Multiple sclerosis and optometry
Multiple sclerosis (MS) is a complex neuro-inflammatory disorder that can result in diplopia, optic neuritis, and myelin loss in around the optic nerve. Optical coherence tomography (OCT) findings have been useful in investigating retinal parameters measured by OCT. For patients with MS, there are several treatment options available that include injectable and oral medications.
Multiple sclerosis (MS) is a complex neuro-inflammatory disorder affecting about 400,000 Americans.1 MS isn’t a single disorder, but a family of disorders categorized by the disease course. There are four major forms of MS:
- Relapsing-remitting. The most familiar form, and consequently the one most seen at the time of diagnosis (85%).1 Relapsing-remitting is characterized by acute episodes of neurological symptoms followed by complete or partial recovery of function. Optometrists are most likely familiar with this form which occurs in patients who present with an acute episode of diplopia or optic neuritis that clears over a period of weeks to months.
- Primary progressive. Has a slow downhill course from the beginning, with no distinct episodes or relapses.
- Secondary progressive. Occurs in patients who initially present with relapses and remissions, but these patients later convert to a progressive downhill course. About 50% of MS patients initially diagnosed with the relapsing-remitting form convert to the secondary progressive form within 10 years of the initial episode.1
- Progressive relapsing. The least common of the forms (5%). In this type, the course is initially progressive, but punctuated by definite neurological episodes.1 Unlike the patient with typical relapsing-remitting MS, patients with this form don’t recover function after acute episodes.
Benchmarking MS
Early diagnosis of MS is important for both treatment and counseling purposes. The McDonald criteria are the most common set of clinical guidelines used to diagnose MS.2 These criteria were developed in 2001 by an international working group and revised in 2010. The diagnosis of MS is marked by the concepts of separation in space and separation in time. In general, two separate documented neurological episodes (in time) consistent with MS and not associated with fever are needed to diagnose the disease. This may be supported by lesions seen on T2 weighted magnetic resonance imaging (MRI) images in separate locations (in space) of the central nervous system or with new lesions documented on repeated MRI scans (in time).
In 2008, the 15-year results of the Optic Neuritis Treatment Trial were released.3 The primary outcome of interest was determining the best way to treat acute non-arteritic optic neuritis, but a secondary goal was to determine the rate of MS diagnosis among the subjects. All subjects in the trial were experiencing their first episode of optic neuritis and didn’t carry a diagnosis of MS at the time they entered the study. By 15 years out, 50% of all subjects were diagnosed with MS. The rate was much higher (72%) among those subjects whose initial MRI scans were positive for brain plaques consistent with MS than among subjects who didn’t have lesions (25%).
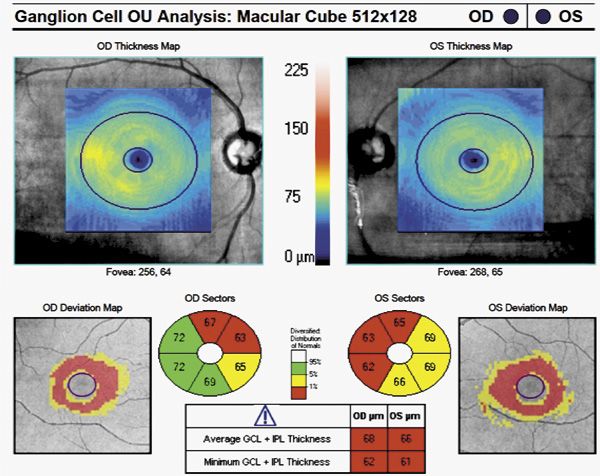
Figure 1. Ganglion cell complex analysis in a patient recently diagnosed with relapsing remitting multiple sclerosis.
OCT and MS
The McDonald criteria recommend the use of visually evoked potential (VEP) as a marker for MS episodes among those with previous visual symptoms, similar to MRI for general CNS lesions. The 2010 paper reporting the McDonald criteria mentioned optical coherence tomography (OCT) as a potential substitute for VEP without endorsing its use.2 However, that report recommended further study. Along this line, the past 7 years have seen an explosion of studies looking at retinal parameters measured by OCT as biomarkers for a host of neurodegenerative disorders, including MS.
The initial study of the relationship of OCT findings to MS appeared in 1999. The results showed a correlation between the retinal nerve fiber layer (RNFL) thickness and electrophysiology results in MS patients with a previous episode of optic neuritis.4 Study in the area went silent until 2006, when new papers began to be published, and the pace has not slowed since. The overarching goal of recent research into OCT and MS has been to determine whether OCT-measured retinal parameters are associated with the level of disease in MS patients regardless of a history of clinical episodes of optic neuritis. Post-mortem studies of persons with MS have shown a strong disease predilection for the optic nerve with almost 95% to 100% showing demyelination at autopsy.5 The mechanism of retinal involvement in MS is thought to be retrograde degeneration of the nerve fiber layer and ganglion cell layer (both thinned) in response to myelin loss in around the optic nerve beyond the lamina.5
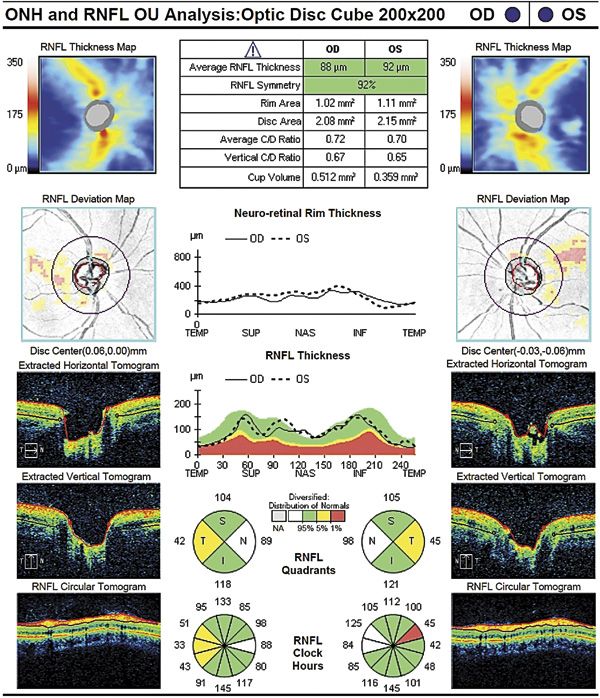
Figure 2. Normal nerve fiber layer analysis in the same patient.
Most studies of OCT parameters and MS have shown good correlation between the overall peripapillary RNFL thickness and ganglion cell complex (GCC) thickness with the length of time a person has had MS as well as the patient’s reported disability level.5 In general, studies have shown that GCC has a slightly better correlation to both disease and disability than RNFL thickness. Deeper retinal layer thickness (inner nuclear/outer nuclear) has also been shown to be thinned with some speculation that this may be due to more retina-specific MS findings, like periphlebitis.5 A study published in the January issue of JAMA Neurology reported GCC thickness and peripapillary RNFL thickness were associated with intracerebral gray matter volume and white matter volume in the cerebellum and brainstem. Inner nuclear layer thickness was shown to correlate to the results of fluid attenuated inversion recovery (FLAIR) MRI, which is particularly useful in MS, by showing periventricular white matter lesions.5 A serendipitous finding in this study was the association of retinal OCT parameters to intracranial volume in normal subjects. The usefulness of OCT findings in MS is an evolving area. In the not too distant future, OCT may be a recommended test for all diagnosed MS patients.
Treatment options
For patients with MS, there are more treatment options available than ever before.1 The majority of treatments are targeted at the relapsing-remitting form and aimed at lengthening the time between relapses. Treatment options for the progressive forms are, unfortunately, limited.
In 1993, injectable interferon β-1b (marketed using the brand names Betaseron [Bayer] and Extavia [Novartis]) was shown to reduce the number of relapses in MS by about one-third. Since that time, interferon β-1a (Avonex [Biogen Idec], Rebif [EMD Serono]) injection has also been shown to be effective at reducing relapses. The interferons continue to be the first-line treatment for MS. Their main limitation is painful injection and infection risk. Mitoxantrone (Novantrone, EMD Serono), glatiramer (Copaxone, Teva), and natalizumab (Tysabri, Biogen Idec]) are effective second-line drugs, but they carry a much higher risk profile than do the interferons. Natalizumab has also shown benefit as a first-line drug. Glatiramer has also drawn interest for its potential neuroprotective effects in glaucoma. Three new oral medications have also become available-fingolimod (Gilenya, Novartis), teriflunomide (Aubagio, Genzyme), and dimethyl fumarate (Tecfidera, Biogen Idec). The yearly cost of these medications is $45,000 to 60,000 per year.
Fingolimod is of interest to optometrists as it has been shown to carry an increased risk of a reversible macular edema. Fingolimod is an analog to sphingosine-1-phosphate, a messenger that normally closes vascular endothelial junctions.6 For reasons that are not clearly understood, fingolimod opens rather than closes vascular junctions in the retina. The sphingosine-1-phosphate pathway has drawn attention and is currently under study in diabetic macular edema and macular degeneration. The current recommendations for patients going on fingolimod are a baseline eye exam before and 3 to 4 months after starting the drug. Optometrists should consider adding an OCT for both drug effects and disease monitoring if asked to see these patients.ODT
References
1. National Multiple Sclerosis Society. What is Multiple Sclerosis? http://www.nationalmssociety.org/about-multiple-sclerosis/what-we-know-about-ms/what-is-ms/index.aspx. Accessed June 10, 2013.
2. Polman CH, Reingold SC, Banwell B, Clanet M, et al . Diagnostic criteria for multiple sclerosis: 2010 Revisions to the McDonald criteria. Ann Neurol. 2011 February; 69(2):292–302.
3. The Optic Neuritis Study Group. Multiple Sclerosis Risk after Optic Neuritis: Final Optic Neuritis Treatment Trial Follow-Up. Arch Neurol. 2008 June; 65(6): 727–732.
4. Parisi V, Manni G, Spadaro M, Colacino G, et al. Correlation between morphological and functional retinal impairment in multiple sclerosis patients. Invest Ophthalmol Vis Sci. 1999 Oct;40(11):2520-2527.
5. Saidha S, Sotirchos ES, Oh J, Syc SB, et al. Relationships between retinal axonal and neuronal measures and global central nervous system pathology in multiple sclerosis. JAMA Neurol. 2013;70(1):34-43.
6. Jain N, Bhatti MT. Fingolimod-associated macular edema: incidence, detection, and management. Neurology. 2012 Feb 28;78(9):672-680.
4 categories of MS
Multiple sclerosis is categorized into 4 major forms.
1. Relapsing-remitting
2. Primary progressive
3. Secondary progressive
4. Progressive relapsing
Author Info

Dr. Swanson is associate professor of optometry and chief of ocular disease and low vision services at University of Alabama School of Optometry. His interests include the epidemiology and functional vision impact of vision disorders among the elderly. E-mail him at mswanson@uab.edu.
Take-Home Message
Multiple sclerosis (MS) is a complex neuro-inflammatory disorder that can result in diplopia, optic neuritis, and myelin loss in around the optic nerve. Optical coherence tomography (OCT) findings have been useful in investigating retinal parameters measured by OCT. For patients with MS, there are several treatment options available that include injectable and oral medications.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.