Preoperative considerations in patients with cataracts and pseudoexfoliation syndrome
Preoperative evaluation of patients with pseudoexfoliation (PXF) syndrome is essential in preparing for and potentially preventing complications during phacoemulsification. Patients with PXF have been documented to have an accelerated rate of cataracts, both nuclear and subcapsular.
Preoperative evaluation of patients with pseudoexfoliation (PXF) syndrome is essential in preparing for and potentially preventing complications during phacoemulsification. Patients with PXF have been documented to have an accelerated rate of cataracts, both nuclear and subcapsular.1,2 These patients may face a greater chance of complications such as increased inflammation, intraocular pressure spikes, and lens related complications, both during and following cataract surgery. In fact, it has been listed as the most common cause of complications associated with cataract surgery.2
Foreseeing potential difficulties is important not only to prepare the surgeon, but to have the preoperative discussion with the patient-the initial decision for cataract excision will entail a more detailed analysis of risks, benefits, and alternatives. This review provides a systematic approach to comprehensively assess eyes with PXF, covering all aspects of the ocular examination, and appropriate surgical considerations.
PXF presentation
In general, corneal findings in PXF are rare, but careful evaluation of the corneal endothelium may reveal flakes of bright white fibrillar exfoliative material attached to the corneal endothelium.3,4 These deposits often appear as irregularly spaced aggregates reminiscent of small filaments. The flakes can vary in shape and size, and may differ over time.
Another posterior corneal finding is a reduction in the number of endothelial cells, sometimes with an accompanying increase in central corneal thickness.3 Specular microscopy has demonstrated a measureable decrease in the number of endothelial cells, as well as cell polymorphism.4 Clinically, these cell changes may appear as a light paracentral area of pigmentation on the corneal endothelium, occasionally organized in the pattern of a Krukenberg spindle.3 A decrease in integrity of the corneal endothelial cells may lead to increased corneal inflammation postoperatively, with signs such as endothelial folds, microcystic edema, and pseudophakic bullous keratopathy.1 Fortunately, these keratopathies are often treated without additional surgical intervention and respond to topical corticosteroids.1,5
Evaluation of the anterior chamber should include careful assessment of chamber depth for 360 degrees, also comparing between both eyes. Though there are many direct signs of lens dislocation (discussed below), one indirect sign is an alteration in chamber depth. A lens can subluxate forward, leading to a shallow anterior chamber, or may fall backward towards the vitreous, resulting in a hyper-deep chamber.1 Asymmetry may be more evident on gonioscopy, hence its increased importance in pseudoexfoliative preoperative assessment.1
Pseudoexfoliation is classically associated with pigment loss both at the pupillary margin, or ruff, and around the iris sphincter. On iris transillumination, the margin may have a moth-eaten appearance.4 Gray-white flakes may be present at the pupillary margin1,4 (Figure 1).
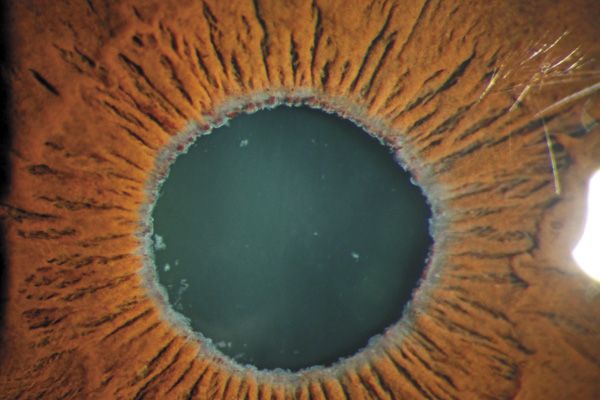
It has been proposed that deposition of this material, possible hypoxia, and iris atrophy may contribute to iris functional changes. As the iris sphincter may be compromised, there may be a reduced response of the eye to mydriatics, both in-office and intraoperatively.1,4 This may hamper the preoperative dilated fundus examination, and intraoperatively may require adjunctive pupil-enlarging surgical devices.1 Posterior synechiae have also been documented in the setting of PXF, which can also contribute to reduced pharmacologic dilation.1 Iris flutter, or iridodonesis, is another indirect sign of weak zonules, which hold the lens in place.1 Sometimes the iris may be more rigid in PXF, so iridodonesis may not be evident.4
Iris changes in PXF closely intertwine with lenticular findings. Exfoliative material most often is present on the anterior capsule of the lens (Figure 2).
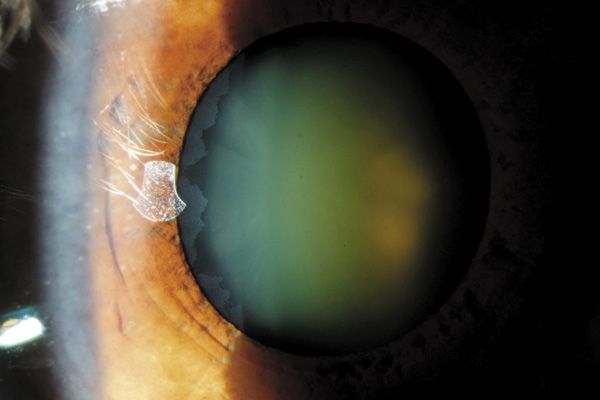
The anterior capsule of PXF may appear to have a target, or bull’s eye pattern, which can consist of three zones after dilation: the central clear disk, approximately the diameter of the pupil; the clear zone corresponding to cleaning via pupil size fluctuations; and a peripheral band of fibrillar material.3,4 A direct sign of zonular damage is phacodonesis, or flutter of the lens.1,4 Although crude, jolting the slit lamp table during examination of the lens can produce a subtle vibration or movement of the lens which may indicate zonular weakness. A grading scale from +1 to +4 exists, which may aid in considering alternative surgical methods in extracting a looser lens.6 A loose or subluxated lens is best viewed after dilation, though in poorly dilating eyes, examining for a decentered fetal nucleus may be helpful.1
Glaucoma and cataract
Patients diagnosed with PXF must be carefully preoperatively evaluated for pseudoexfoliative glaucoma (PXG); it has been found that they are twice as likely to convert from ocular hypertension to glaucoma.2 It is suspected that deposits of fibrillar material and pigment in the trabecullar meshwork and Schlemm’s canal may be the main reason for elevated intraocular pressure (IOP) in PXF.4 Additional tests if suspecting glaucoma include but are not limited to: optic nerve imaging, visual field testing, and if not previously done, pachymetry and gonioscopy. Treating these patients prior to phacoemulsification may require topical medications and/or lasers.5 Patients with concurrent cataracts and glaucoma, pseudoexfoliative or otherwise, must have the glaucoma stabilized prior to considering phacoemulsification as post-operative pressure spikes are much more common in such instances.1 Occasionally, the best strategy may be a combined cataract-glaucoma procedure when IOP control is difficult preoperatively or there is advanced optic nerve damage.5
PXF is a significant risk factor for patients undergoing cataract surgery. Weakness of the zonular apparatus, reduced pupillary dilation, and corneal changes may necessitate altered surgical techniques and adjunctive devices. Recognition and preparation is instrumental; the surgeon may need alternative intraocular lenses, adjunctive devices to expand the pupil or stabilize the capsular bag, and other ophthalmic specialties on standby to the operating room. Candid conversation with PXF patients on the risks, benefits and alternatives is important-optometrists are often the first point of conversation for discussing cataract surgery. Recognition of pseudoexfoliation may better prepare the practitioner for postoperative care; additional medications and more frequent follow-up may be required.ODT
Special thanks for insights and photographs: Richard Braunstein, MD, Amilia Schrier, MD, Sarah Harmon, Martha Moszczynski.
References
1. Shingleton BJ, Crandall AS, Ahmed II. Pseudoexfoliation and the cataract surgeon: preoperative, intraoperative, and postoperative issues related to intraocular pressure, cataract, and intraocular lenses. J Cataract Refract Surg. 2009 Jun;35(6):1101-20.
2. Fingeret M. Exfoliation glaucoma. PowerPoint Presentation. Optometric Glaucoma Society Residency Education Meeting. Fort Worth. 8/5/13.
3. Crista AR. Pseudoexfoliation syndrome and cataract surgery in pseudoexfoliation syndrome. Timisoara Med J. 2009;59(3-4):378-380. http://www.tmj.ro/article.php?art=237564682127339. Accessed July 16, 2013.
4. Drolsum L, Amund R, Nicolaissen B. Cataract and glaucoma surgery in pseudoexfoliation syndrome: a review. Acta Ophthalmologica Scandinavica. 85.8 (2007): 810-21.
5. Ahmed IK. The Art of managing PXF glaucoma. Rev Ophthalmol. http://www.revophth.com/content/d/cataract/c/33327/. Accessed July 16, 2013.
6. Calafati J, Tam DY, Ahmed IK. Pseudoexfoliation syndrome in cataract surgery. EyeNet. 2009 April;13(4): 37-39.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.