Using precision medicine for dry eye
The Precision Medicine Initiative offers a model to customize treatment for each individual patient. Katherine M. Mastrota, MS, OD, FAAO, Dipl ABO explains why using precision medicine to treat dry eye disease can be beneficial for the OD and patient.

The Precision Medicine Initiative, a long-term research endeavor involving the National Institutes of Health (NIH) and multiple other research centers, aims to understand how a person’s genetics, environment, socioeconomic status and lifestyle can help determine the best approach to prevent or treat disease.
Recently, as I learned about the Precision Medicine Initiative in the Monroe J Hirsch Symposium at the American Academy of Optometry’s 2017 meeting in Chicago, I could not help thinking about “precision” management of dry eye for our patients.
Minorities under-represented
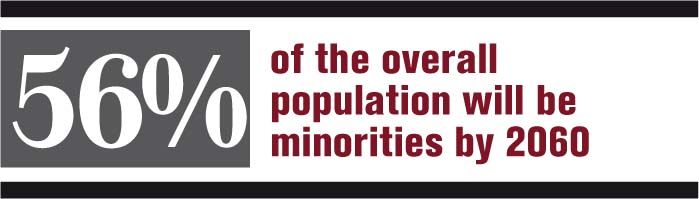
The Precision Medicine Initiative, under the banner of All of Us Research Program, will include minority and under-represented populations in its dataset. As an example, Dara Richardson-Heron, MD, NIH’s Chief Engagement Officer for the All of Us program, offered U.S. Census Bureau data that states minorities make up 38 percent of the population and that numbers are projected to rise to more than 56 percent of the overall population by 2060.1
Previously from Dr. Mastrota: How vaping affects the ocular surface
It is important to note that minorities are under-represented in important clinical trials overall. I wondered if under representation held true in dry eye trials as well. The goal of the All of Us Research Program, although not targeting dry eye and ocular surface disease (OSD) specifically, is to sequence the genome of one million volunteers.2
Employing precision medicine
Dr. Richardson-Heron explained that rather than using a cookie-cutter, one-size-fits-all approach to patient care, precision medicine aims to deliver “the right treatment, for the right person, at the right time” approach to disease management.
She paralleled the prescription of glasses to precision medicine-each Rx is finely tuned to the individual with attention not only on the Rx, but also the pupillary distance, base curve, and spectacle design.
Are we approaching this “precision medicine” approach in the diagnosis and management of OSD?
Precision medicine in your practice
We now have a myriad of diagnostics at our disposal such as LipiView (TearScience), LipiFlow (TearScience), LipiScan (TearScience), Keratograph 5M (Oculus), and Meibox (Box Medical Solutions) that can hone and tailor our thinking and management for patients with OSD. TearLab offers point-of-care testing to measure tear osmolarity, and InflammaDry (Quidel) serves as a biomarker of inflammation.
Related: How sleep affects the ocular surface
ODs are able to understand the rate and completeness of the blink. We can estimate with accuracy the height of the tear meniscus and the rate at which the surface of the tear film disintegrates. We can visualize the meibomian glands hidden within the tarsus-their number, length, width, degree of tortuosity, and caliber. We can test tear production and corneal sensitivity. At its limits, we can appreciate corneal physiology on a cellular level, evaluating ocular surface cell population types, and corneal nerve morphology.3
Every snippet of information gleaned from an OD’s available technology helps build a profile of OSD that is unique to each patient. This profile aids us in designing a care protocol built to address each individual case.
I can imagine how someday the information collected in the All of Us NIH research program effort may direct ODs in how we manage dry eye in distinct populations. Although we have notions and anecdotes of risk profiles for OSD and dry eye disease patients, we do acknowledge that we are far from a perfect understanding of dry eye disease.
References
1. United States Census Bureau. New Census Bureau Report Analyzes U.S. Population Projections. Available at: https://www.census.gov/newsroom/press-releases/2015/cb15-tps16.html. Accessed 12/14/17.
2. National Institutes of Health (NIH). All of Us Research Program. Available at:
. Accessed 12/14/17.
3. Hamrah P, Qazi Y, Shahatit B, Dastjerdi MH, Pavan-Langston D, Jacobs DS, Rosenthal P. Corneal Nerve and Epithelial Cell Alterations in Corneal Allodynia: An In Vivo Confocal Microscopy Case Series. Ocul Surf. 2017 Jan;15(1):139-151.




.png&w=3840&q=75)











