Prepping the ocular surface before surgery
With patients undergoing cataract or refractive surgery, optometrists ensure a stable ocular surface before the surgeon performs preoperative calculations.

The ocular surface is the first refracting surface of the eye; therefore, the tear film provides the basis for good vision. An unhealthy tear film can cause an almost 1.00 D fluctuation in visual acuity.1,2
In the case of patients undergoing cataract or refractive surgery, optometrists ensure a stable ocular surface before the surgeon performs preoperative calculations. In my practice, I evaluate patients using a tear break-up test and vital dye staining of the cornea and conjunctiva, and then if necessary, schedule them back for a presurgical dry eye disease (DED) examination.
My full DED evaluation includes meibomian gland evaluation using the Korb gland evaluator as well as LipiView II Ocular Surface Interferometer with Dynamic Meibomian Imaging (DMI; Johnson & Johnson Vision), which measures lipid layer thickness, captures blink dynamics, and images the meibomian gland structure). I also conduct osmolarity reading with TearLab Osmolarity System (TearLab Corp.), look for MMP-9 inflammatory marker with InflammaDry (Quidel), and stain the cornea and conjunctiva using both fluorescein and lissamine green vital dyes.

Once I determine the cause of the physiologic imbalance, I can initiate treatment before the patient sees the surgeon. Restoring tear film homeostasis in DED patients leads to improved surgical outcomes.3,4
Previously from Dr. O'Dell: Why meibography can be a game-changer in treating dry eye
Patient education helps
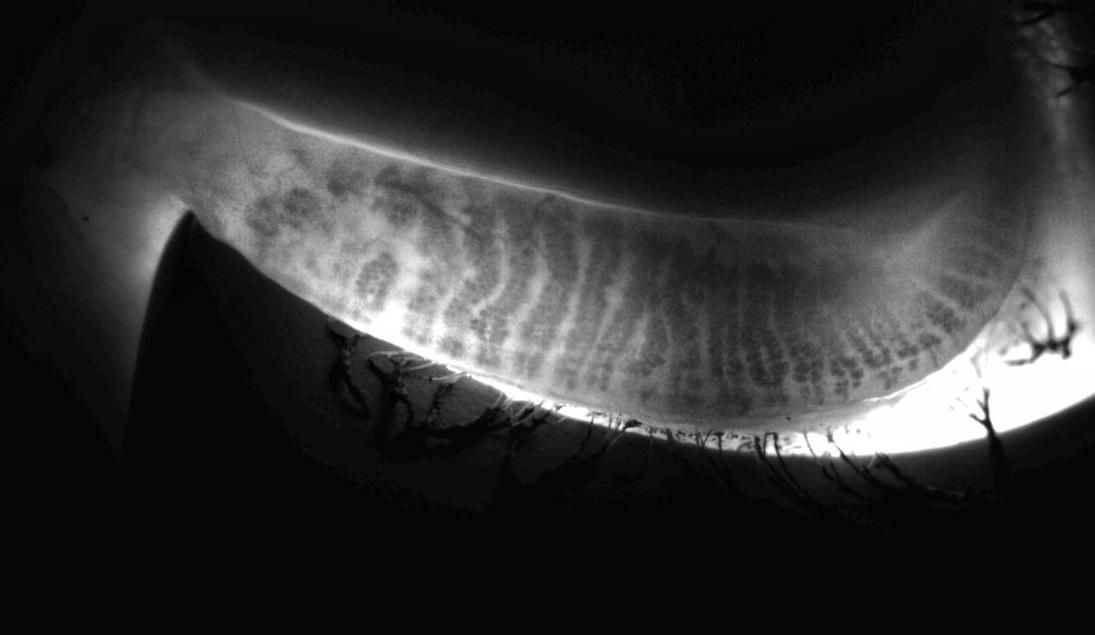
Education is paramount for patients to commit to their DED treatment plan. Asymptomatic individuals who develop postoperative ocular surface disease (OSD) concerns are prone to unfairly blame the surgeon for their discomfort. With meibography, for example, I can show patients what their glands look like (and what healthy ones should look like), which helps them understand why they need treatment and makes them more receptive to the required follow-up regimen.
For patients who are symptomatic, education provides more evidence on why we need to be aggressive in their treatment. They already understand they have a condition, and I explain that surgery will increase their inflammatory response and possibly worsen their symptoms.

Figure 1A (Top) and 1B (Bottom). A 51-year-old Caucasian female presented with reduced vision due to progressive cataract. Presurgical ocular wellness exam included dry eye testing with dry eye questionnaire, LipiView II imaging, meibography, lipid layer thickness and blink analysis, InflammaDry, and an ocular surface evaluation using vital dyes. She was found to have dry eye disease, predominantly evaporative, due to obstructive meiboniman gland dysfunction with mild inflammation and mild hyperosmolartiy. Prior to surgery, she elected treatment with LipiFlow thermal pulsation in addition to lifetegrast (Xiidra).
By aggressively treating OSD in presurgical patients, I build better relationships with my referring surgeons. Although rare, the most feared complication of surgery is
endophthalmitis.5-7 For patients with signs of blepharitis, I perform BlephEx (RySurg) to exfoliate the lids and remove the bacterial load. I also recommend a lid hygiene regimen and a lid wipe containing hypochlorous acid, further ensuring optimal outcomes.
Treating conditions
I direct my therapy based on what I learned in the DED evaluation and the patient’s load of inflammation.
Pre-surgically, Xiidra (lifitegrast, Shire) is my choice of prescription medication because patients have improvement in as little as two weeks. I favor FreshKote drops (Focus Laboratories) as an over-the-counter eye drop which patients can conveniently purchase in the practice. For those with meibomian gland dysfunction, I will perform LipiFlow (Johnson & Johnson Vision) thermal pulsation to help clear obstruction prior to surgery.
For patients with allergies, inferior corneal staining due to exposure, and low levels of inflammation, I like to use absorbable punctum plugs, such as Comfortear Lacrisolve 180 (Paragon BioTeck). They are ideal for use around surgery and are widely underutilized. Alternatively, I may employ the manufacturer’s long-term Comfortear Punctum Plugs; they are easy to insert and fit most punctum sizes.
It is easy to get overwhelmed by the vast array of OSD treatments, so it is important to take a stepwise approach. For presurgical patients, decide what needs immediate attention and what can wait, based on the testing. Treat the highest need first.
As mentioned earlier, the most important aspect to achieving success with this comprehensive strategy is education. By explaining a patient’s condition and informing them of how it is treated, you help them understand the importance of the therapy you prescribe.

ODs taking charge
The need for comprehensive, full-scope optometric care is clear. Many aspects of patient care could benefit from better relationships between primary-care providers and optometrists. To help bridge this gap, ODs should consider working directly with primary-care providers. Family physicians often refer directly to ophthalmologists, bypassing optometrists. We need to educate primary-care doctors about to our role in caring for patients.
When optometrists take charge of the care, we create solid partnerships with our patients. I know my patients will continue their care with me following referral to my fellow ophthalmologists because of the time and effort I spend educating them up front prior to the referral.
Related: Ocular surface disease limits surgical options
It has been well discussed that the eye care industry is facing an increase in the number of patients needing surgical care. At the same time, the number of U.S. ophthalmologists isn’t expected to increase, and they are retiring faster than they are being trained.8 I talk to patients about local surgeons who are performing micro-invasive glaucoma surgery (MIGS), small-lenticule extraction, dropless procedures, laser cataract surgery, or about those who are using the latest intraocular lens (IOL) technology.
Because I take charge and help my patients choose a surgeon, I build trust by sharing my expertise. Perhaps ODs do not always consider taking charge in that way, but we can. I attend MD meetings, get to know the doctors, and forge relationships. I find out if they are responsive and how they communicate (Can I text or call them? Do they read my letters?), and I learn what works.
Looking ahead
Optometrists are poised to leverage our key role in patients’ overall eye health. By employing all tools and treatments available and enhancing our relationships with surgeons and primary-care providers, we will ensure the highest standard of care for our patients.
References
1. Tutt R, Bradley A, Begley C, Thibos LN. Optical and visual impact of tear break-up in human eyes. Invest Ophthalmol Vis Sci. 2000 Dec;41(13):4117-23.
2. Epitropoulos AT, Matossian C, Berdy GJ, Malhotra RP, Potvin R. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J Cataract Refract Surg. 2015 Aug;41(8):1672-7.
3. Donnenfeld ED, Solomon R, Roberts CW, Wittpenn JR, McDonald MB, Perry HD. Cyclosporine 0.05% to improve visual outcomes after multifocal intraocular lens implantation. J Cataract Refract Surg. 2010 Jul;36(7):1095-100.
4. Albietz JM, Lenton LM. Management of the ocular surface and tear film before, during, and after laser in situ keratomileusis. J Refract Surg. 2004 Jan-Feb;20(1):62-71.
5. Endophthalmitis Vitrectomy Study Group. Microbiologic factors and visual outcome in the endophthalmitis vitrectomy study. Am J Ophthalmol. 1996 Dec;122(6):830-46.
6. Taban M, Behrens A, Newcomb RL, Nobe MY, Saedi G, Sweet PM, McDonnell PJ. Acute endophthalmitis following cataract surgery: a systematic review of the literature. Arch Ophthalmol. 2005 May;123(5):613-20.
7. West ES, Behrens A, McDonnell PJ, Tielsch JM, Schein OD. The incidence of endophthalmitis after cataract surgery among the U.S. Medicare population increased between 1994 and 2001. Ophthalmology. 2005 Aug;112(8):1388-94.
8. Bethke W. What’s the future of private practice? Rev Ophthalmology. Available at: https://www.reviewofophthalmology.com/article/whats-the-future-of-private-practice. Accessed 3/27/18.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.