions are often a problem solver and are effective for all scleral lenses, particularly for patients sensitive to chemicals and preservatives in multipurpose solutions. Brands of hydrogen peroxide systems in the United States include Clear Care (Alcon) and PeroxiClear (Bausch + Lomb), which is currently recalled.
According to the SCOPE study, hydrogen peroxide-based systems were the most common recommended disinfection systems (61.4 percent), followed by gas permeable lens cleaner (37.8 percent), and gas permeable condition solution (33.8 percent).13 Participants could select multiple solutions in this study.
8. Immerse the ocular surface
Dry eye disease is a highly prevalent condition, ranging from 7 percent to 34 percent.14,15 Dry eye is a common and chronic condition where there are not enough tears or poor quality of tears to lubricate and nourish the eye.
Many different factors cause dry eye disease; this condition is more common in people 50 years old or older.16 Hormonal changes, especially in women, are a common cause of dry eye.17-19 Other conditions that can exacerbate dry eye symptoms include diabetes, glaucoma, Sjögren’s disease, lupus, and rheumatoid arthritis.
Medications can worsen dry eye symptoms, including antihistamines, hormonal replacement therapy, and androgen therapy. Environmental factors such as pollen or allergies, digital device or computer usage, overhead ceiling fans, or contact lens wear can worsen dry eye.20 In advanced stages of the condition, the severity of dry eye may damage the front surface of the eye and impair vision.
Dry eye may have multiple presentations and can range from mild to moderate to severe. In all forms of dry eye, especially in the severe ocular surface disease including Sjögren’s disease, graft versus host disease (GVHD), Stevens-Johnson syndrome, or limbal stem cell deficiencies, scleral lenses are an option to alleviate symptoms of dry eye that may be debilitating.21
Scleral lenses are advantageous to protect and lubricate the ocular surface. The post-lens fluid layer between the posterior surface of the scleral lens and the anterior portion of the cornea acts as a tear reservoir. This layer constantly bathes the cornea with scleral lens wear.
This tear reservoir can dramatically improve patient comfort and symptoms of dry eye. The scleral lens also serves as a barrier between the ocular surface and the outside environment, which can aid in protecting the eye.
The use of scleral lenses to manage ocular surface disease prior to the introduction of GP lenses, including exposure and neuropathic keratitis, neuropathic keratitis, and dry eye conditions, has been well documented in the literature.22-24 Several papers reported the use of scleral lenses manufactured with GP materials for ocular surface disease.25-28
Currently, scleral lenses have been reported to improve corneal epithelial integrity, vision-related quality of life, and visual acuity in patients with ocular surface disease.29-31
In clinical practice, patients who had failed or are intolerant to conventional GP contact lenses showed a significant improvement in quality of life.1
Related: How to establish value in the minds of contact lens wearers
9. Embrace scleral lenses for healthy eyes
Scleral lenses help optimize visual acuity with crisp optics from GP materials.32 Lenses can be customized to reduce higher order aberrations, glare, and halos.
Comfort is exceptional due to the minimal movement of scleral lenses that do not touch the cornea or limbus.
Scleral lens candidates are any patient wearing any type of contact lens, including soft and GP, who complains of discomfort or experiences visual disturbance.
Novel scleral lens designs and technology are available for patients with healthy/normal corneas and regular astigmatism. These patients are great candidates for scleral lenses, especially when their visual needs exceed standard soft lens parameters.
Patients with high astigmatism, refractive error, post-LASIK, along with presbyopia and mild-to-moderate dry eye are all candidates for scleral lenses.
By offering scleral lens technology to the healthy cornea population, not only are patients thrilled with the vision and comfort of scleral lenses, it profoundly enhances practice growth.
10. Utilize manufacturer consultants
Each scleral lens design has its own features and specifications. Because manufacturer laboratory consultants are experts in their specific lens designs, it is important to develop a close relationship to succeed with scleral lenses.
Scleral lens consultants can aid in designing the customizable features and capabilities of specific lens designs.
Additionally, in order to troubleshoot complicated cases, communicate with your laboratory consultant in order to achieve success. Even if you do not know exactly what needs to be altered, contact the laboratory consultant to be guided to a successful scleral lens result.
Scleral lenses can significantly improve our patients’ quality of life. However, scleral lenses may have their own complexities. These 10 pearls will help eyecare practitioners better succeed with the intricacies of scleral lens fitting.
References:
1. Picot, C, Gauthier AS, Campolmi, N, Delbosc B. Quality of life in patients wearing scleral lenses. J Fr Ophtalmol. 2015 Sep;38(7):615-9.
2. Pecego M, Barnett, M, Mannis MJ, Durbin-Johnson B. Jupiter Scleral Lenses: the UC Davis Eye Center experience. Eye Contact Lens. 2012 May;38(3):179-82.
3. Pullum, KW, Whiting MA, Buckley RJ. Scleral contact lenses: the expanding role. Cornea. 2005 Apr;24(3):269-77.
4. Ensley, R, Miller, H. Good Chemistry. Rev Cornea CL. Available at: http://www.reviewofcontactlenses.com/content/c/59290/. Accessed 6/14/17.
5. Scleral Lens Education Society Website. Sclerallens.org, June, 2015.
6. Visser ES, Visser R, Van Lier HJ. Advantages of toric scleral lenses. Optom Vis Sci. 2006 Apr;83(4):233-6.
7. Visser ES, Van der Linden BJ, Otten HM, Van der Lelij A, Visser R. Medical applications and outcomes of bitangential scleral lenses. Optom Vis Sci. 2013 Oct;90(10):1078-85.
8. Ticak A, Marsack JD, Koenig DE, Ravikumar A, Shi Y, Nguyen LC, Applegate RA. A Comparison of Three Methods to Increase Scleral Contact Lens On-Eye Stability. Eye Contact Lens. 2015 Nov;41(6):386-90.
9. Britton S, Bray C, Yeung D, Haines L, Sorbara L. Changes in over-refraction after scleral lens settling. Poster presented at Global Specialty Lens Symposium. Las Vegas, NV. January 2016.
10. Brujic M, Miller, J. Minimizing Dropouts: What You Can Do. Review of Cornea and Contact Lens. Available at: http://www.reviewofcontactlenses.com/content/c/27244/. Accessed 6/14/17.
11. Barnett, M. Multifocal Scleral lenses. CL Spectrum. Available at: http://www.clspectrum.com/issues/2015/december-2015/multifocal-scleral-lenses. Accessed 6/15/17.
12. Food and Drug Administration. Menicon Saline Rinse Solution approval letter. Available at: https://www.accessdata.fda.gov/cdrh_docs/pdf15/K151768.pdf. Accessed 6/15/17.
13. Shorter, E, Barr, J, Nau, A, Nau C, Harthan, J, Schornack M. SCOPE Study: Current consensus of prescribers’ scleral lens wear and care recommendations. Poster presented at American Academy of Optometry Annual Meeting, October 2015.
14. Lin PY, Tsai SY, Cheng CY, Liu JH, Chou P, Hsu WM. Prevalence of dry eye among an elderly Chinese population in Taiwan: The Shihpai Eye Study. Ophthalmology. 2003 Jun;110(6):1096-1101.
15. McCarty CA, Bansal AK, Livingston PM, Stanislavsky YL, Taylor HR. The epidemiology of dry eye in Melbourne, Australia. Ophthalmology. 1998 Jun;105(6):1114-1119.
16. Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. Am J Ophthalmol. 2003 Aug;136(2):318-26.
17. Chia EM, Mitchell P, Rochtchina E, Lee AJ, Maroun R, Wang JJ. Prevalence and associations of dry eye syndrome in an older population: the Blue Mountains Eye Study. Clin Exp Ophthalmol. 2003 Jun;31(3):229-232.
18. Erdem U, Ozdegirmenci O, Sobaci E, Göktolga U, Dagli S. Dry eye in postmenopausal women using hormone replacement therapy. Maturitas. 2007 Mar 20;56(3):257-262.
19. Uncu G, Avci R, Uncu Y, Kaymaz C, Develioßlu O. The effects of different hormone replacement therapy regimens on tear function, intraocular pressure and lens opacity. Gynecol Endocrinol. 2006 Sep;22:501-505.
20. Kumar N, Feuer, W, Lanza NL, Galor A. Seasonal Variation in Dry Eye. Ophthalmology. 2015 Aug;122(8):1727-1729.
21. Schornack MM. Scleral lenses: a literature review. Eye Contact Lens. 2015 Jan;41(1):3-11.
22. Klein M. Contact Lens in Cases of Neuroparalytic Keratitis. Br J Ophthalmol. 1943 May;27(5):221-2.
23. Constable JD, Carroll JM. The emergency treatment of the exposed cornea in thermal burns. Plast Reconstr Surg. 1970 Sep;46(3):309-12.
24. Rosenthal P, Cotter JM, Baum J. Treatment of persistent corneal epithelial defect with extended wear of a fluid-ventilated gas-permeable scleral contact lens. Am J Ophthalmol. 2000 Jul;130(1):33-41.
25. Schornack M, Pyle J, Patel SV. Scleral Lenses in the Management of Ocular Surface Disease. Ophthalmol. 2014 Jul;121(7):1398-405.
26. Gould HL. Management of the dry eye using scleral lenses (a report on 66 cases). Eye Ear Nose Throat Mon. 1970 Mar;49(3):133-40.
27. Kok JH, Visser R. Treatment of ocular surface disorders and dry eyes with high gas permeable scleral lenses. Cornea. 1992 Nov;11(6):518-22.
28. Rosenthal, P, Cotter J. The Boston Scleral Lens in the management of severe ocular surface disease. Ophthalmol Clin North Am. 2003 Mar;16(1):89-93.
29. Pullum K, Buckley R. Therapeutic and ocular surface indications for scleral contact lenses. Ocul Surf. 2007 Jan;5(1):40-8.
30. Blackmore SJ. The use of contact lenses in the treatment of persistent epithelial defects. Contt Lens and Anterior Eye. 2010 Oct;33(5):239-244.
31. Bavinger JC, DeLoss K, Mian SI. Scleral lens use in dry eye syndrome. Curr Opin Ophthalmol. 2015 Jul;26(4):319-24.
32. Michaud L, Barriault C, Dionne A, Karwatsky P. Empirical fitting of soft or rigid gas-permeable contact lenses for the correction of moderate to severe refractive astigmatism: a comparative study. Optometry. 2009 Jul;80(7):375-83.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.