Multiple diagnostic modalities for x-linked retinoschisis
A six-year old white male presented for low vision rehabilitation with a history of X-linked retinoschisis (XLRS). He reported blurred vision for a year.

A six-year old white male presented for low vision rehabilitation with a history of X-linked retinoschisis (XLRS). He reported blurred vision for a year. His medical history was unremarkable. His family ocular history was positive for X-lined retinoschisis, including a brother and an uncle.
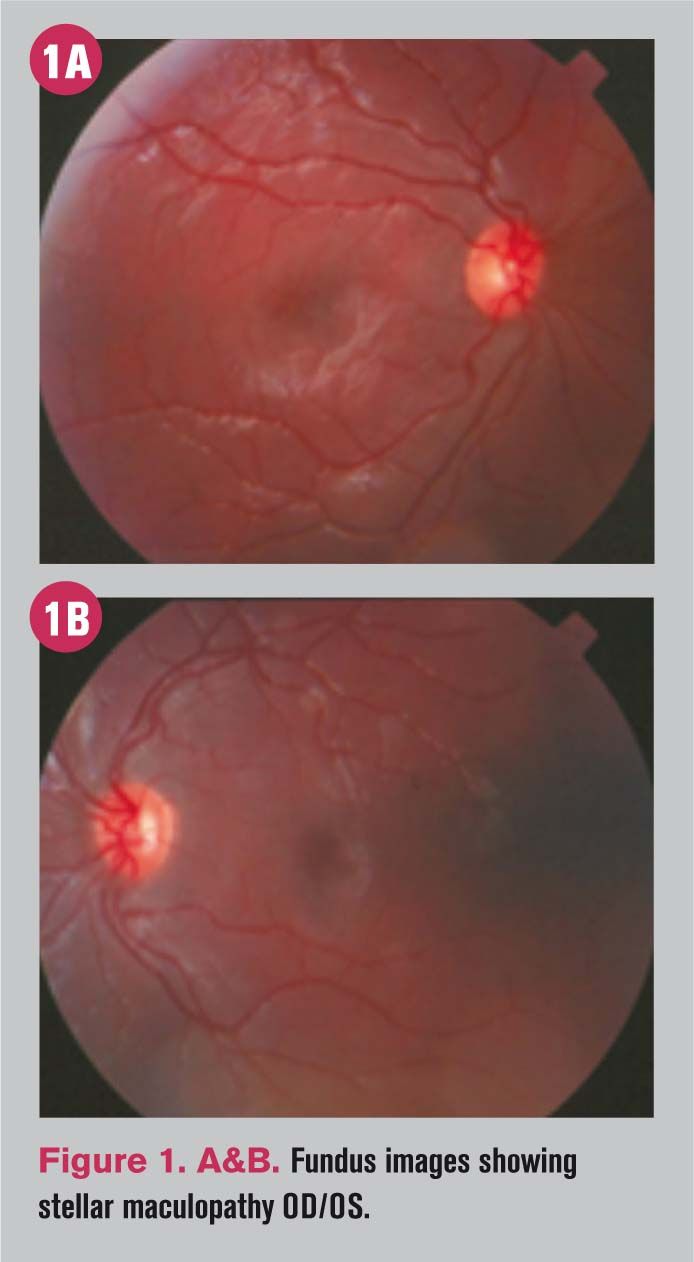
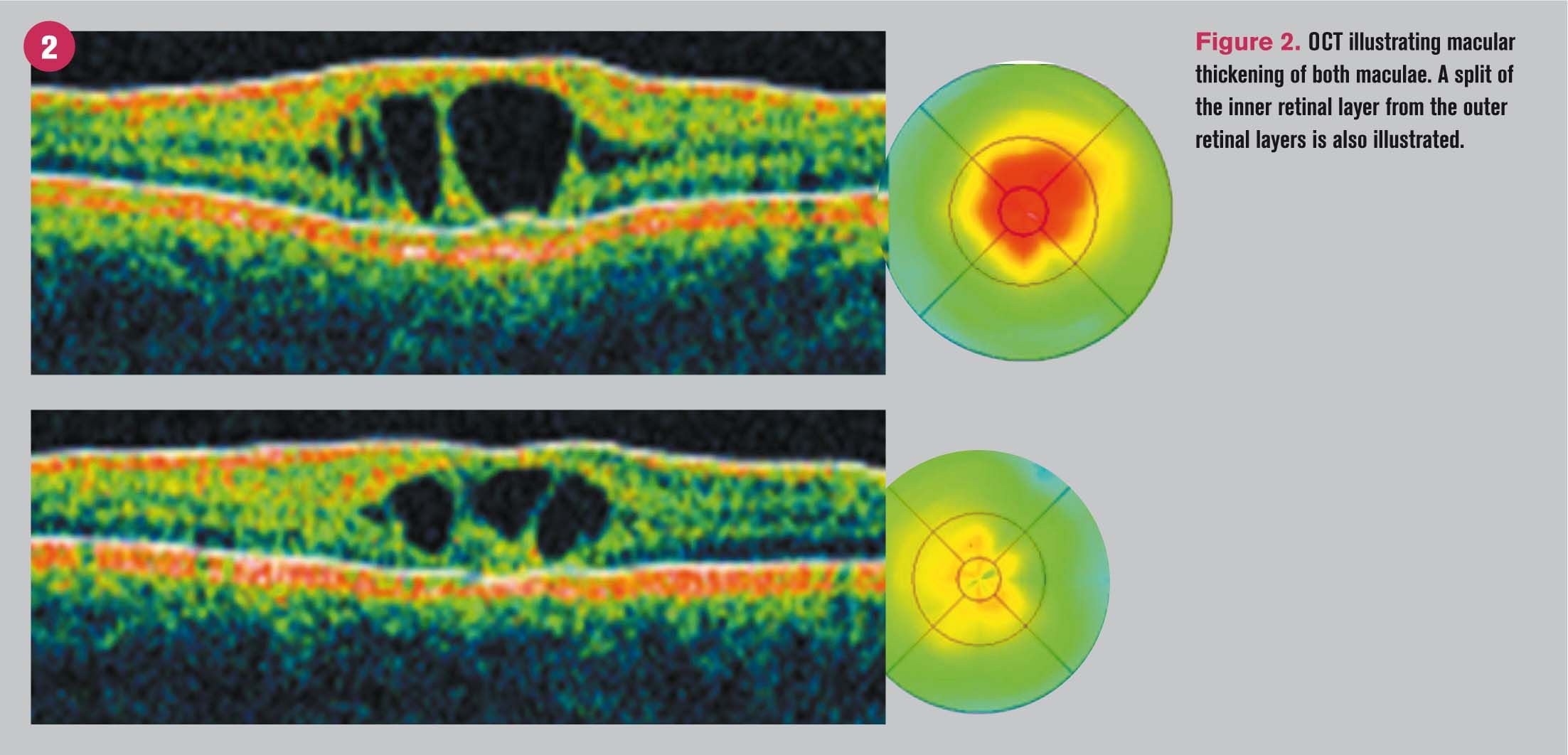
Best-corrected visual acuity was 20/100 OD and 20/80 OS. Preliminary testing and anterior segment findings were unremarkable for age. Dilated fundus exam revealed symmetrical stellate pattern bilaterally without associated findings. The peripheral fundus was flat and attached without predisposing conditions to retinal detachment. An OCT was ordered, which revealed a neurosensory retinal split with associated columnar defects found within the split. Thickening of the macula was evident topographically. Previously obtained ERG revealed an electro negative response.
More from Dr. Semes: Evaluating myopic maculopathy
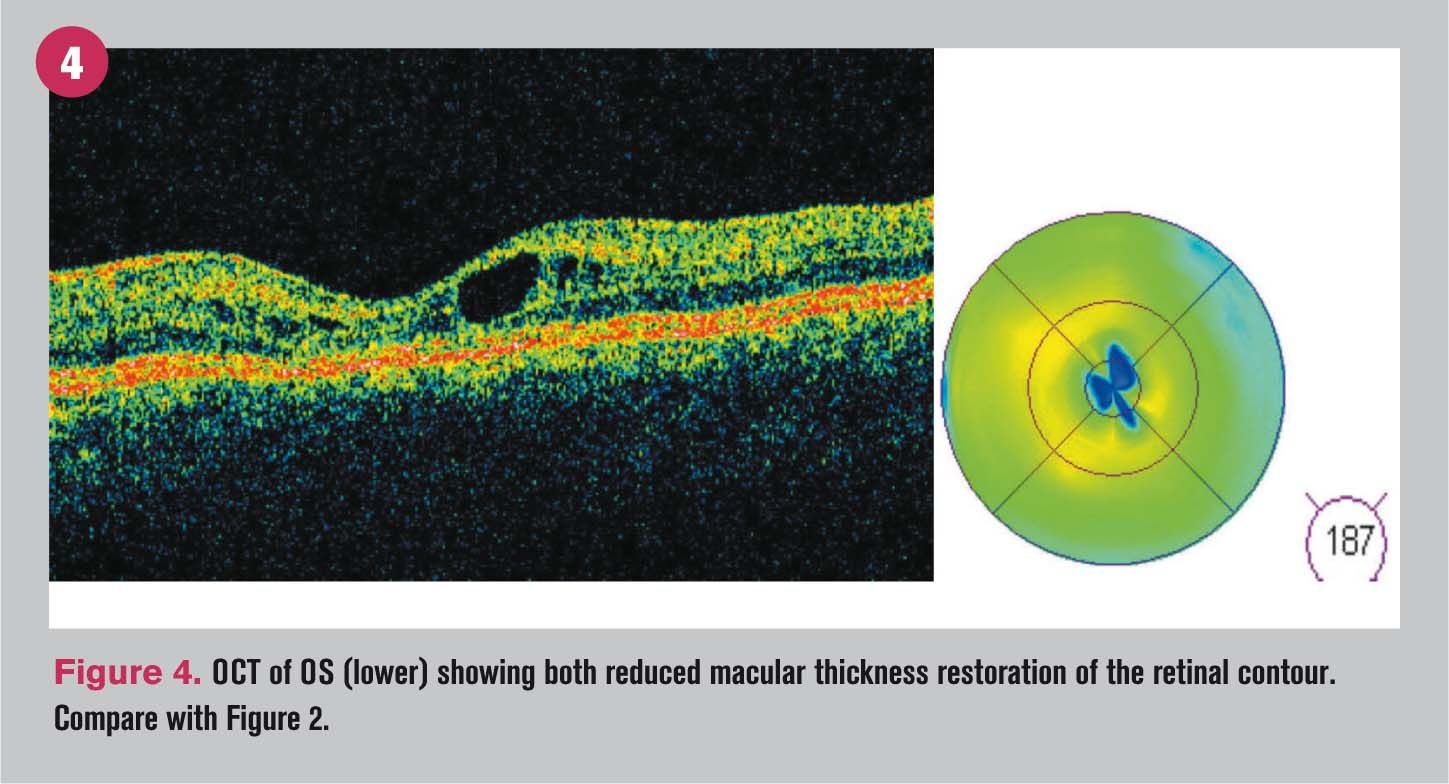
At a follow-up visit four months later, visual acuity was 20/80+2 OD and 20/60+2 OS, correlating with notably decreased macular thickness. Normalization of the foveal pit OD and restoration of the macular contour OS was also noted. This result was in response to treatment with timolol maleate 0.05% (Timoptic, Bausch + Lomb) and dorzolamide 1% (Trusopt, Merck) as a treatment option for patients with XLRS. The patient had been treated for two months, and he was under the care of a retinal specialist who had enrolled him in an NEI clinical trial.
Click here to see the images







Next: XLRS clinical presentation and diagnosis
XLRS clinical presentation and diagnosis
X-linked retinoschisis (XLRS) or juvenile retinoschisis is an inherited retinal degeneration characterized by the splitting of the neurosensory retinal layers. Retinoschisis affects males almost exclusively, and in fact it is one of the most common macular degenerations associated with visual impairment in that group.1 Although the retinoschisis principally affects that macula, 50 percent of patients develop peripheral retinoschisis.2
The classic clinical presentation is described as symmetrical bilateral radiating inner retinal layer cystic-like defects (spoke pattern). Patients generally are discovered due to reduced visual acuity during the first decade of life. Visual impairment by school age progresses to 20/200 by age 60. XLRS is caused by a mutation of the RS1 gene localized to the short arm of the X-chromosome. The inherited defect affects the Muller cells.3
More from Dr. Semes: Anti-VEGF treatment helps diabetic patient
Although the diagnosis is often based on clinical observation, ancillary testing such as optical coherence tomography (OCT), molecular genetic and electrophysiologic testing have been particular useful.4,5 Photography with red-free may also help enhance the view of the macular stellate appearance. OCT images clearly show the split affecting the neurosensory retina with apparent bands localized vertically within the schisis cavity, representing Muller cell stretching. An increase in macular thickness will also be noted. The OCT findings may be similar to cystoid macular edema (CME), but given that this is a morphological changes, the corresponding fluorescein angiography will not show any associated leakage.6 Classic ERG findings will denote the electro negative respond, correlating to inner retinal layer dysfunction.5
More from Dr. Semes: A closer look at the retina in multiple sclerosis
Over the years, genetic testing has elucidated the understanding of the disease. XLRS is linked to variable mutations in the RS1 gene, which codes for the retinoschisin protein.3,7 At the molecular letter retinoschisin is instrumental in cell adhesion of the inner nuclear layer. Retinoschisin also supports synaptic connections between bipolar cells and photoreceptors.7 In patients with XLRS, defective Muller cells lose normal contact with neighboring cells.3,7 This allows for the accumulation of retinoschisin both extracellularly and intracellularly. It is believed that this accumulation corresponds to the cystic-like spaces.7
In recent years, carbonic anhydrase inhibitors have shown some efficacy as an effective, albeit intermittent, treatment option for patients with XLRS. The current case illustrates short-term improvement in response to the off-label use of fixed-combination 0.5% timolol maleate and 1% dorzolamide.8-12
References
1. Prenner JL, Capone A Jr, Ciaccia S, Takada Y, Sieving PA, Trese MT. Congenital X-linked retinoschisis classification system. Retina. 2006 Sep;26(7 Suppl):S61-4.
2. George ND, Yates JR, Moore AT. X-linked retinoschisis. Br J Ophthalmol. 1995 Jul; 79(7):697-702.
3. Chan WM, Choy KW, Wang J, Lam DS, Yip WW, Fu W, Pang CP. Two cases of X-linked juvenile retinoschisis with different optical coherence tomography findings and RS1 gene mutations. Clin Experiment Ophthalmol. 2004 Aug;32(4):429-32.
4. Ericksson U, Larsson E, Holmström G. Optical coherence tomography in the diagnosis of juvenile X-linked retinoschisis. Acta Ophthalmol. Scand. 2004 Apr;82(2):218-23.
5. Peachey NS, Fishman GA, Derlacki DJ, Brigerr MG. Psychophysical and electroretinographic findings in X-linked juvenile retinoschisis. Arch Ophthalmol. 1987 Apr;105(4):513-6.
6. Apushkin MA, Fishman GA, Janowicz MJ. Correlation of optical coherence tomography findings with visual acuity and macular lesions in patients with X-linked retinoschisis. Ophthalmology. 2005 Mar;112(3):495-501.
7. Molday LL, Hicks D, Sauer CS, Weber BH, Molday RS. Expression of the X-linked retinoschisis protein RS1 in photoreceptor and bipolar cells. Invest Ophthalmol Vis Sci. 2001 Mar;42(3):816-25.
8. Apushkin MA, Fishman GA. Use of dorzolamide for patients with X-linked retinoschisis. Retina. 2006 Sep;26(7):741-5.
9. Ghajarnia M, Gorin MB. Acetazolamide in the treatment of X-linked retinoschisis maculopathy. Arch Ophthalmol. 2007 Apr;125(4):571-3.
10. Gurbaxani A, Wei M, Succar T, McCluskey PJ, Jamieson RV, Grigg JR. Acetazolamide in retinoschisis: a prospective study. Ophthalmology. 2014 Mar;121(3):802-3.e3.
11. Collision FT, Genead MA, Fishman GA, Stone EM. Resolution of mid-peripheral schisis in x-linked retinoschisis with the use of dorzolamide. Ophthalmic Genet. 2014 Jun;35(2):125-7.
12. Rocha Cabrera P, Pareja Rios AC, Cordoves Dorta L, Mantolan Sarmiento C, Serrano Garcia MA. A combination of topical and systemic carbonic anhydrase in the treatment of chromosome X-linked retinoschisis. Arch Soc Esp Oftalmol. 2014 Aug;89(8):320-3.