Study evaluates impact of exercise on intraocular pressure in glaucoma patients
Recent studies that have reported that active and healthy living can reduce IOP.
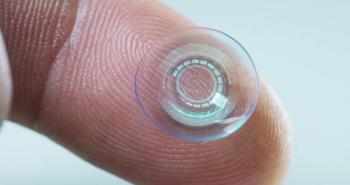
A new Spanish study found that exercise, especially aerobic exercise, may help modulate intraocular pressure (IOP) and may serve as a complementary therapy for patients with
Their rationale for delving into this topic is the recent studies that have reported that active and healthy living can reduce IOP. Many patients have consulted their doctors for lifestyle guidance based on this evidence.2
Further, they pointed out, “Physical activity is an important but often overlooked factor that affects glaucoma progression, according to recent research.3 However, the scientific community has yet to reach a consensus regarding the effects of exercise on glaucoma. Some theories suggest that an exercise-induced IOP elevation may lead to reduced ocular perfusion pressure, possibly causing mechanical or ischemic damage to the optic nerve head.4 In contrast, other studies proposed that exercise can trigger a reduction in IOP levels, thus positively affecting ocular health.5”
To increase the body of evidence regarding the impact of physical exercise on IOP, González-Devesa and colleagues conducted a literature search of English, Portuguese, or Spanish studies on the effect of exercise on IOP in glaucoma. They excluded case reports and yoga-based interventions. Of 1,001 identified records, 15 studies were independently evaluated. Of the 15 studies that were evaluated through the Mixed Methods Appraisal Tool scoring system, two quantitative randomized controlled studies scored 100% and 13 non-randomized studies averaged 84.62%, the investigators explained.
“Our findings indicated that both aerobic and resistance training led to an immediate IOP reduction post-exercise. In addition, exercise may serve as complementary therapy in glaucoma patients, potentially reducing glaucoma progression risk,” González-Devesa and colleagues reported.
Further, they offered the caveat that their findings were in large part obtained from single-session experiments and that the effects of longer-term exercise programs on IOP varied.
However, while they believe that their study underscores the potential benefit of exercise in IOP management, “the evidence remains inconclusive due to variations in study design, participant demographics, and exercise parameters. This lack of consistency in the research highlights the necessity for larger, standardized, and longer-term studies to robustly corroborate these preliminary findings,” they commented.
References:
González-Devesa D, Suárez-Iglesias D, Diz JC, et al. Systematic review on the impact of exercise on intraocular pressure in glaucoma patients. Int Ophthalmol. 2024;44:351;
https://doi.org/10.1007/s10792-024-03216-4 Hecht I, Achiron A, Man V, Burgansky-Eliash Z. Modifiable factors in the management of glaucoma: a systematic review of current evidence. Graefe Arch Clin Exp Ophthalmol. 2017;255:789–796.
https://doi.org/10.1007/s00417-016-3518-4 Olszewska H, Kosny J, Jurowski P, Jegier A (2020) Physical activity of patients with a primary open angle glaucoma. Int J Ophthalmol. 2020;13:1102–1108.
https://doi.org/10.18240/ijo.2020.07.14 McMonnies CW. Intraocular pressure and glaucoma: is physical exercise beneficial or a risk? J Optom. 2016;9:139–147.
https://doi.org/10.1016/j.optom.2015.12.001 Kumar H, Taneja S. Commentary: exercise and intraocular pressure: friends or foes? Indian J Ophthalmol. 2022;70:4236–4237.
https://doi.org/10.4103/ijo.IJO_2258_22
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.