Training Doctors vs. Training Technical Skills
The structure of training an optometrist, or any other professional, is to start with a strong foundation of knowledge and build on that. This is designed to create a level of expertise and skill that can adapt to changes in the profession and acclimate to any situation in any system. Strong comprehension of the basics is crucial for this level of education.
The structure of training an optometrist, or any other professional, is to start with a strong foundation of knowledge and build on that. This is designed to create a level of expertise and skill that can adapt to changes in the profession and acclimate to any situation in any system. Strong comprehension of the basics is crucial for this level of education.
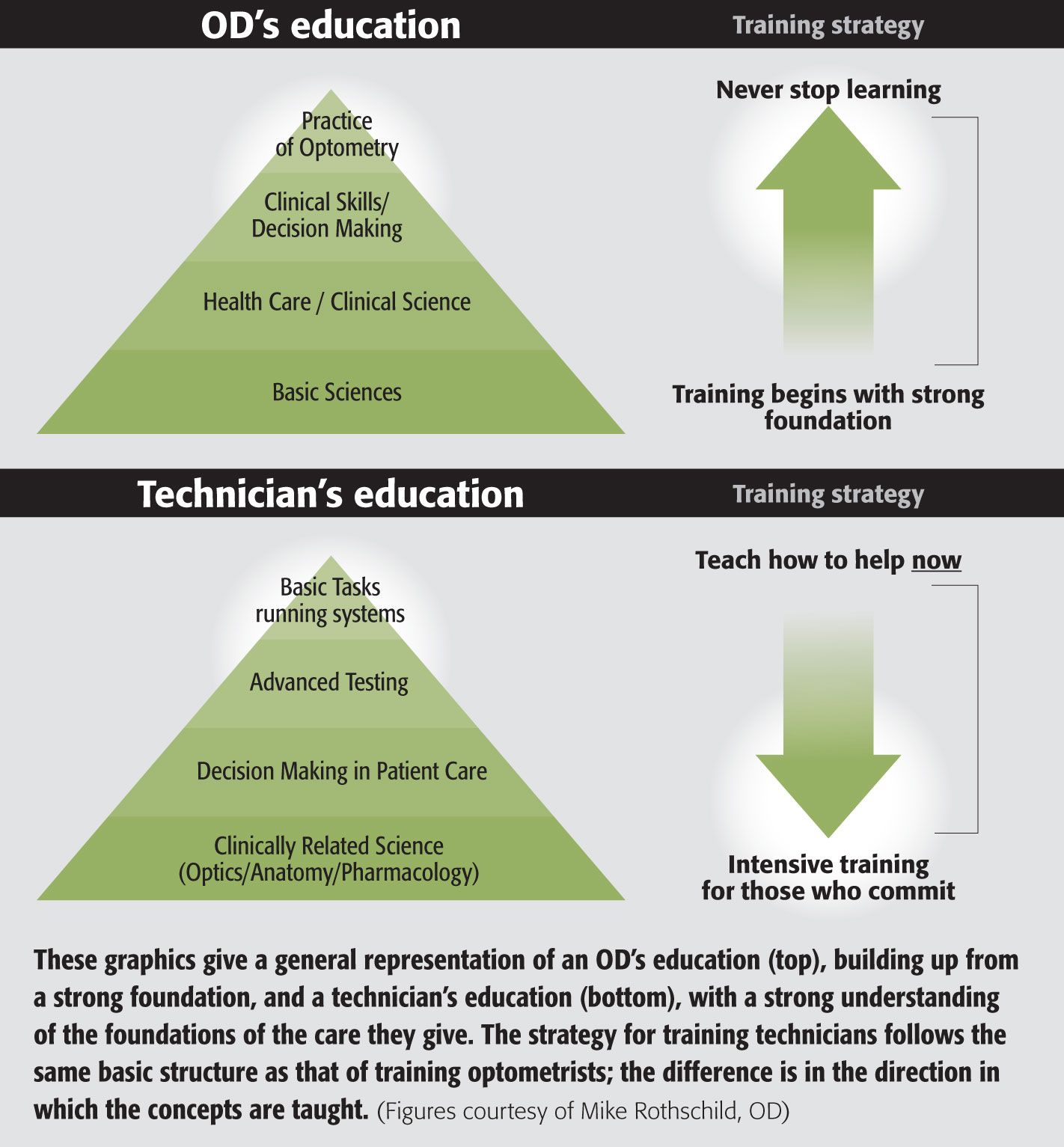
The following graphic give a general representation of an OD’s education, building up from a strong foundation:
How is training staff different?
We hire a new staff person not because we will need help in 4 years but because we need help now. Because our offices are set up as a series of systems, we hire someone to run those systems. This is why technical training should wait until later.
Many people argue that giving a quick lesson on the basics is important before teaching technical component of how to accomplish any given task. This is not true. It actually makes it more difficult to learn.
Maybe it is important that the new employee have a basic understanding of the tests that they perform. But it is important and urgent that someone is doing the test soon.
The technical training strategy has the same basic structure as the doctor’s educational strategy. This shows that the best employees have a strong understanding of the foundations of the care they give. The difference is the direction in which we teach it.
In our office, most new employees begin as technicians and the first thing we “train” them in is the auto-refraction and visual fields. We do this because it is the easiest to learn, the hardest to mess up, and it can have immediate impact on the flow of the office.
Here’s how:
1 - Make sure the patient is comfortable – Like this....
2 - Make sure the instrument is clean – Like this.....
(We do break our why rule here. We explain WHY it is important to clean the instrument in front of the patient or the staffer may try to improve efficiency and start cleaning between patients.)
3 – Read this script and push this button.
Congratulations! You are now an auto-refracting technician and we are better because you are here.
To put this concept into perspective, consider these two points:
·To understand basic refraction, you have to first understand basic ocular anatomy and basic optics. (If new employees don’t understand, you never know.)
·To operate an auto-refractor for the 2:00 patient, you need to know only how to push a button. (If they don’t understand, you will know very soon.)
Employees are eager to make a difference in the practice, and optics is not easy for someone who might have been selling shampoo last week. Resist the very natural urge to talk about “why” we do the test, and get straight to “how.” The “why” will come soon enough.
Note: Our first day of training is Day 3 on the job. Our first two days are reserved for Orientation which focuses on our Mission, our Values and the Basics of the practice.ODT
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.