New technology may lead to earlier AMD Diagnosis
While there have been advances in the treatment of AMD, the methods to detect and diagnose AMD have remained the same, with the exception of OCT. But new technology-including the Adapt Dx, multi-spectral imaging, and fundus autofluorescence-may allow for earlier detection.
Great advances have been made over the last decade in the treatment of age-related macular degeneration (AMD) since the advent of Macugen (pegaptanib, Eyetech, Pfizer) in 2004. As most clinicians are aware, the current mainstay of treatment for wet or neovascular AMD is serial injections of anti-VEGF agents, most notably Lucentis (ranibizumab, Genentech), Avastin (bevacizumab, Genentech), and Eylea (aflibercept, Regeneron), the newest FDA-approved agent.
However, despite advances in treatment of AMD, the diagnosis methods to detect and diagnose AMD have remained relatively the same over the same period, with the obvious exception of OCT. Fortunately, new technology may soon allow us to detect AMD sooner than our current screening methods.
Dark adaptation
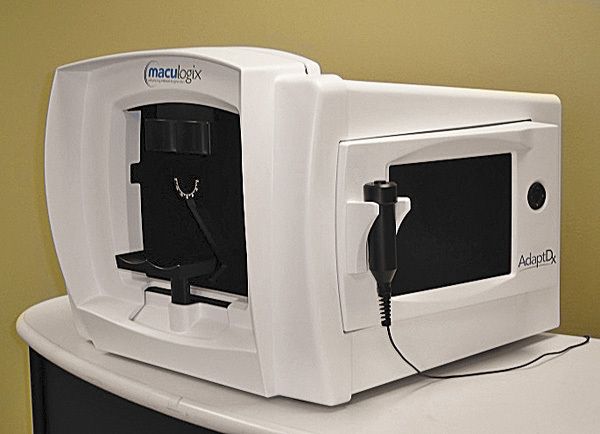
The Adapt Dx (Maculogix) is based on the functional test of dark adaptation-that is, the transition from being light-adapted to being dark adapted. Specifically, it measures the rate of recovery of scotopic sensitivity after photobleaching. Several studies at University of Alabama at Birmingham (UAB) have determined that dark adaptation is impaired with AMD.1 Further, there is a marked deterioration of dark adaptation speed as the disease progresses.2
According to this same study, dark adaptation is impaired up to 4 years before AMD is clinically relevant, with mean recovery time of AMD patients twice that of age matched normal adults. In an unpublished study conducted at Penn State University, the instrument was shown to have excellent sensitivity and specificity, 88% and 100% respectively. A second study at Penn State University revealed even better sensitivity of 91%.
The instrument itself is approximately the same size of a Humphrey Visual Filed Analyzer. Patients are exposed to a brief camera flash, and then instructed to respond when they detect a progressively dimmer spot of light presented near the macula. The screening test in non-invasive and can be completed within 5 minutes or less by a technician. If results are found to be abnormal, a more extensive threshold test may be performed. There is currently an established CPT code for dark adaptometry (92284) that has a reimbursement between $60 and $80. However, it is important to note that the AdaptDx is cleared for sale only as a dark adaptometer by the FDA-not approved as a test for AMD. It is currently under investigation as a diagnostic test for AMD, but as of this time is not cleared by the FDA.3
Multi-spectral imaging
Multi-spectral imaging (MSI) is an emerging technology that uses various wavelengths in order to better evaluate the retina and choroid for changes. Essentially, multiple monochromatic wavelengths from 550nm to 780 nm are used to visualize the retina in spectral slices, all the way from the internal limiting membrane ILM to the choroid. In general, the shorter wavelengths are used to visualize the more anterior surfaces, while the longer wavelengths are used to reflect the deeper structures, including the choroid. It is thought that by examining the choroid, RPE, and deeper tissues, the clinician may be able to visualize changes in the RPE representing early AMD prior to it becoming clinically apparent.4 This earlier diagnoses may prompt the clinician to counsel patients earlier or more aggressively regarding diet, vitamin supplements, or other modifiable risk factors for AMD.
One company’s system, the Annidis RHA, also adds additional features to its commercially available unit. It has additional imaging that can be used to highlight oxygenated and deoxygenated hemoglobin, which may relate to the metabolic activity of the retina. The MSI technology is also available under the name Multi Color as a cSLO through Heidelberg.
Fundus autofluorescence
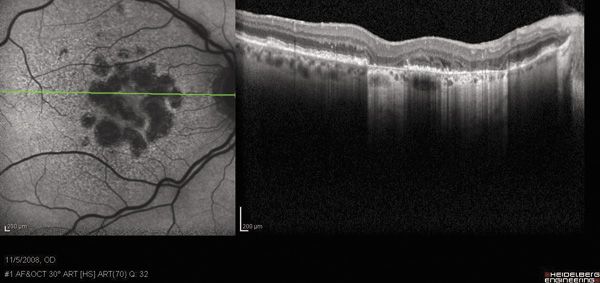
Fundus autofluorescence (FAF) is a non-invasive technique which uses the properties of lipofuscin to help analyze the heath of the retina. Lipsofuscin is a byproduct of damaged outer segment photoreceptors that accumulates in the RPE with age and with certain retinal disease. Hence, it serves a s a precursor to retinal damage and eventually death.5 When exposed to short to medium wavelength visual light, liposfuscin autofluoresce.
The images obtained by FAF appear somewhat similar to images associated with more traditional flourescein angiography but without needing to inject any dye. Increased areas of lipofuscin appear as bright, hyperfuorescent areas, whereas the absence of lipofuscin appears dark, or hyofluorescent.
FAF imaging can be obtained in two ways: either with confocal scanning laser ophthalmoscope (cSLO) or by filter based cameras. Instruments such as the Daytona by Optos, or under the trade name Blue Peak through Heidelberg, capture retinal FAF using a low-energy laser that excites the lipofuscin. Filter based cameras such at the Canon CX-1 uses a excite filter with high energy white flash to get the same results.
Currently, FAF is probably most useful in AMD for documenting the development and progression of geographic atrophy (GA).6 The exact borders of the GA can be much more readily identified than by clinical appearance or standard color photography, perhaps giving a more accurate assessment of the true extent of the atrophy. Further, some studies have indicated that hyperfluorescent borders surrounding a GA lesion may be the best predictor for advancement.6
Early diagnosis of AMD will be paramount as the population continues to age. Earlier detection may mean earlier intervention, such as alteration of risk factors such as smoking, poor diet, and obesity. It may also mean starting patients sooner on vitamin therapy in hopes of preventing the decline to advanced AMD. It may also mean more frequent monitoring for patients found to have AMD by these new diagnostic measures, in hopes of detecting advancing AMD or worse yet, conversion to wet AMD. Ultimately, these new techniques and equipment will hopefully help our patients maintain better vision and a better quality of life as they age.ODT
References
1. Jackson GR, Owsley C., Curio CA. Photoreceptor degeneration and dysfunction in aging and age-related maculopathy. Ageing Res Rev. 2002 June: 1(3): 381-86.
2. Oslwey C, McGwin G, Jackson GR, et al. Effect of short-term high-dose retinol on dark adaptation in aging and early age-related maculopathy. Invest Ophthalmol Vis Sci. 2006 Apr;47(4):1310-8.
3. MacuLogix Web site. http://maculogix.com/adaptdx. Accessed December 12, 2013.
4. Hitchmoth DL. Multispectral Imaging: A revolution in retinal diagnosis and health assessment. Advanced Ocular Care. 2013: May/June: 1-4.
5. Von Ruckman A, Fitzke FW, Bird AC. Distribution of fundus autoflorescence with a scanning laser ophthalmoscope. Br J Ophthalmol. 1995 May: 79(5): 407-12.
6. Holz FG, Bindewald-Wittich A, Fleckenstein M, et al. Progression of geographic atrophy and impact of fundus autoflourescence patterns in age-related macular degeneration. Am J Ophthalmol. 2007 Mar:143(3): 463-72.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.