Study: comparison of glisenings, PCO in hydrophobic acrylic IOLs
Investigators evaluated and compared the long-term formation of posterior capsular opacification (PCO) and the rate of glistenings that developed between 2 hydrophobic acrylic intraocular lenses (IOLs).
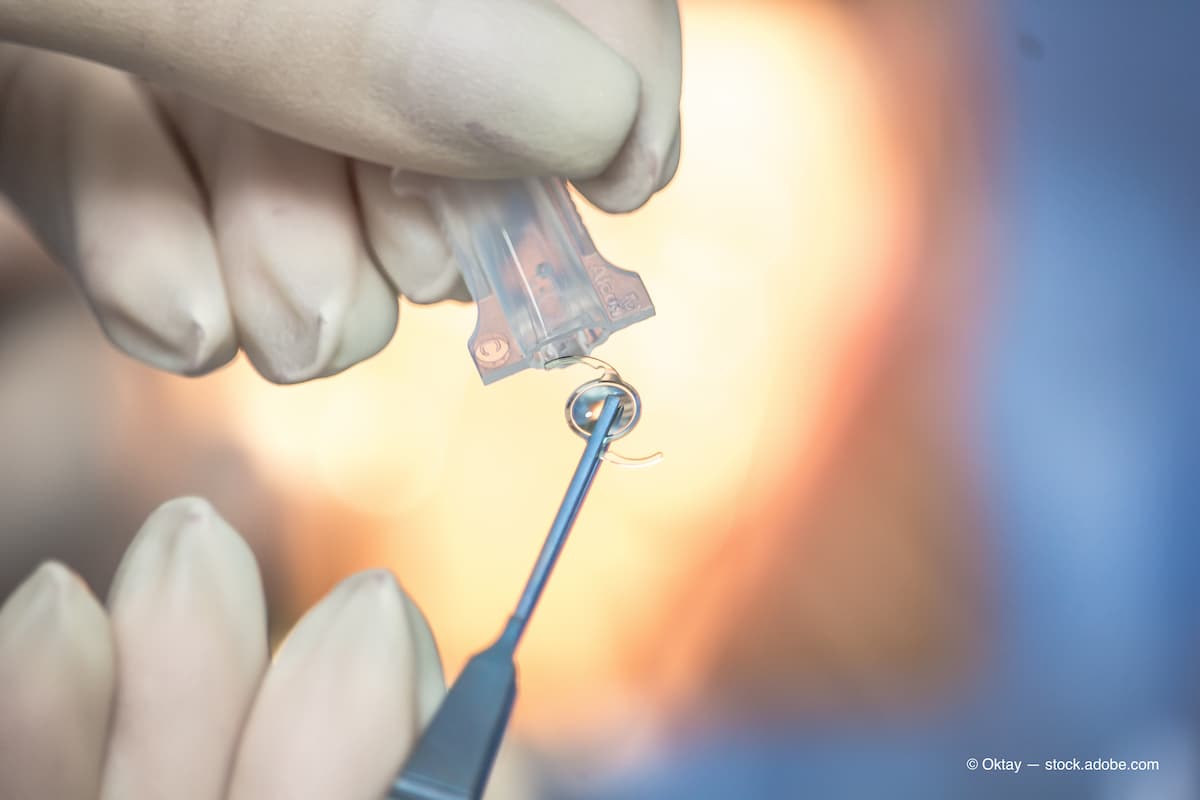
A comparison of 2 hydrophobic acrylic intraocular lenses (IOLs) evaluated the long-term formation of posterior capsular opacification (PCO) and the rate of glistenings that developed. The investigators found that the Hoya Vivinex had significantly lower development of glistenings compared with the Alcon AcrySof lens,1 according to Gerd Auffarth, MD, and colleagues. He is from the University of Heidelberg, Heidelberg, Germany.
The investigators conducted a prospective, multicentric, randomized, paired-eye, open-label study that included 87 subjects who underwent cataract surgery with IOL implantation; of these, 67 patients completing the 3-year follow-up examination.
The completer population consisted of 32 subjects implanted with the Hoya IOL and 35 implanted with the Alcon IOL. The primary endpoints were an evaluation of glistenings and measurement of PCO. The secondary outcomes were measurement of the best-corrected distance visual acuity (VA), contrast acuity, uncorrected VAs, subjective refraction, medical and lens complication rates, adverse events, and optical/visual symptoms.
The patients were followed at 6-months and 1, 2 and 3 years postoperatively. At the 3-year follow-up, the mean PCO scores were 0.121 ± 0.193 for eyes implanted with the Hoya IOL versus 0.239 ± 0.463 for those with the Alcon IOL, a difference that reached significance (p = 0.026). The Hoya IOL had a significantly lower rate of glistening occurrence throughout the 3 years postoperatively (0.14 ± 0.26) compared to the Alcon IOL (1.79 ± 1.43; p < 0.0001).
The postoperative VAs improved from baseline with both IOL (p < 0.0001) and remained stable through the 3-year follow-up period. The eyes that received the Hoya IOL had a significantly lower occurrence of glistening at 3 years compared with the Alcon IOL (p < 0.0001). The incidence rates of PCO were very low and comparable with both IOLs.
Reference
Auffarth GU, Brézin A, Lignereux F, et al. Randomized multicenter trial to assess posterior capsule opacification and glistenings in two hydrophobic acrylic intraocular lenses. Sci Rep. 2023;13:2822; https://doi.org/10.1038/s41598-023-29855-8
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.