Patient perception of good vision a trap leading to loss
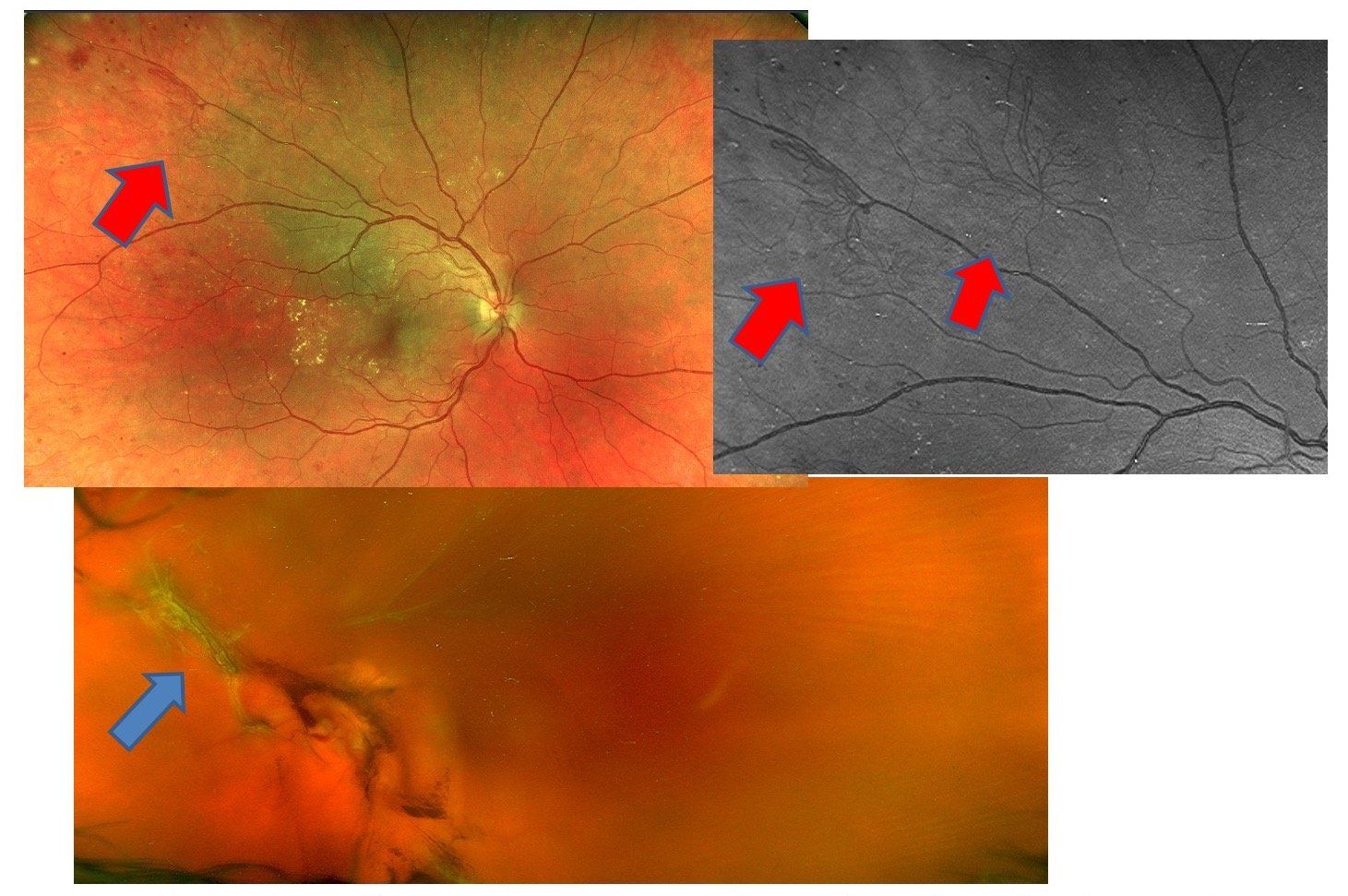
Figure 2. OCT topographical map shows localized non-centered thickening (blue arrow). Cross-section tomography shows intraretinal exudates (red arrow).
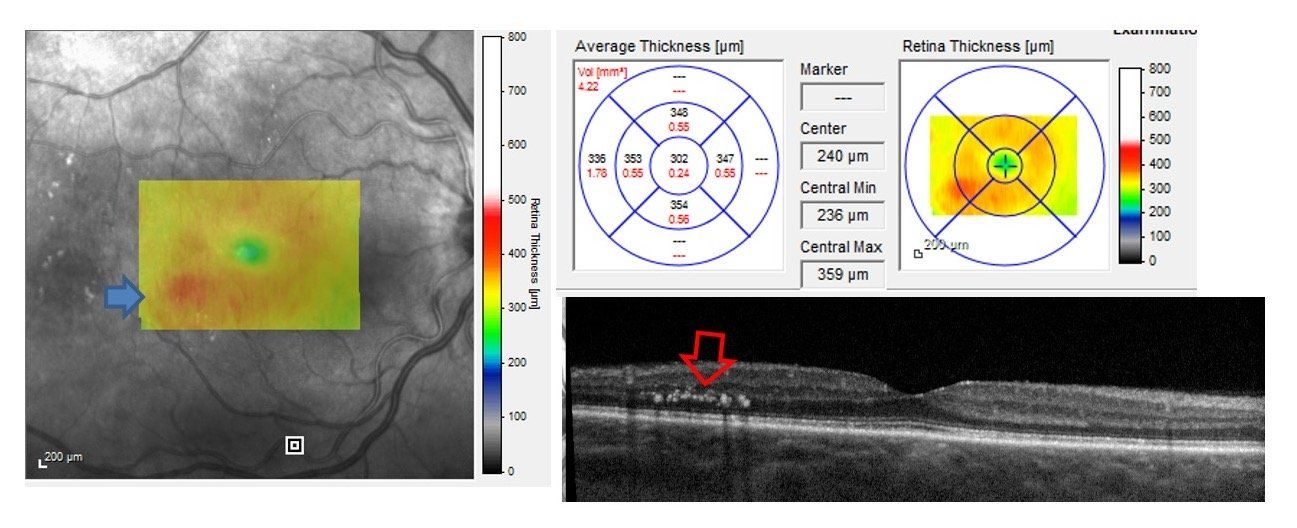
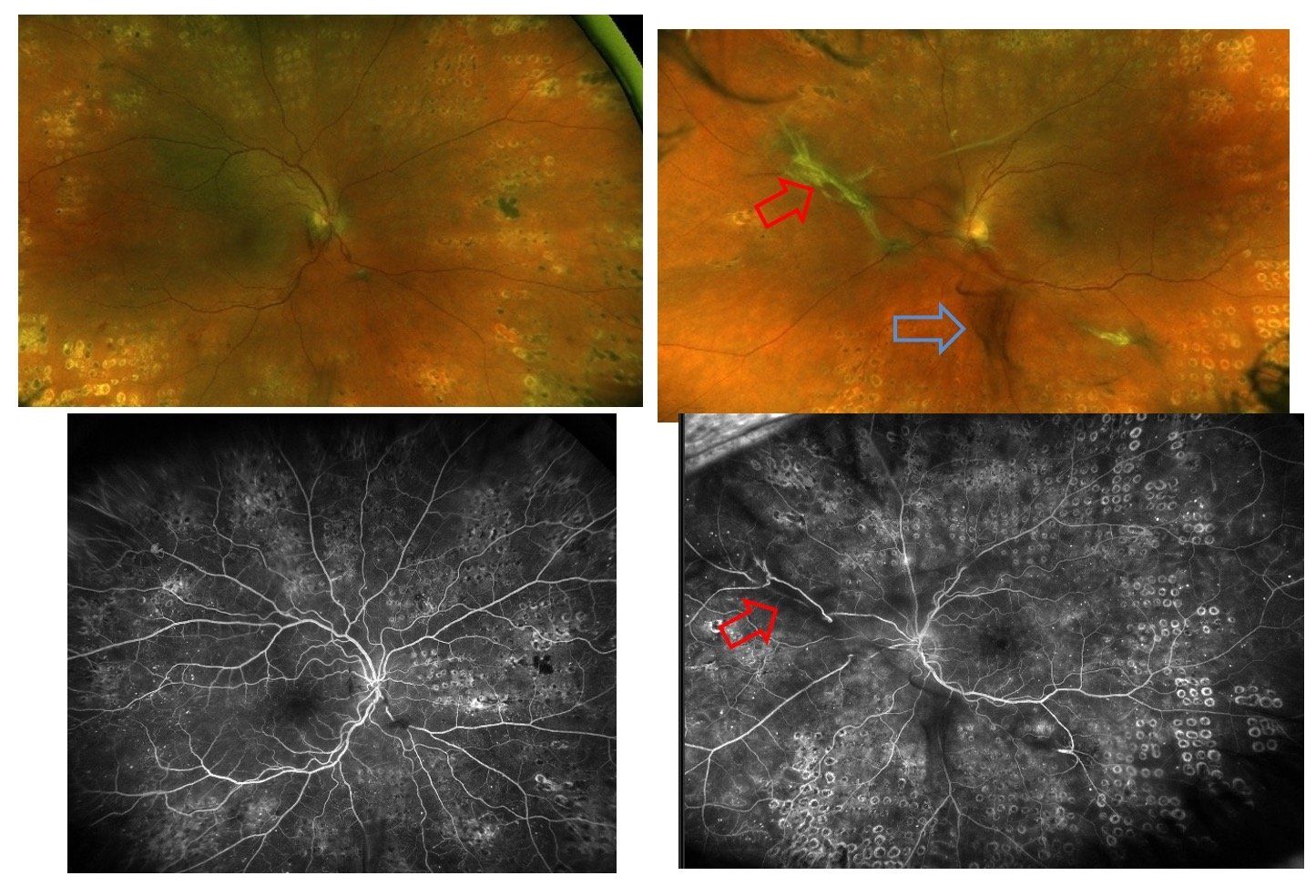
Figure 3. Fundus exam and fluorescein angiography OD. Panretinal photocoagulation spots are notable with no active neovascularization. OS fibrotic membrane with no leakage noted (red arrow) residual vitreous hemorrhage (blue arrow) with no active neovascularization.
When new patients or noncompliant established patients present with sudden vision loss, they comment, “I wasn’t having any problems until…” or “I was doing well until…”
This perception of “seeing well” creates circumstances for potential vision loss.
Case report
A 40-year-old white female is referred to rule out retinal detachment OS. She indicates “blurred vision” OS for about 2 to 3 weeks. She has been diagnosed with type 2 diabetes for a little over one year. She indicates good control and takes metformin 1000 mg daily as well as Ultra Comfort Insulin Syringe as directed; however, she is not sure of her blood sugar level or hemoglobin A1C. She also suffers from obesity.
Related: Time in range as an alternative to HbA1c
Her examination was remarkable for visual acuity (VA) OD 20/20, OS 20/400. Intraocular pressures (IOP) were 16 mm Hg OD/OS.
Anterior segment examination was unremarkable.
Fundus examination was remarkable for exudates in the macula and posterior pole. Multiple scattered microaneurysms (MA) and intraretinal hemorrhages (IRH). Retinal neovascularization was noted superotemporally. OS exhibited diffuse subhyaloid vitreous hemorrhage, a large mobile preretinal hemorrhage inferiorly, and fibrovascular proliferation into the vitreous cavity nasally. Although the view was limited, there was no evidence of rhegmatogenous retinal detachment (RRD). These findings are evident in the fundus photographs. (Figure 1)
More by Dr. Rafieetary: Toxoplasmosis retinochoroiditis pictorial review
Optical coherence tomography (OCT) OD (Figure 2) demonstrated exudates but no significant central macular edema or significant thickening. OS did not exhibit sufficient view for imaging.
Diagnosis of proliferative diabetic retinopathy OU and vitreous hemorrhage OS was established. The patient was treated with an intravitreous bevacizumab (Avastin, Genentech; IVA) OS on the same day and was scheduled for panretinal photocoagulation (PRP) OD one week later. She received a second IVA OS one month later, and after the resolution of vitreous hemorrhage underwent PRP OS as well.
Approximately one year from her initial visit fundus examination and fluorescein angiography show no active retinal neovascularization. (Figure 3) Patient continues with proper follow-up care and has been stable for nearly two years.
Related: Retina presentation looks familiar
Discussion
Although the presence and degree of diabetic retinopathy increases with duration of the disease itself, many type 2 diabetics have delayed diagnosis. ODs should diligently evaluate all patients with diabetes, regardless of the onset of the disease, for presence of diabetic retinopathy.
In addition, all patients with diabetes should be educated about the potential ocular complications of diabetes and be warned that although they should report any sudden onset vision loss to their eyecare providers, they should not assume stability of the eye based on their perception of “normal, stable” vision.
Diabetic retinopathy remains a major cause of vision loss and blindness. With timely and proper intervention, eyecare practitioners can avert debilitating results.
On the side note, lack of visualization of the retina during fundus examination is not always indicative of RRD. The proper diagnosis in this case is vitreous or media opacity until RD can be ruled out by further examination or ancillary testing such as B-scan.
More by Dr. Rafieetary: Case report: Don’t be misled by diabetic retinopathy
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.