Tapping technician’s expertise in averting claim denials

Exceptional patient care and valuable protected revenue can be achieved when we, as ophthalmic technicians, assist ophthalmologists by performing at our best. Taking patient histories, performing delegated ancillary testing, and scribing with the physician all proved opportunities to ensure that patients has a rewarding experience while we are with them in the office.
In addition to quality medical care, how can you help avoid claim denials, which are costly to the practice and confusing for the patient?
Claim denials are costly for any ophthalmology practice. It takes a team of committed individuals to help prevent these mistakes through a process of education, application, and communication. Technicians are critical members of the team who help bridge the gaps between the front and back office and between physicians and patients. This article addresses three pertinent questions about claim denials and the technicians’ role in how to avoid them.
Why do claim denials matter?
Ophthalmic practices are always seeking ways to increase efficiency. Every practice has processes in place to deal with claim denials, but how about a process that helps avoid the majority of these denials? Claim denials create inefficiencies by causing unnecessary work or rework.
By avoiding and preventing claim denials, technicians can dramatically increase the overall efficiency of the practice by decreasing the amount of work done on the back end with correcting and resubmitting claims.
Why should the technician want to be involved? Learning how to avoid claim denials supports ophthalmic technicians’ ultimate goal of caring for patients.
When a claim is denied, patients are often notified by their insurance, which creates unnecessary stress and worry for the patient, in addition to more work for them. Techs can help by recognizing common claim denial reasons and working to prevent them.
What are some typical denials?
There are many reasons why claims are denied. Some of the top reasons include insufficient documentation, inappropriate CPT or ICD-10 codes, missing or wrong modifiers, correct coding initiative (CCI) edits, prior authorization not obtained, and medical vs. vision. Following is an overview of common claim denials and how technicians can help patients steer clear of them.
Insufficient documentation
Sufficient and appropriate documentation is needed to help establish medical necessity for all billable services: exams, testing, minor and major surgeries, etc. As technicians, we can help ensure that all documentation is complete and appropriate by knowing the requirements.
How many elements of the exam are needed for a new patient level 4 E/M code? How many elements of the history of present illness are present? What are the different requirements for intermediate and comprehensive eye visit codes? Does this test require an interpretation or report?
Knowing the answers to these questions allows the tech to appropriately assist in fulfilling the necessary document requirements and prevent these types of claim denials.
Inappropriate codes
“As gas is to a car and electricity is to a light bulb, so are diagnosis codes (ICD- 10) to procedure (CPT) codes.” You need to have the correct CPT code for the procedure, test, or surgery associated with the correct diagnosis for the claim to be accepted by insurance.
Once we know the medical necessity requirements for specific services, we can actively look over the chart documentation to make sure the test and diagnosis are correctly linked. A necessary step is appropriately identifying laterality, coding to the highest level of specificity (avoid using unspecified codes), using the correct CPT code and modifier. “Scrubbing” documentation in this way by reviewing the documentation before the claims are sent to insurance can significantly decrease the amount of denials.
Missing or wrong modifiers
Did you know that certain tests and or surgeries are always bundled together? Sometimes a modifier allows these tests to be billed out, and sometimes they don’t. Modifiers tell the whole story to the payer and indicate that the test, surgery, or exam has been changed in some way.
The incorrect use or absence of a required modifier is one of the top five reasons claims are denied. Knowing how to use modifiers appropriately will help technicians understand some billing nuances and limitations.
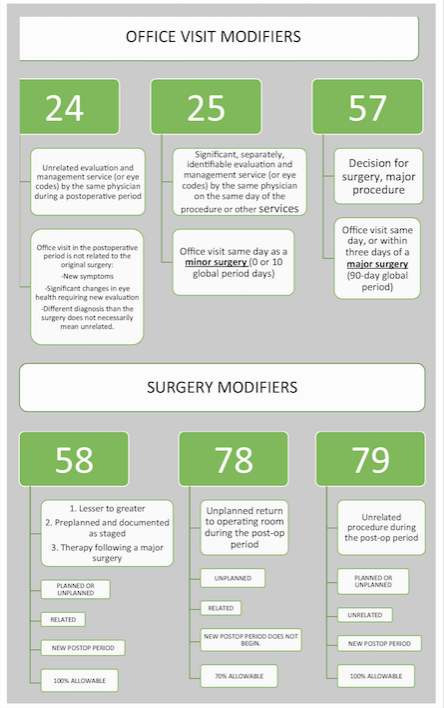
Modifiers can be appended to office visits (-24, -25, -57), diagnostic testing services (-RT, -LT, -TC, -26, -50, -59), and surgeries (-50, -54, -55, -58, -59, -78, -79, -RT, -LT).
Following is a helpful summary of how and when to use the most common office and surgery modifiers.
CCI edits
CCI edits are a list of services that are “bundled” or not individually payable when performed the same day. CCI edits affect the following in various combinations:
– Exams can be bundled with other exams.
– Exams can be bundled with tests.
– Tests are often bundled with other tests.
– Tests can be included with surgery bundles.
– Surgery can be combined with other same day/same session surgery.
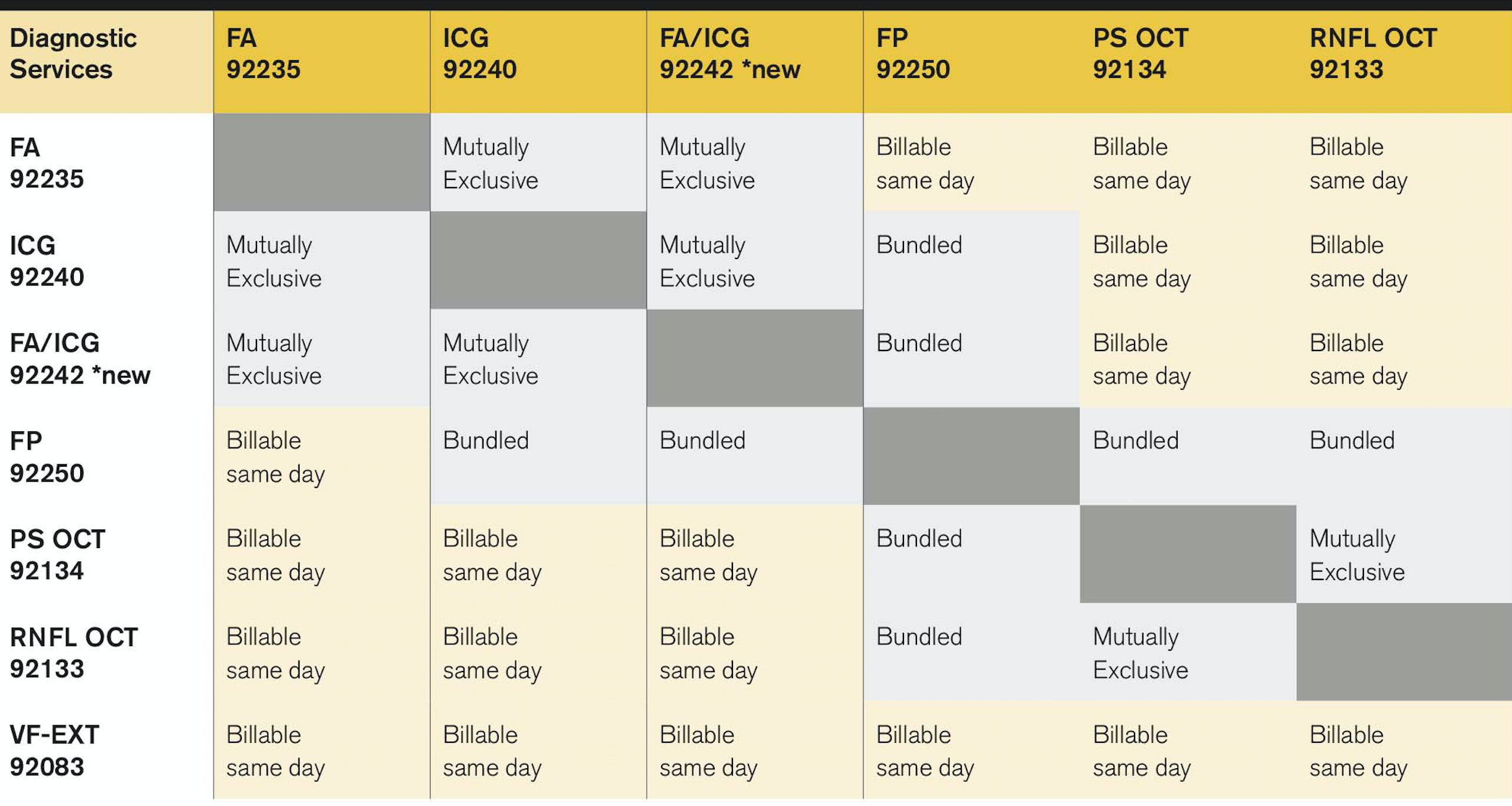
The next chart is a grid of which testing services are bundled together. The description “mutually exclusive” is used to describe a combination of tests that should never be unbundled (by using a modifier) unless a payer has a written policy that states it is OK to do so. Billing for a combination of tests that are bundled can be unbundled in specific situations (using a modifier).
Billable same-day combinations do not require the use of a modifier to be billed out. For example, when fluorescein angiography and indocyanine green chorioangiography are performed by two separate machines on the same patient, is only one of the tests billable? Which test? The answer: The one that gives the physician the information needed for diagnosis and or treatment.
Prior authorization not obtained
Prior authorizations are becoming a more common requirement for commercial insurance and Medicare Advantage plans. Although a prior authorization does not guarantee payment, no prior authorization guarantees no payment.
Technicians play a critical role in making sure prior authorizations are in place for tests and minor procedures that are performed in the clinic and minor rooms. Make a list of these common tests and procedures that require a prior authorization.
Medical vs. vision
Patients can have vision insurance coverage, which covers routine eye exams usually once per year and requires a “vision” diagnosis as the primary diagnosis, or medical insurance coverage, which covers medical eye problems and requires a medical diagnosis as a primary diagnosis.
What are vision diagnoses? Refractive diagnoses such as myopia, hyperopia, and presbyopia are typically billed for vision exams.
Some vision insurance plans also require the use of a Z code:
– Z01.00-encounter for examination of eyes and vision without abnormal findings
or
– Z01.0- encounter for examination of eyes and vision without abnormal findings
Medical diagnoses are anything pathologically occurring with the eyes: glaucoma, cataracts, macular degeneration, to name a select few. How many times do you hear this from a patient in response to your question of, “How can we help you,” or “What brings you in today?” “I am here for my yearly checkup” or “my annual eye exam” (or maybe even “I don’t know!”)?
These are not appropriate chief complaints and phrases that indicate that the patient would like to use his vision insurance. Technicians can communicate with physicians when patients want their vision insurance billed for this particular visit and if a medical concern is revealed during the exam, explain to the patient what the next step may be (consider billing medical insurance, returning for another visit to address the medical concern, potential out-of-pocket expenses if the patient has only vision coverage).
If the claim is sent to the wrong insurance or the correct primary diagnosis is not listed, this can be difficult and time-consuming to fix on the back end. The ideal process to handle the question of, “Is this exam medical or vision?” begins when the patient first makes the appointment, reinforced at registration and during the exam, communicated to the physicians, and then verified by scrubbing the documentation.
How does this knowledge boost my career?
The more you know, the more you can help. Just like learning about the anatomy of the eye, various diagnoses or procedures can help you help the patient and physician; learning about reasons claims are denied and how to prevent them can give you more tools to help patients, physicians, and your practice.
What type of technician do you want to be? Tech 1 has limited skills and tools to help the practice, like a pocketknife. Tech 2 has many skills and tools to help the practice, such as a Swiss army knife. Secondly, which technician is more valuable to the patient, physician, and practice: Tech 1 or Tech 2?
By increasing your skills and learning how to avoid claim denials you increase your value to your practice and enhance your ability to be of service to patients. With increased ability comes greater job satisfaction, stability, responsibilities, and possible growth opportunities.
How do I learn more?
We learn by doing, so try it out.
Start by auditing and scrubbing your own charts. Then contact your billing office/staff and identify top reasons why claims are being denied.
Next, discuss what you and the clinical team can do to help prevent these denials. Always use a trusted source.
Remember, learning about the coding and billing process can be overwhelming at times, but as you educate yourself using trusted sources, apply what you learn through practice, and communicate and implement the needed changes, you will become a valuable and indispensable part of the patient care team by helping fulfill the technician’s role in avoiding claim denials.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.