Top 5 reasons to request a retinal consult
Don’t fear the retina. Optometrists are able to diagnose and treat many retinal disorders. Remembering these 5 reasons to refer out will help you know when to ask for help and keep your patients in your practice-both of which create value for your patients.
In a practical sense, categories of retinal disease come to mind that could trigger a retinal consult. Broadly, when the macula is compromised by conditions amenable to surgery, these rise to the top of the list. Keeping with the theme of surgery, patients with retinal detachment not yet involving the macula come in a close second. So, let’s start down the road keeping in mind that other guidance includes those cases, in general, that threaten vision.
Because we have more efficient diagnostic methods than ever before, optometrists have the ability to make more detailed clinical determinations. This gives us information that, in conjunction with the philosophy of the consultant retina specialist, will create benefit for our patients. As primary-care providers with sophisticated diagnostic imaging at our disposal, we should respect-not fear-the retina.
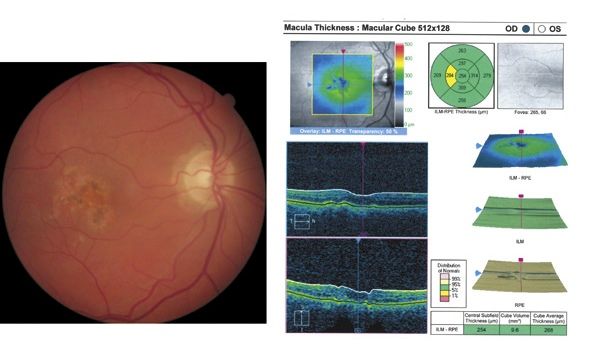
Figure 1. The right eye of a patient who had been followed for non-neovascular AMD for several years. He presented stating that he woke up in the middle of the night and could not see the middle digit on his alarm clock. Stereoscopic fundus examination revealed a subtle macular elevation consistent with CNVM, which was demonstrated on OCT.
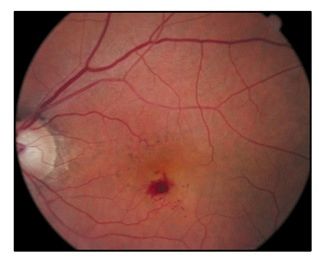
Figure 2. The left eye of a long-time patient who had undergone cataract surgery elsewhere and noticed recent vision loss. Note the subtle pigmentary changes surrounding the macula as well as the bright red appearance of blood in the macula suggesting its location above the RPE.
Getting started
Patients who present with painless vision loss of acute onset should be differentiated regarding etiology. The biggest differentiator is between optic nerve and macular disorders. Cerebrovascular etiologies, however, represent a separate category and are generally easily sorted out using visual field testing. Those patients often require systemic care or the services of a neurologist or neuro-ophthalmologist.
Etiologies involving the optic nerve have characteristic appearances-including pale nerve, swollen nerve, and hemorrhagic involvement of the nerve-and show color vision or contrast sensitivity deficits. In addition, they have visual field defects that correspond to the portion of the visual pathway involved. Macular etiologies are often visible at stereoscopic fundus examination.
Let’s begin with the category of proliferative macular disorders. The poster child here is choroidal neovascularization (CNV). While we all know what the hall-of-fame cases present and look like, sometimes these are subtle. Under the umbrella of age-related CNV would be choroidal neovascularization secondary to age-related macular degeneration (see Figure 1). A rarer macular proliferative disorder is retinal angiomatous proliferation (RAP) (see Figure 2). In each of these cases, restoration of the integrity of a compromised circulatory system (choroidal and retinal, respectively) may be amenable to an intravitreal injection of an ant-VEGF agent. At the surgeon’s suggestion and based on the patient’s preference, these may include, ranibizumab (Lucentis, Genentech), bevacizumab (Avastin, Genentech) or the more recently approved aflibercept (Eylea, Regeneron Pharmaceuticals).
Other disorders presenting with choroidal neovascularization include infectious etiologies, such as the histoplasmosis syndrome, CNV secondary to high myopia, macular teleangiectasia, polypoidal, and angioid streaks. Category one for a retinal consult would then be anything that involves choroidal neovascularization.
Diabetes and CSME
We all see patients with diabetes and are faced with varying degrees of compliance. It is particularly important to follow regularly those patients at greatest risk for developing clinically significant macular edema (CSME), which is the leading cause of vision loss among diabetics. When discussing the retina consult with patients, I relate the accumulation of fluid in the retina as akin to having a flood in the basement. The longer the water sits there, the worse the damage. The same is true of CSME. Making a diagnosis of CSME is often a clinical challenge at fundus examination. Subtle thickening of the retina may not be evident, which makes ancillary tests, such as photography and digital imaging, so helpful (see Figure 3). The definitions that qualify a fundus appearance as having CMSE center around retinal thickening (fluid accumulation) and evidence of exudate in proximity to the macula. Fluid accumulation representing CSME may be amenable to an anti-VEGF treatment as well, and deserves retinal consultation.
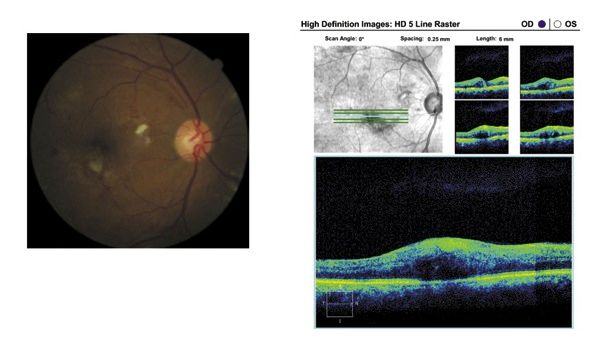
Figure 3. The left eye of a patient diagnosed with diabetes for over 20 years. In addition, he had been treated for systemic hypertension for that same period of time. Note the blurry grey area near the macula that represents fluid accumulation and corresponds with cystic spaces imaged at OCT.Another etiology of macular edema is secondary to retinal vein occlusion (RVO), an obstruction of small veins in the retina. Similar to CSME, these cases may respond to intravitreal anti-VEGF, but may be treated initially with a topical non-steroidal anti-inflammatory (NSAID). More rapid resolution is generally obtained with the former (see Figure 4).
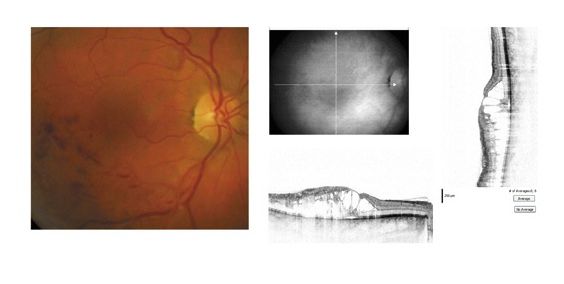
Figure 4. Macular edema following branch RVO. The macula is involved as seen in the fundus photo and the OCT demonstrates significant retinal disruption.Cystoid macular edema (CME) is not nearly as common following cataract surgery as was the case 2 decades ago, but still occurs occasionally. Since many of these cases are co-managed by optometrists, vigilance during the post-operative period is the paradigm. Vision loss or the observation of macular thickening, or demonstration of CME by digital imaging deserves a retinal consult. Neglect can result in vision loss as with CSME in diabetic patients (see Figure 5).
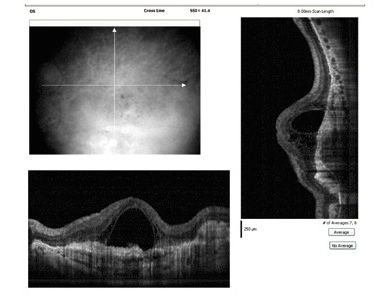
Figure 5. OCT of a patient following bilateral cataract extraction with IOL implantation. The VA is 20/200 in the case of late-onset macular edema.Vitreomacular abnormalities
The third category of retina-specialist consults would be those involving abnormal vitreomacular interactions. Several items fall under this heading. Vitreo-macular traction, per se, may be asymptomatic or go unnoticed by the patient. When visual disturbances prompt a visit to the optometrist, subtle changes may be difficult to detect at stereoscopic examination. We have learned much from OCT that substantiates histology and supports the original staging of this group of disorders. Macular hole formation is a leading cause of the sight-threatening entities. In many instances, the patient presents only following vision loss and fundus examination confirms the central defect. In other instances, precursors to full-thickness macular hole formation are seen at OCT and prompt closer follow-up of those patients at highest risk by either the optometrist or retinal surgeon (see Figure 6).
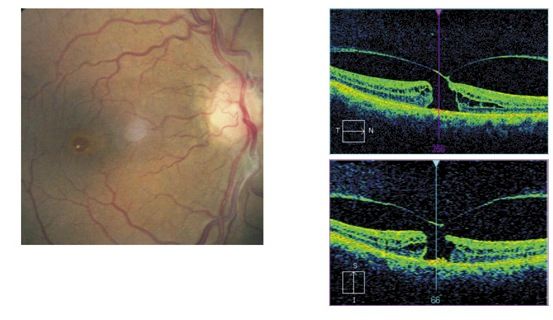
Figure 6. Macular hole formation in a 60-year-old patient. Note the small macular hole and vitreo-retinal defect in the fundus image and the characteristic appearance on OCT. (Photos courtesy of Leo Semes, OD, FAAO.)Leaving the posterior pole as a prompt for retina consult, fresh retinal detachment with intact macula would be next in the lineup. When patients become symptomatic with persistent flashing lights or a new-onset of floaters, the examining optometrist may observe red blood cells or RPE cells in the vitreous. Other characteristic clues to retinal detachment in the presence of symptoms are wrinkled retina/retinal vasculature, and obscured choroidal detail. When the macula remains attached, the prognosis for visual recovery is improved if the patient is attended to within 24-48 hours.
The fifth and final reason to obtain a retina consult would be when you just can’t figure it out. This is not intended as a cop-out suggestion. We should use all our diagnostic capabilities, background knowledge of anatomy, and the patient history to make a tentative diagnosis. When the possibilities are confusing and the prognosis is unknown, then appropriate consultation is in order. A further aspect of this fifth reason is to have a good understanding of your retina specialist’s management philosophies. Another component of such a relationship consists of good communication between the optometrist and the consultant. This also includes what the optometrist’s role in follow-up will be. All of those elements should be in place for the benefit of seamless patient care.
Finally, resist the urge to send a patient for a consult when the surgeon will be doing nothing more that you are capable of providing for the patient.ODT
Dr. Semes is a professor of optometry at the University of Alabama-Birmingham. He is a founding member of the Optometric Glaucoma Society and a founding fellow of the Optometric Retina Society.
Take-Home Message
Don’t fear the retina. Optometrists are able to diagnose and treat many retinal disorders. Remembering these 5 reasons to refer out will help you know when to ask for help and keep your patients in your practice-both of which create value for your patients.
Five reasons for requesting a retinal consult
- Anything that involves choroidal neovascularization.
- Patients with diabetes, at risk for developing clinically significant macular edema.
- Abnormal vitreo-macular vitreomacular interactions.
- Fresh retinal detachment with macula intact.
- When you just can’t figure it out.