Using warm compresses to treat meibomian gland disease
Warm compresses (WCs) are commonly recommended as supplementary therapy for MGD as well as a number of other conditions of the eyelid. While the core therapy for MGD is to remove obstruction, which requires an in-office procedure, the therapeutic goal of adjunctive WC use is to heat the eyelids to help soften and partially melt any remaining material obstructing the glands.

Meibomian gland disease (MGD) is a chronic, progressive disease and the leading cause of dry eye1 (up to 86 percent of all dry eye sufferers have MGD).2 The prevalence of MGD in several large general Asian population-based studies has been found to be as high as 69 percent.3-5 Recent data from a general Caucasian clinical population, using appropriate metrics for diagnosis, indicates similarly high prevalence ~70 percent.6
Warm compresses (WCs) are commonly recommended as supplementary therapy for MGD as well as a number of other conditions of the eyelid.7 While the core therapy for MGD is to remove obstruction, which requires an in-office procedure, the therapeutic goal of adjunctive WC use is to heat the eyelids to help soften and partially melt any remaining material obstructing the glands.
The goal is to stabilize the tear film and provide the ocular surface with adequate defense against evaporative stress.8-13 In terms of supporting gland function, it has been established that warmer is better when it comes to WCs. This is especially true for more advanced disease.
However, warmer is not better for the ocular surface. The challenge with any form of front surface lid heating is to transfer therapeutic levels of heat to the meibomian glands (>40°C/104°F),14 while not risking thermal injury to the ocular surface or the skin.
Related: Diagnosing and treating dry eye with technology
The use of warm compresses
Warm compresses come in many designs, ranging from various homemade versions heated in a microwave to self-heating, commercially available masks and goggles. Some unique methods have been described to heat eyelids, including hard-boiled eggs, heating lamps, and even baked potatoes.15,16
Unfortunately, most patients performing WCs find themselves unenthusiastic about the procedure due in part to the lack of personal results, the laborious nature of the application, and/or the lack of instructions about how to optimize their efficacy.
A 2008 study determined the following key features to increase the effectiveness of a WC.17 WCs applied to the outer lid surface must maintain a consistent 45°C (113°F) in order for the therapeutic heat to reach the MGs, ideally >40°C (104°F).
Forty-five degrees Celsius, when the heat source is steadily cooling from the time of application, can be applied safely against the external eyelid skin without risking thermal injury for the duration of a treatment, but heat needs to be applied for a minimum of four to six minutes in order for the heat to pass through anatomical barriers that naturally shield the glands, e.g., skin, fat, the tarsal plate, and vasculature of the eyelids.
The compress needs to be replaced with a freshly heated compress every two minutes. In addition, because the cornea is more susceptible to corneal warpage when it is heated, patients should be advised not to massage their lids during or immediately after warm compress application.18
Related: A new tool for managing ocular surface disease
A recent study compared the efficacy of heat transfer to the outer and inner eyelid surfaces of eight different warm compress methods. The methods tested included several commercially available beaded masks, a chemically activated heating compress, a rice bag, an electronic mask, and two methods of applying moist heat.
The only compress which was shown to elevate inner eyelid surfaces (where the MGs are located) above a therapeutic temperature of 40°C after the 10-minute heating period was the heated moist towels that were wrapped in a bundle.
This method has been named the Bundle method. Because the performance of the Bundle method elevated all measured eyelid temperatures above a therapeutic 40°C, its design and preparation will be further described for practical use.19
Next: Bundle method preparation and use
Bundle method preparation and use
The Bundle method involves heating several moistened cloth towels, wrapped together, into a circular bundle as shown in Figure 1. The concentric geometry of the bundle facilitates heat retention of the inner towels while the outer towels are being used.
Making the bundle large enough to supply a 10-minute treatment eliminates the time and inconvenience of needing to reheat a warm compress during the treatment. This also frees the patient to conduct treatment at any comfortable location rather than having to remain near the microwave.
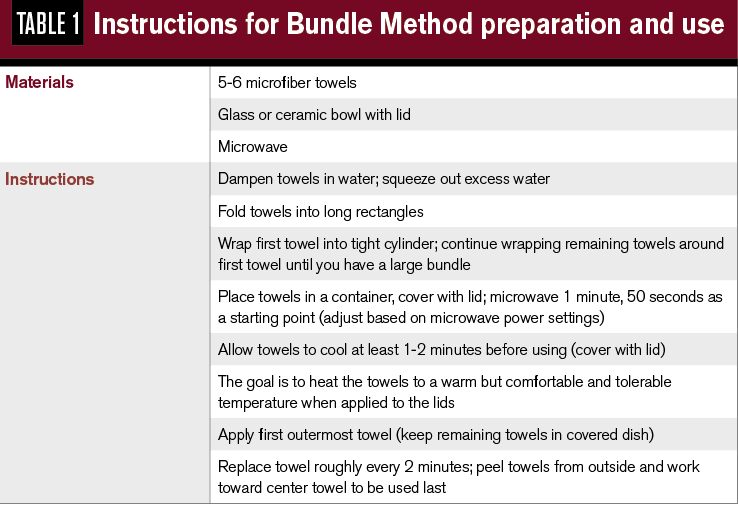
The following section details the necessary items to perform this method, along with how to prepare and heat the towels for use. A convenient reference is outlined in Table 1.
Related: Diagnosing and treating lagophthalmos

Step 1. Folding, wrapping, and wetting the towels in a bundle. Prior to wetting the towels, each cloth is folded, as shown in Figure 2. The first cloth is then rolled into a cylinder. The next cloth is wrapped around the first, and so on, until all of the cloths have been added to the bundle. The entire bundle is then rinsed in warm tap water until it is soaked, and then squeezed (using both hands to compress the circumference of the bundle) to remove excess water.
Step 2. Heating the bundle. The wet bundle is placed in a microwave-safe container as shown in Figure 3 and heated for about 1 minute and 50 seconds. It is beneficial to use a container with a lid for more rapid heating in the microwave and better heat retention after the bundle is removed from the microwave. Allow the bundle to cool for about one to two minutes.
Step 3. Applying the WCs from the bundle. The first WC is peeled from the bundle to begin the treatment when it can be safely applied to the outer eyelid without the patient feeling discomfort from the heat. This temperature will be ~ 45°C. If the outer towel is still too hot after up to two minutes of cooling, the patient should wait another 10 seconds and try again.
Step 4. Replacing the WC at regular intervals. Each WC lasts for approximately two minutes, during which time the temperature will have cooled such that the temperature is no longer in the therapeutic range. An egg timer or smartphone timer can be set to alert every two minutes when it is time to change from one WC to the next. The cooled towel is replaced with the next outermost towel from the bundle. The final towel at the center of the bundle is the most tightly rolled and thus tends to be much hotter at one end. Advise your patient to apply the heat from part of the towel that feels most consistent with previous towels.

Next: WC temperatures with the Bundle method
WC temperatures with the Bundle method
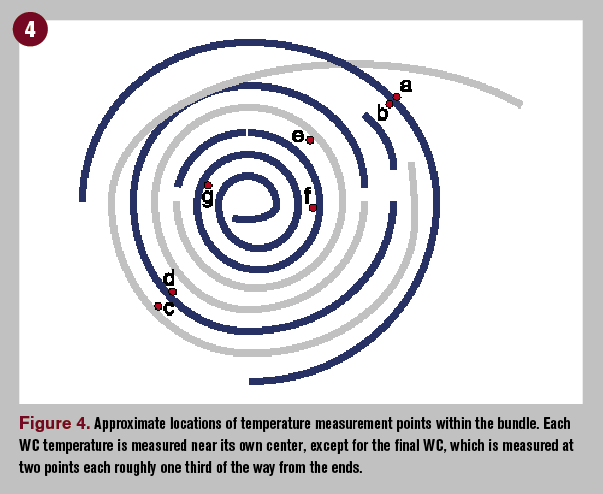
When the Bundle method was initially developed, a series of test bundles were prepared, and an infrared thermometer was used to quantify the varying temperatures among the towels in various situations: pre-heated baseline temperatures, temperature differences among the towels immediately after being heated, and the temperature of towels as they were pulled apart at regular intervals.
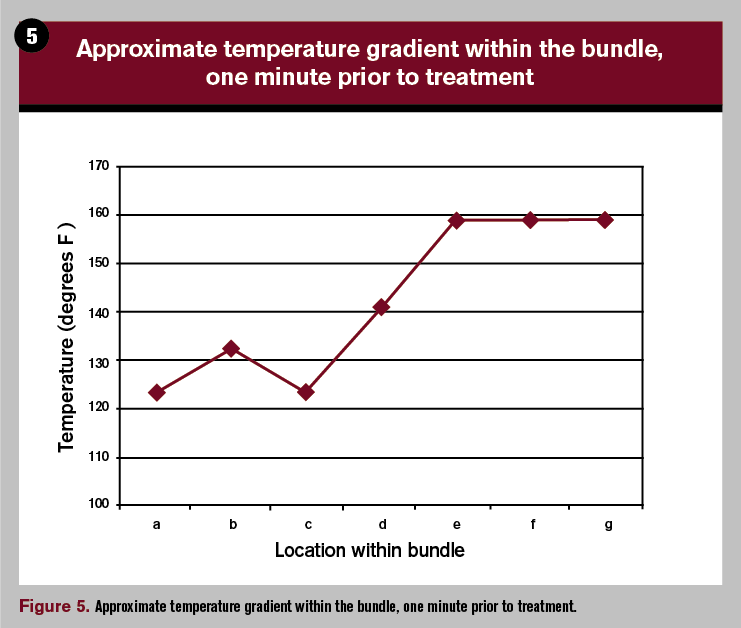
The approximate location within the bundle of the points measured is shown in Figure 4. The corresponding temperatures after being heated and one minute prior to treatment are plotted in Figure 5.
Prior to heating, the temperature of the exterior of the moistened bundle was found to be between 34°C and 42°C (94°F and 107°F.) Immediately after heating, the exterior cloth measured approximately 49-54°C (120-130°F), while the core of the bundle was between 66°C and 77°C (150°F and 170°F).
Related: Using the SPEED questionnaire to identify dry eye
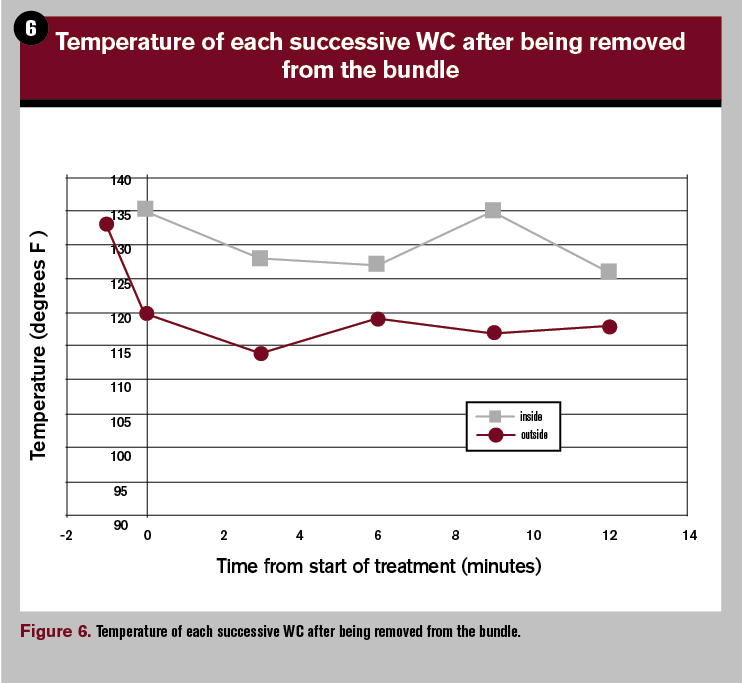
The temperature of each WC was measured when it was removed at regular intervals, mimicking an actual treatment. Both cotton and microfiber towels were tested with very consistent and similar results. The temperature was measured on the inner and outer surface of each cloth immediately after its removal from the bundle.
The outer temperature of the outermost WC was also measured upon removal from the microwave, one minute prior to commencement of the treatment. Figure 6 shows the temperature of each cloth at the moment when it is ready to be applied.
The outer surface of each of the five WCs was between 46°C and 49°C (115°F and 120°F,) just a few degrees above the ideal target of 45°C (113°F.) Each WC would require several seconds of air-cooling before it could be comfortably applied.
Next: Variations on the procedure and other tips
Variations on the procedure and other tips
Other key points to keep in mind include:
• Wait slightly longer if bundle remains too hot after removal from microwave. (A compress should never be applied too hot)
• The inner surface of each WC is considerably warmer than the outer surface
• The bundle retains heat better and cools slower than an individual WC; replacing a towel is quick when wrapped in a bundle and heated together
• Tailor the number of towels required to fit the needs of the patient-using more towels is useful for patients with more advanced stages of MGD who require longer periods of heat
• Lint-free microfiber cloths can be alternated for cotton washcloths. (Lightweight and inexpensive)
• Towels can be also be soaked individually before wrapping into a bundle
• Water temperature for initial wetting can vary-heat for a few additional seconds if cooler water is used
• Stress the importance of keeping towels clean by washing regularly
Next: Patient experience
Patient experience
The first author, a PhD in physics and a patient with MGD from a clinic in Boston, developed the bundle method. This method has been subsequently taught to and used by several additional patients at the same clinic, all of whom reported positive feedback and excellent compliance.
For the following two cases, patient symptoms were gathered with the SPEED Questionnaire (scored from 0 – 28)20 and MG function (the ability of a meibomian gland to release liquid oil during a deliberate blink) was assessed with a standardized meibomian gland evaluator (MGE).21
Related: Identify Sjögren’s patients with Sjö test
Case 1. A 46-year-old Caucasian female diagnosed with MGD was switched to the Bundle method when she reported that her compliance with a single-towel WC had been waning over the year prior. Her symptoms of eye dryness steadily increased from 5 to 8 over the previous year.
Using the MGE, only one functional gland was observed in each eye. After nine months of daily Bundle method WC application, the patient returned for a follow-up evaluation and reported that she had been “doing better” and was very enthusiastic with the Bundle method. Her symptom score was down to 4, which was half the value from her previous exam, nine months prior.
MG function also showed improvement in both eyes, with four to six functioning glands of each eyelid. It was also noted that all functional glands were also expressing significantly greater volume.
Case 2. A 43-year-old Caucasian female, using a daily single-towel WC since 2011, admitted that her compliance was poor. Her symptom score had increased from 6 to 8. There were two to three functional glands in each lower eyelid.
The Bundle method was recommended in November 2013. After 16 months of using the Bundle method WC, the patient reported her compliance was up to five to six days per week. The number of functional glands on each lower lid had doubled.
Interestingly, her symptoms showed no quantitative improvement despite her perception that she had improved. Given the chronicity of her condition and the progressive nature of MGD, it was clinically significant that her symptoms were not worsening.1
Next: Prescribing the Bundle method
Prescribing the Bundle method
Once MGD has been identified and the in-office treatment plan executed (removal of obstruction via manual expression of glands or via LipiFlow [TearScience] therapeutic procedure), the supplementary at-home therapy plan should be prescribed.
This plan frequently includes the use of self-administered front surface lid heating in the form of a WC. WCs prepared by the Bundle method have been shown to increase inner eyelid surface temperatures above a therapeutic level (>40°C or >104°F), if performed correctly.19
The general form of supplemental front surface lid heating is not as important as ensuring that the heat reaching the MGs falls within the therapeutic range (>40°C or >104°F) and that the patient is aware of the dangers of massaging the lids and globe during or immediately after heating.
Related: Screen younger patients for dry eye
When recommending a WC, clinicians should educate their patients that a consistent temperature of ~ 45°C is needed for a home-heated compress and that the WC should be used for a minimum of eight to 10 minutes.
We have found that compliance is greatly improved when patients are educated about the role of the supplemental therapy for MGD when they receive specific instructions how to prepare and use the WC (analogous to brushing and flossing our teeth, we understand that just rinsing will not be effective because we understand the individual roles of brushing and flossing).
The conventional approach to offer nonspecific instructions such as “use warm compresses daily” or “just heat a washcloth and hold it over your eyes for a few minutes” is ineffective. This vague approach minimizes the importance of the supplemental therapy and sets patients up for failure.
MGD is a prevalent, obstructive, and progressive disease. Our modern lifestyle, whereby we subject ourselves to chronic evaporative stress,22 places us all at risk for MGD; hence, the high reported prevalence of 60 to 70 percent.
There are many areas in which we can raise the level of awareness of MGD as well as greatly improve the standard of care we offer our patients by performing the necessary baseline MG evaluations on all patients.
However, in the interim, we can at least provide specific instructions for a self-administered efficacious WC such as is described with the Bundle method presented here.
Click here to read the latest dry eye news and advice from your colleagues
References:
1. Nichols KK, Foulks GN, Bron AJ, et al. The International Workshop on Meibomian Gland Dysfunction: Executive Summary. Invest Ophthalmol Vis Sci. 2011 Mar;52(4):1922-9.
2. Lemp MA, Crews LA, Bron AJ, et al. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012 May;31(5):472-8.
3. Lin PY, Tsai SY, Cheng CY, et al. Prevalence of dry eye among an elderly Chinese Population in Taiwan: the Shihpai Eye Study. Ophthalmology. 2003 Jun;110(6):1096-101.
4. Uchino M, Dogru M, Yagi Y et al. The features of dry eye disease in a Japanese elderly population. Optom Vis Sci. 2006 Nov;83:797-802.
5. Jie Y, Xu L, Wu YY, et al. Prevalence of dry eye among adult Chinese in the Beijing Eye Study. Eye (Lond). 2009 Mar;23:688-693.
6. Murakami DK, Blackie CA, Korb DR. The Prevalence of Meibomian Gland Dysfunction in a Caucasian Clinical Population. Poster presented at: The Association for Research in Vision and Ophthalmology; 2015 May 4-8; Denver, CO.
7. Olson MC, Korb DR, Greiner JV. Increase in tear film lipid layer thickness following treatment with warm compresses in patients with meibomian gland dysfunction. Eye Contact Lens. 2003 Apr;29:96-99
8. Gifford SR. Meibomian glands in chronic blepharoconjunctivitis. Am J Ophthalmol. 1921;4:489–94.
9. Korb DR, Henriquez AS. Meibomian gland dysfunction and contact lens intolerance. J Am Optom Assoc. 1980 Mar;51(3):243–51.
10. Geerling G, Tauber J, Baudouin C, et al. The International Workshop on Meibomian gland dysfunction: Report of the subcommittee on management and treatment of meibomian gland dysfunction. Ophthalmol and Vis Sci. 2011 Mar 30;52(4):2050-64.
11. Goto E, Endo K, Suzuki A, et al. Improvement of tear stability following warm compression in patients with meibomian gland dysfunction. Adv Exper Med Biol. 2002;506(Pt B):1149–52.
12. Korb DR, Baron DF, Herman JP, et al. Tear film lipid layer thickness as a function of blinking. Cornea. 1994 Jul;13(4):354-9.
13. Arita R, Morishige N, Shirakawa R, Sato Y. Comparison of effect of five warming devices onto tear functions, meibomian glands and ocular surface. Poster presented at: The Association for Research in Vision and Ophthalmology; 2014 May 4-8; Orlando, FL.
14. Bron AJ, Tiffany JM, Gouveia SM, et al. Functional aspects of the tear film lipid layer. Exp Eye Res. 2004 Mar;78(3):347-60.
15. Lam A, Lam C. Effect of warm compress therapy from hard-boiled eggs on corneal shape. Cornea. 2007;26(2):162-67.
16. Nichols KK. Let’s ask Siri a dry eye question. Optom Management. 2012. Mar;47, 66-69.
17. Blackie CA, Solomon JD, Greiner JV, et al. Inner Eyelid Surface Temperatures as a function of warm compress methadology. Opt Vis Sci. 2008 Aug;85(8):675-83.
18. McMonnies C, Korb D, Blackie C. The Role of heat in rubbing and massage-related corneal deformation. Contact Lens Anterior Eye. 2012;35:148-154
19. Murakami DK, Blackie CA, Korb DR. All warm compresses are not equally efficacious. Optom Vis Sci. 2015 Jul 8.
20. Ngo W, Situ P, Keir N, et al. Psychometric properties and validation of the standard patient evaluation of eye dryness questionnaire. Cornea. 2013. Sep;32(9):1204-10.
21. Korb DR, Blackie CA. Meibomian Gland Diagnostic Expressibility: Correlation with dry eye symptoms and gland location. Cornea. 2008 Dec;27(10):1142-7.
22. Suhalim JL et al. Effect of desiccating stress on mouse meibomian gland function. Ocul Surf. 2014 Jan;12(1):59-68.