Review Chiari-related diseases and associated ocular symptoms
There is a role for optometrists in diagnosis and treatment of these conditions
Table 1
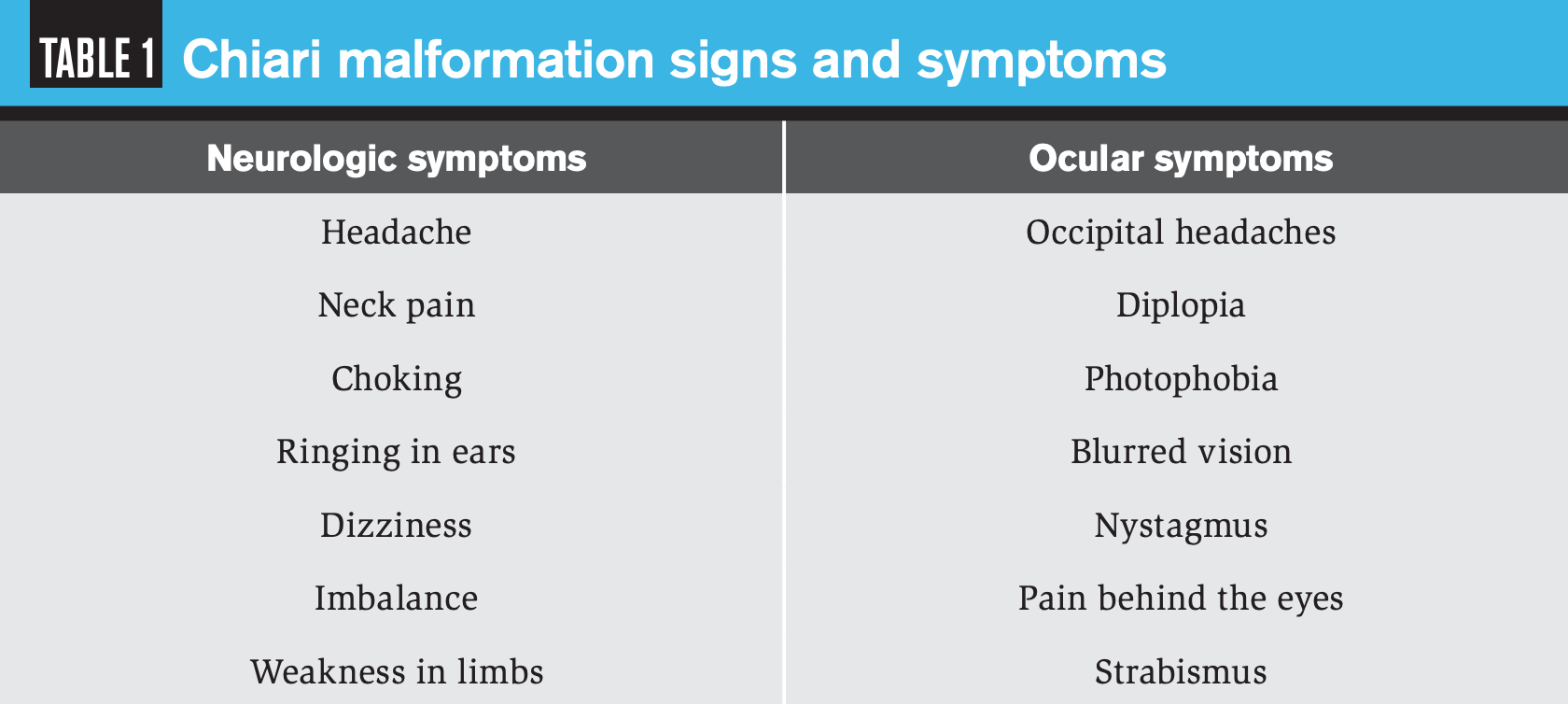

Chiari malformations (CMs) can cause a variety of ocular symptoms, which optometrists should be aware of in order to provide correct diagnosis and timely referral to a neurologist.
A Chiari malformation (CM), named after Austrian pathologist Hans Chiari in 1891, is a structural defect in the inferior area of the brain (both the cerebellum and brain stem). These malformations have also been referenced as a congenital tonsillar herniation, tonsillar ectopia, or tonsillar descent. Due to human anatomy and much of the visual system being occupied in this area of the brain, these malformations can present with many ocular manifestations. This article will review CMs and related disorders and discuss the ocular symptoms, diagnosis, and treatment options for these disorders.
A CM occurs when a portion of the cerebellum (part of the brain responsible for controlling balance), most predominantly the cerebellar tonsils, is situated under the funnel-shaped opening of the skull (the foramen magnum) to the spinal cord.1 It is more prevalent in females and occurs mostly during fetal development. Those who develop CM later in life do so because of a lesion in the brain, causing excessive drainage of cerebrospinal fluid (CSF), as a result of injury, toxic substances, or infection.2
Types of CM
CM is categorized as Types I to IV. These types are assigned based on the anatomy of the brain tissue pushed into the spinal cord and whether developmental abnormalities of the brain or spine exist. It is important to understand that the numbering of the types of CM is not due to severity but rather represents distinct anatomical anomalies of the brain. Types III and IV are rare and not reviewed in this article. Another related disease that will be addressed along with the ocular manifestations is syringomyelia.3
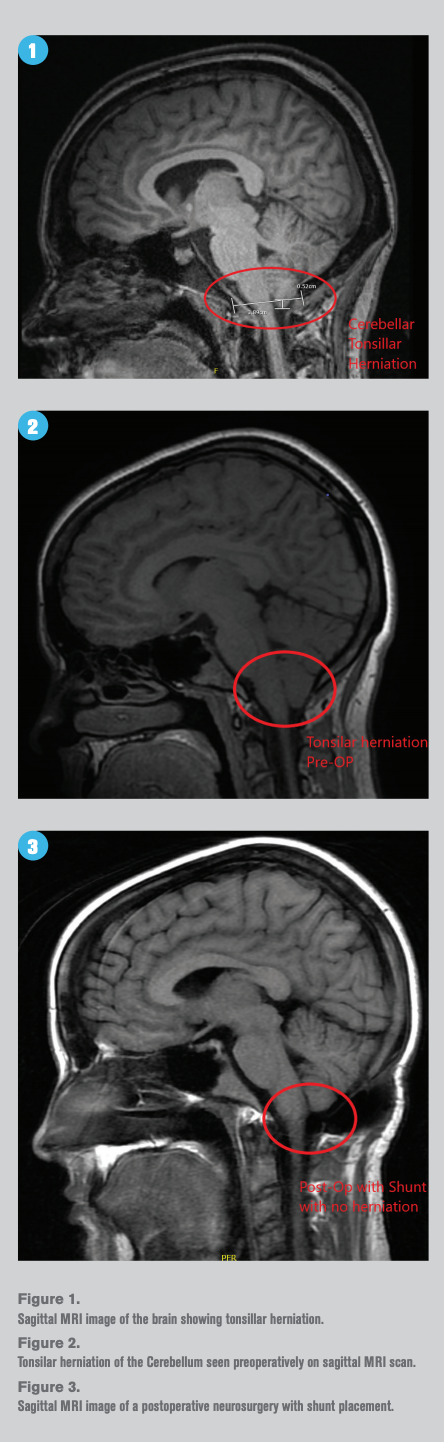
A type I CM (CM I) is characterized by the cerebellar tonsillar descent into the foramen magnum with resulting impairment of CSF and/or brainstem composition (Figure 1). It most commonly occurs in children (40 percent under age 5 years, 25 percent age 5 to 10 years, and 30 percent age 10 to 15 years).4 The most common symptom is pain, usually occipital or upper cervical headache exacerbated by Valsalva (straining, coughing, and sneezing). Other symptoms vary greatly and may include motor and sensory changes in the extremities, clumsiness, and dysphasia (Table 1). Also, syringomyelia may coexist in many patients and be associated with progressive scoliosis.
Diagnosis is made with magnetic resonance imaging (MRI) and is the gold standard diagnostic tool. Descent of the cerebellar tonsils through the foramen magnum up to 6 mm is normal in children 0 to 10 years old. In CM I, the tonsils are generally pointed rather than rounded. This type of CM is defined radiographically as a simple displacement of the cerebellar tonsils 5 mm or greater below the foramen magnum.5
Type II CM (CM II), sometimes referred to as an Arnold-Chiari malformation, is typically more severe than Type I, and generally the onset of symptoms occurs at a younger age. The herniation of the vermis, medulla, and fourth ventricle of the cerebellum extends into the spinal cord. Nearly 100 percent of these patients also have myelomeningocele (spina bifida). Myelomeningocele is an anomaly where a portion of the spinal cord is exposed through the child’s back, forming a sac filled with cerebrospinal fluid (CSF), meninges, and spinal cord nerves. This can be associated with paralysis and possible lack of bladder and bowel control. These patients almost always require surgical intervention during infancy or early childhood.6
The symptoms of CM II are similar to CM I, along with additional findings such as hydrocephalus. Hydrocephalus is a condition in which excessive CSF accumulates in the brain ventricles, which leads to pressure on the tissues of the brain. This can lead to an enlarged head (macrocephaly), vomiting, seizures, and developmental delays.
Syringomyelia occurs when a cavity, or a syrinx, is formed inside of the spinal cord. The syrinx is caused by a buildup of fluid or cyst and is a chronic condition that can expand over time. It is often associated with CM but can also be caused by spinal trauma, a tumor, or other causes. The symptoms associated with this diagnosis depend on the size and specific location, and include numbness, tingling, loss of muscle mass, muscle weakness, decreased sensation to hot and cold, abnormal curvature of the spine (scoliosis), chronic pain, and spasms and tightening of the muscles in the legs (spasticity).
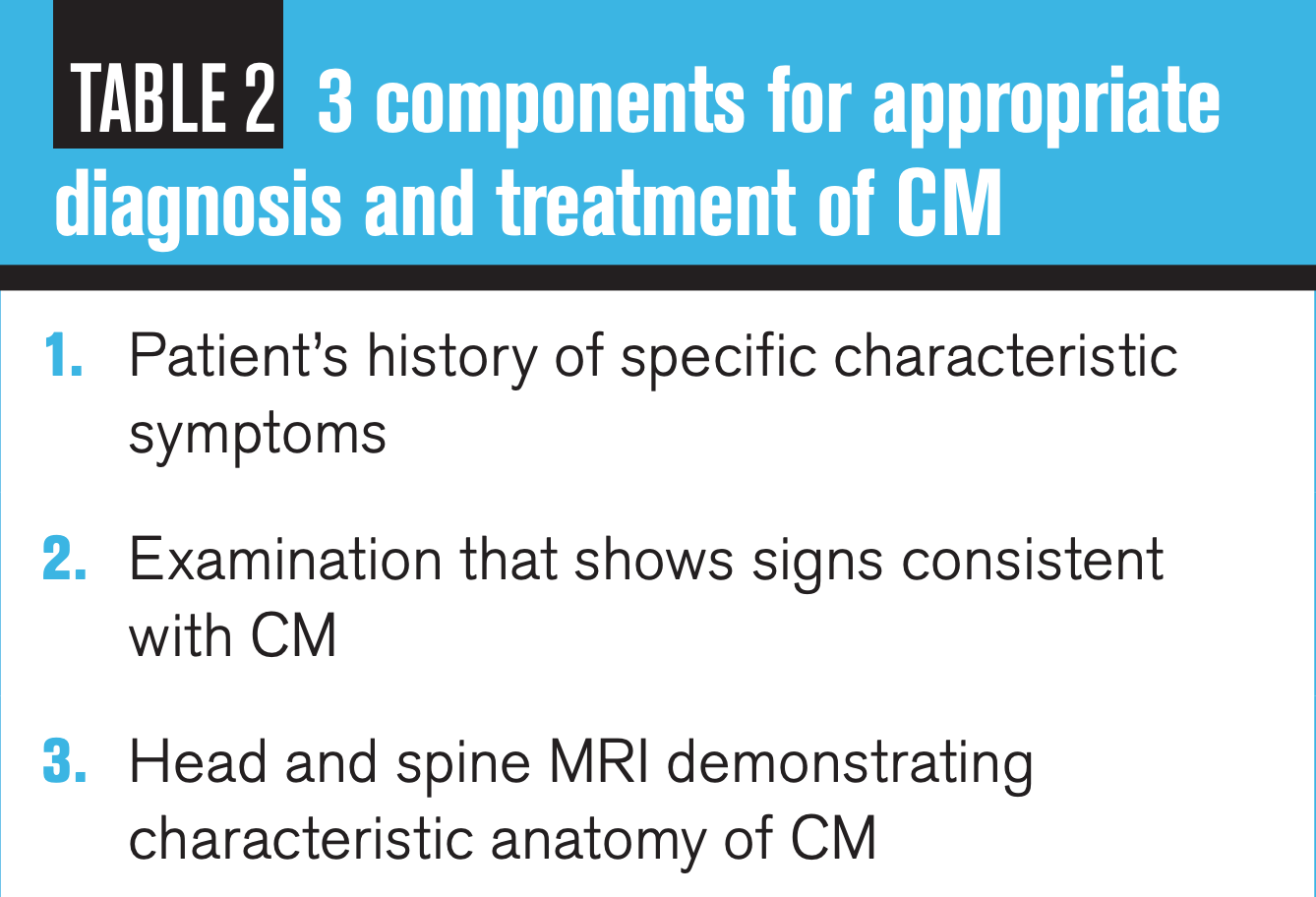
Three important components make a diagnosis of CM versus syringomyelia. First is a complete patient history and list of symptoms; second is the clinical exam and signs consistent with syringomyelia; and finally an MRI scan of the brain and spine (Table 2). Having both sets of neuroimaging helps to determine the cause of the syrinx.7
Figures 1, 2 and 3
Imaging
Neuroimaging techniques that are beneficial include MRI, cine MRI, plain X-rays, and computed tomography (CT) scans. MRI uses a magnetic field and radio waves to produce cross-sectional images of tissues in the body. The best visualization of the MRI and cine MRI is a sagittal cross-sectional cut (Figure 1). A cine MRI is like a traditional MRI, but it can be used in real time to measure and assess CSF flow abnormalities. A plain X-ray can point to malformations in the skull and defects in the cervical vertebrae, and a CT scan may also be useful in clarifying congenital bony abnormalities at the skull base.
Treatment
The current treatment options for CM depend on the severity of the symptoms experienced. Other factors include disease progression, impact of symptoms on overall quality of life, an individual’s age, and general health.
For mild symptoms such as pain and headache, in many cases medication and lifestyle alterations such as avoiding weightlifting may be initiated.
For more severe CM symptoms, neurosurgery may be the only answer. Most commonly, the procedure performed is a posterior fossa decompression. This surgery is usually performed in older children and adults to create more space for the cerebellum and reduce pressure on the spinal column. Another procedure commonly used is a spinal laminectomy to remove part of the bony roof of the spinal canal, increasing its size and reducing pressure on the spinal column. CM patients with hydrocephalus are most commonly treated with implantation of a tube (shunt) to drain excessive CSF away from the skull and brain.8,9 Figures 2 and 3 show a CM before and after a neurosurgery procedure, respectively.
Table 2
Ocular manifestations
Due to the anatomical structures of the brain and location of occipital lobes (which contain the visual cortex), CMs will many times have other ocular manifestations. As previously mentioned, pain and occipital headaches are the most common symptoms associated with CM. CM I research indicates that visual symptoms are present in up to 80 percent of patients.10
These ocular symptoms include retro-orbital pain, blurred vision, photophobia, diplopia, nystagmus, and strabismus. Nystagmus is the most common eye movement deficit in CM patients due to the location of the ocular motor vermis (located in the cerebellum), which is responsible for the accuracy of rapid saccadic eye movements.11,12
In CM II with hydrocephalus and increased CSF, there is also a risk of increased intracranial pressure, which can lead to papilledema. Thus, a thorough patient case history, comprehensive dilated eye exam, and special testing such as ocular coherence tomography (OCT) and visual field are very important for any patient suspected of having a CM.
Conclusions
CMs and associated diseases have a large range of symptoms, many of which are ocular in nature. Thus, it is vital for the primary eyecare provider to understand that a patient complaining of these symptoms may be at risk of having some form of CM, especially in younger patients.
A CM diagnosis is serious and can be life threatening. If CM is suspected, a timely referral to a neurologist is important. A comprehensive case history, neurological clinical exam, and neuroimaging are the gold standard needed to confirm a diagnosis of CM and related diseases.
Once a definitive diagnosis is made, it is imperative to have full clinical team of neurologist, neurosurgeon, neuro-ophthalmologist and optometrist to address all the patient’s needs. Optometrists have the skill set to diagnose, treat, and manage ocular manifestations associated with CMs now and into the future.
References
1. Hernández AA, Guerrero AI, Martínez MI, Vázquez ME, Fernández JB, Chesa i Octavio E, Labrado Jde L, Silva ME, de Araoz MF, García-Ramos R, Ribes MG, Gómez C, Valdivia JI, Valbuena RN, Ramón JR. Malformations of the craniocervical junction (Chiari type I and syringomyelia: classification, diagnosis and treatment). BMC Musculoskelet Disord. 2009 Dec 17;10 Suppl 1(Suppl 1):S1.
2. Mampalam TJ, Andrews BT, Gelb D, Ferriero D, Pitts LH. Presentation of type I Chiari malformation after head trauma. Neurosurgery. 1988 Dec;23(6):760-762.
3. Levy WJ, Mason L, Hahn JF. Chiari malformation presenting in adults: a surgical experience in 127 cases. Neurosurgery. 1983 Apr;12(4):377-90.
4. Iskandar BJ, Oakes WJ. Chiari Malformations, in Principles and Practice of Pediatric Neurosurgery, ed 1st. Albright AL, Pollack IF, Adelson PD (eds). New York, NY: Thieme Medical Publishers, 1999.
5. Milhorat TH, Nishikawa M, Kula RW, Dlugacz YD. Mechanisms of cerebellar tonsil herniation in patients with Chiari malformations as a guide to clinical management. Acta Neurochir (Wien). 2010 Jul;152(7):1117-27.
6. Stevenson KL. Chiari type II malformation: past, present and future. Neurosurg Focus. 2004 Feb;16(2):E5.
7. Aghakhani N, Parker F, David P, David P, Morar S, Lacroix C, Benoudiba F, Tadie M. Long-term follow-up of Chiari-related syringomyelia in adults: analysis of 157 surgically treated cases. Neurosurgery. 2009 Feb;64(2):308-5.
8. Mutchnick IS, Janjua RM, Moeller K, Moriarty TM. Decompression of Chiari malformation with and without duraplasty: morbidity versus recurrence. J Neurosurg Pediatr. 2010 May;5(5):474-8.
9. Attenello FJ, McGirt MJ, Gathinji M, Datoo G, Atiba A, Weingart J, Carson B, Jallo GI. Outcome of Chiari-associated syringomyelia after hindbrain decompression in children: analysis of 49 consecutive cases. Neurosurgery. 2008 Jun;62(6):1307-13.
10. Milhorat TH, Chou MW, Trinidad EM, Kula RW, Mandell M, Wolpert C, Speer MC. Chiari I malformation redefined: clinical and radiographic findings for 364 symptomatic patients. Neurosurgery. 1999 May;44(5):1005-17.
11. Takagi M, Zee DS, Tamargo RJ. Effects of lesions of the oculomotor vermis on eye movements in primate: saccades. J Neurophysiol. 1998 Oct;80(4):1911-31. 12. Shaikh AG, Ghasia FF. Neuro-ophthalmology of type 1 Chiari malformation. Expert Rev Ophthalmol. 2015;10(4):351-357.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.