Welcoming myopia modalities into optometric practice
Incorporate management of disease as the new standard of care.
By 2050, 50% of the world’s population is expected to have myopia.1 The prevalence of that population progressing to high myopia (over –5.00) is also expected to increase more than 5-fold in the next 30 years.1
Once identified, it is clear there is need to intervene in myopia progression as soon as possible to prevent increased risk of ocular disease (retinal detachment, glaucoma, myopic macular degeneration, etc).2-4
With the treatments now available, how do practitioners decide which myopia control option to start with? When would a practitioner consider combining different modalities for increased efficacy?
Related: Podcast: Sheila Morrison, OD reviews the latest in myopia management
Treatment options
Current optical designs for treatment of myopia are based on the theory of peripheral defocus. These corrections focus peripheral light rays onto the inside of the peripheral retina (myopic defocus).

There is no peripheral hyperopic defocus, which usually would send a signal to the eye to grow longer. Undercorrection of myopia repeatedly has been shown to either have no effect on the elongation of the eye or to cause a slightly faster progression.5-7
Spectacles
Lately, there has been a lot of interest in spectacle options for myopia control because of their ease of use. Historically, spectacles have had a less than optimal treatment efficacy.
Based on the 2003 COMET study (NCT00000113), progressive addition lenses (PAL) only offer a 14% reduction in progression on refraction (0.20 diopters [D]) and axial length (0.11 mm).8
Interestingly, patients with a higher lag of accommodation and near esophoria showed a 30% reduction in progression. Still, the magnitude of slowing found with progressive addition lens (PAL) use is insignificant compared with recent advances in lens design with peripheral defocus optics.
Related: Misight 1 day contact lenses show no rebound effect in children, new data reveals
With the recent launch of MiyoSmart (Hoya) spectacle lenses with Defocus Incorporated Multiple Segments (DIMS) technology in Canada, spectacles can now offer 59% refractive slowing (0.44 D) and 60% axial length slowing (0.34 mm) over a 2-year period.9
This is a significant improvement on other earlier peripheral focus designs that were far less effective with roughly 33% refractive slowing and 20% axial length slowing.10
In Canada, options like the Kikko (SightGlass Vision) and anticipated Stellest (Essilor) lenses have shown promising clinical data as well, cementing spectacle lenses as another tool for practitioners to confidently recommend to patients.
Soft contact lenses
Contact lenses are an excellent choice for myopia control because the peripheral defocus optics move with the eye, always staying in the ideal position.
Daily lenses are the preferred option for children because of convenience of use and low risk of complications compared with extended wear designs. MiSight (omafilcon A; CooperVision) lenses are the first FDA-approved contact lenses for the purpose of myopia control.
Their dual-focus design has been shown to significantly slow both axial length and spherical equivalent compared with placebo in their initial 3-year study.11
Follow-up data found that even treating older children and teenagers with MiSight had a significant impact in slowing progression.12 Final 7-year data investigating whether there is a rebound effect after discontinuing wear is expected to be published soon.
Related: The safety and efficacy of mass-produced colored contact lenses
The anticipated Acuvue Abiliti soft lens (Johnson & Johnson Vision) was recently approved by Health Canada as an on-label treatment for myopia. It will be interesting to see whether this technology will soon be available in the United States.
When discussing off-label lenses with patients, it is important to counsel on the lenses’ intended use and hopes for treatment outcomes. Regular follow-ups are critical to ensure treatment goals are being met, especially with off-label options.
Other off-label lens options include daily disposable NaturalVue (extended depth of focus lens from Visioneering Technologies, Inc) as well as monthly disposable Biofinity (CooperVision) center-distance (CD) multifocals (MF).
The latter was used in the recent Blink Study,13 which found high (+2.50) CD MF lenses are more effective in slowing myopia (both refraction and axial length) compared with lower add powers or single vision. These lenses are also an option for patients with astigmatism because toric CD MF parameters are now available.
Another option for astigmatism is the Duette Progressive (SynergEyes) hybrid lenses, which can be ordered with up to +5.00 add power in the CD design.
Related: Five ways to stand out with specialty contact lenses
The new extended depth of focus iD design is a new addition to the SynergEyes lens family. This lens comes in a high power and has the potential to be used for off-label myopia control as well.
Orthokeratology
Orthokeratology (Ortho-K) uses a reverse geometry design made with high oxygen permeable rigid materials to temporarily shape the cornea, providing peripheral optical defocus and slowing myopia progression.14,15
When fitted appropriately, these lenses offer freedom from wearing spectacles or contact lenses during the day and the benefit of slowing myopia progression.
Ortho-K success depends on ensuring parents are aware myopia treatment is a long-term process.
Parents need to understand the course of treatment, including the importance of regular follow-ups. Axial length elongation is the best indicator in measuring success; however, most parents go by their child’s report of clear unaided vision.16
Parents need to understand the importance of regular follow-ups, because relying on vision alone is not the best way of optimizing treatment outcomes.
Parents and children must also understand the risks of nonadherence to treatment recommendations, including following cleaning procedures and replacing accessories.
Related: Contact lens overwear leads to short-term, long-term consequences
Supporting clinical data studying the effect of orthokeratology on myopia progression are expanding every year.
Overall, Ortho-K has been found more effective in slowing axial elongation than glasses during the early treatment of myopia in children.17
Ortho-K has also been found more effective in slowing axial elongation than 0.02% atropine in children with higher myopia over a period of 2 years.18 It is important to consider this when deciding which treatment to recommend to patients first.
With such a large range in available lens designs, a recent study found that a relatively smaller treatment zone size and larger treatment zone decentration may be beneficial in slowing myopia in children with orthokeratology treatment.19
It is not clear why treatment zone decentration contributes to the slowing of myopia, but increased coma symmetry and increased corneal symmetry have been suggested.20
Related: Give toric ortho-k lenses a try
Another study found similar results when looking at the impact of a 5-mm vs 6-mm back optic zone diameter (BOZD). This study showed the smaller BOZD led to a smaller treatment zone and, over a 1-year period, a retardation of axial length by 0.13 mm compared to the larger BOZD.21
The clinical implication from these studies is yet to be determined. It is an exciting time to offer these treatments because new designs and materials are released frequently.
Atropine
The mechanism of action of atropine in myopia control is still debated, but atropine has been shown to cause a slight thickening of the choroid in young healthy adults.22
The ATOM studies proved low-dose atropine could slow progression of myopia by roughly 50%,23 and that there is comparable refractive control with 0.01%, 0.1%, and 0.5% atropine.
Of the 3 concentrations, 0.01% caused less of a rebound response after discontinuing treatment.24
The LAMP study investigated 0.05%, 0.025%, and 0.01% atropine to determine whether better control could be demonstrated than that shown in the ATOM studies.25
This study showed that 0.05% atropine had double the efficacy compared with 0.01% atropine, with a very similar adverse effect (AE) profile. Clinically, these new findings have shifted practice patterns to prescribing 0.05% first, and only reducing to 0.025% if AEs are noted by the patient, especially for young myopes.
Related: COVID-19 pandemic increases myopia prevalence in children
Clinical context
The 4 main pillars of myopia control are clear. What may be murkier is deciding which option is most appropriate for each patient. Generally, this decision starts with a discussion with the patient and their parent(s).
At the baseline examination, all treatment options should be discussed. Even if a patient chooses a particular option now, it does not mean they may not want to change to a different option in the future.
Contact lens options can be offered regardless of patient age, but key indicators for success include willingness of parents to be involved in handling and cleaning of the lenses if necessary, as well as the patient’s own maturity level and motivation for contact lens wear.
We have all met extremely motivated 5-year-old and 6-year-old patients who insert and remove their lenses with confidence, whereas there are 13-year-old patients who cannot be bothered to try contact lenses.
Because myopia progression generally slows over time, looking at percentage reductions in refraction year over year is not the most reliable way to determine whether patients are responding to treatment well.
Formulas from Jones et al (2005) also provide a good estimate for what normal axial length growth should be. Comparing your patient’s growth with these values is helpful in differentiating between normal age-related growth and myopic progression.26
Figure 1. Axial length growth percentage charts for Chinese schoolchildren.27
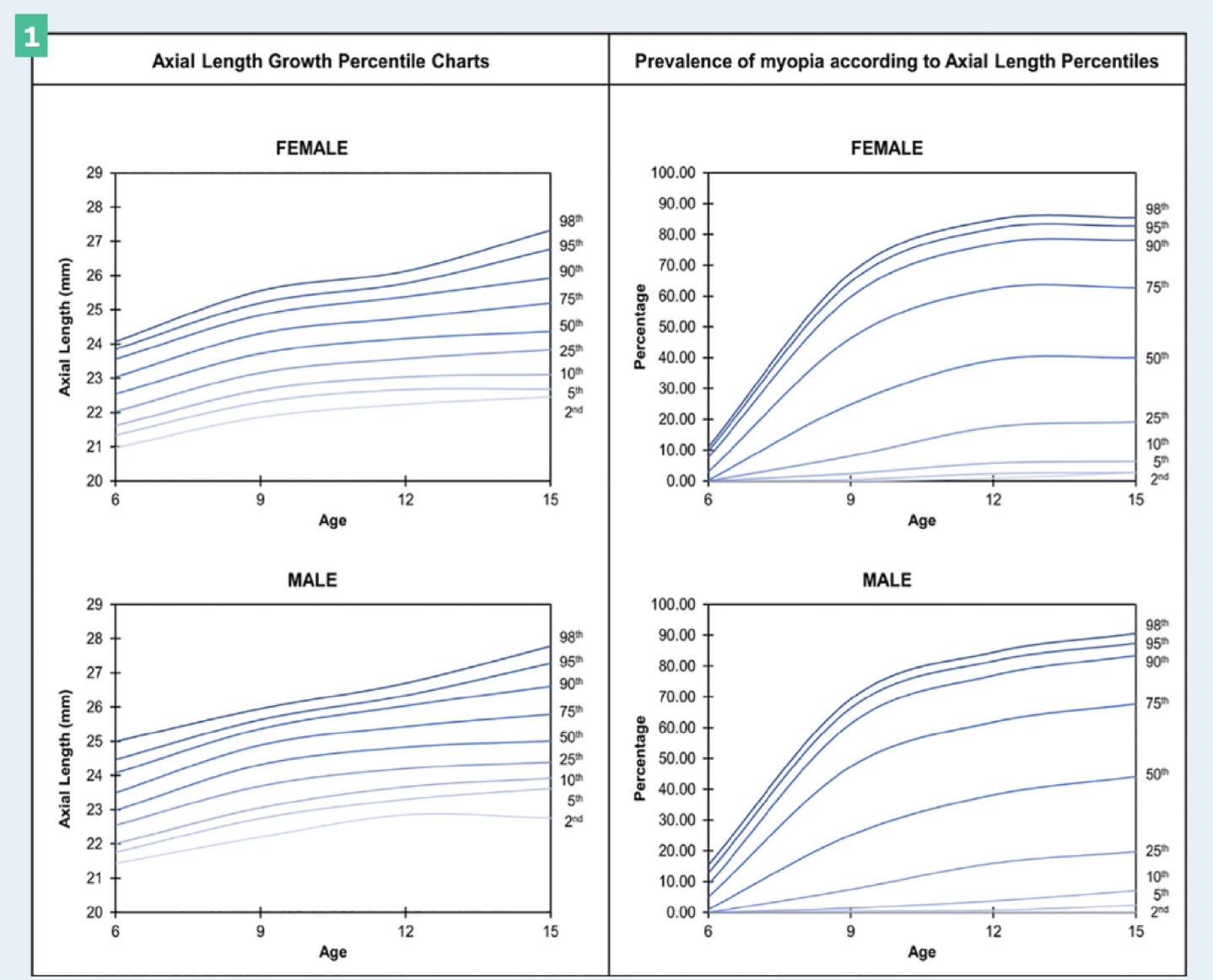
Figure 2. Axial length growth charts for European study subjects with the risk of myopia in adulthood. The myopia percentage on these charts represents the proportion of myopia halfway above and below the percentage line.28 (Images courtesy of Andrea Lasby, OD, FAAO, FSLS.)
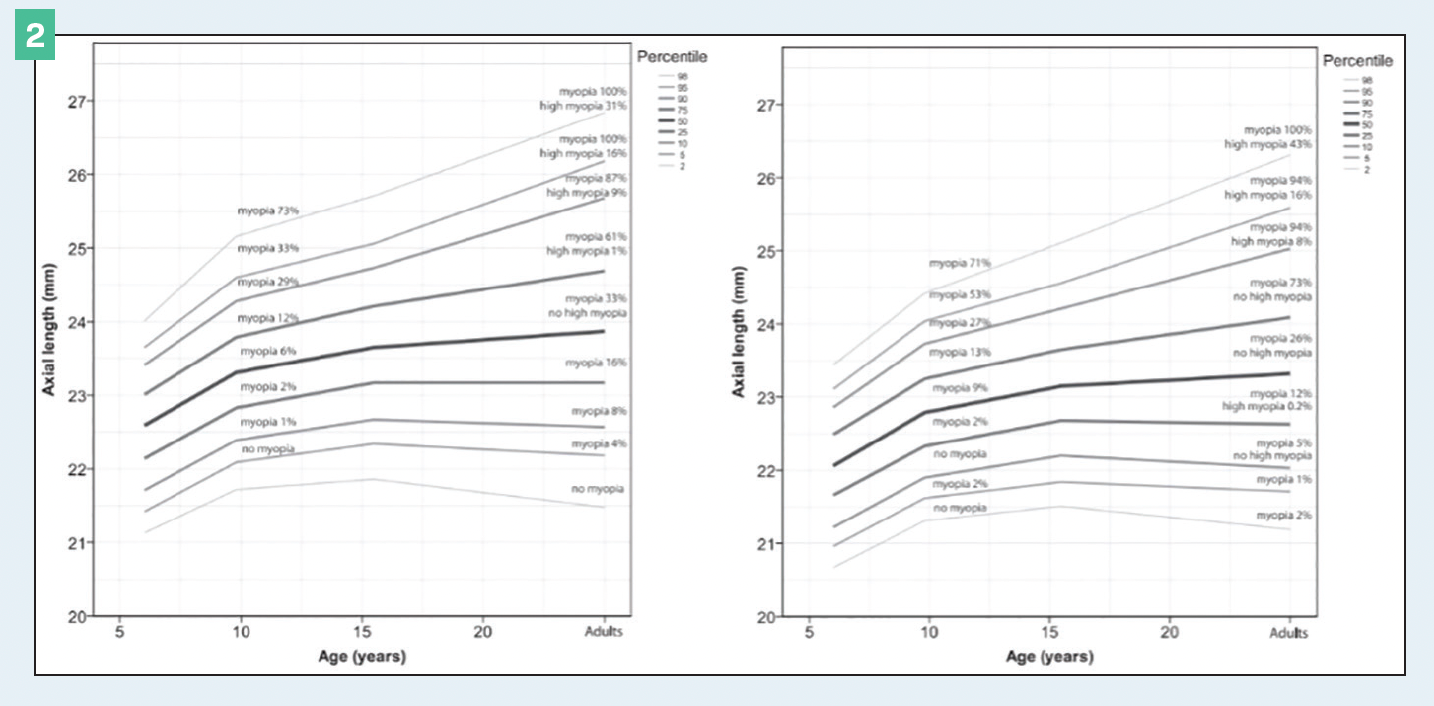
Figure 1 and Figure 2 show charts that are simple to print for parents, and plot where their child’s axial length may compare with averages. This is an excellent tool for initial discussion and treatment choice, but also to monitor progression over time.
There are several studies showing that combining low-dose atropine with spectacle or contact lens designs has an additive effect on the slowing of myopia.29-31
We often start with one form of treatment and then add atropine if expected slowing is not observed.
There are some cases where we recommend starting with combination therapy (atropine + glasses/soft contact lenses/orthokeratology) from the beginning. Imagine a 12-year-old White female patient presents for her first assessment.
Axial length measurement is 24.5 mm OU, and refraction is –2.50 D OU. She reports last year her refraction was –1.00 D OU. Comparing her with Tideman et al’s growth chart, her axial length places her near the 98th percentile for her age and sex.
Both parents reveal they themselves have pathological myopia with refractive powers over –8.00 D OU. One parent has been treated in the past for a retinal detachment.
In a case like this, we tend to start with 0.05% atropine every night at bedtime in each eye as well as full-time contact lens wear (Ortho-K or a soft contact lens would be appropriate in this situation).
Related: Experts offer tips for sucess in contact lens practice
For children who progress very quickly, we generally monitor every 4 months rather than every 6 months, which is typical for a myopia control patient in our practice.
The future of myopia control may not be waiting until myopia is established to begin treatment. The most exciting new research that is being done is on children who are not yet myopic.
Even years before myopia onset, axial length elongates on average 0.37 mm/y for children who later became myopic, compared with 0.14 mm/y for emmetropic children32 (Singaporean population).
It has been shown that using one drop of 0.025% atropine every night at bedtime in each eye in premyopic children (< +1.00 D) can prevent the onset of myopia over a 1-year period compared with placebo.33
As biometry becomes more available to optometrists, it may not seem too far-fetched to include axial length measurements in every child’s eye examination for early detection of axial elongation.
Implementation of preventive measures could be recommended before onset of myopia. More data are necessary before this becomes standard of care, but the future of myopia control is exciting.
Changing practice patterns
The World Council of Optometry recently advised optometrists to incorporate myopia management as standard of care.
This means early and frequent discussion with parents about what myopia is, lifestyle factors affecting myopia, the risks to long-term ocular health that accompany myopia, and the available evidence-based interventions now available for myopia.
At the end of the day, it is our responsibility as practitioners to do something.
They say an ounce of prevention is worth a pound of cure, and optometrists should be ready to take up this responsibility.
See more myopia and contact lens coverage
References
1. Holden BA, Fricke TR, Wilson DA, et al.Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-1042. doi:10.1016/j.ophtha.2016.01.006
2. Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012;31(6):622-660. doi:10.1016/j.preteyeres.2012.06.004
3. Bullimore MA, Brennan NA. Myopia control: why each diopter matters. Optom Vis Sci. 2019;96(6):463-465. doi:10.1097/OPX.0000000000001367
4. Chua SYL, Sabanayagam C, Cheung YB, et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol Opt. 2016;36(4):388-394. doi:10.1111/opo.12305
5. Chung K, Mohidin N, O’Leary DJ. Undercorrection of myopia enhances rather than inhibits myopia progression. Vision Res. 2002;42(22):2555-2559. doi:10.1016/s0042-6989(02)00258-4
6. Adler D, Millodot M. The possible effect of undercorrection on myopic progression in children. Clin Exp Optom. 2006;89(5):315-321. doi:10.1111/j.1444-0938.2006.00055.x
7. Vasudevan B, Esposito C, Peterson C, Coronado C, Ciuffreda KJ. Under-correction of human myopia—is it myopigenic?: a retrospective analysis of clinical refraction data. J Optom. 2014;7(3):147-152. doi:10.1016/j.optom.2013.12.007
8. Gwiazda J, Hyman L, Dong LM, et al; Comet Group. Factors associated with high myopia after 7 years of follow-up in the Correction of Myopia Evaluation Trial (COMET) cohort. Ophthalmic Epidemiol. 2007;14(4):230-237. doi:10.1080/01658100701486459
9. Lam CSY, Tang WC, Tse DYY, et al. Defocus Incorporated Multiple Segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial. Br J Ophthalmol. 2020;104(3):363-368. doi:10.1136/bjophthalmol-2018-313739
10. Sankaridurg P, Donovan L, Varnas S, et al. Spectacle lenses designed to reduce progression of myopia: 12-month results. Optom Vis Sci. 2010;87(9):631-641. doi:10.1097/OPX.0b013e3181ea19c7
11. Chamberlain P, Peixoto-de-Matos SC, Logan NS, Ngo C, Jones D, Young G.A 3-year randomized clinical trial of MiSight lenses for myopia control. Optom Vis Sci. 2019;96(8):556-567. doi:10.1097/OPX.0000000000001410
12. Chamberlain P, Hammond D, Arumugam B, Bullimore MA. Measured and predicted axial elongation in the MiSight 1 day clinical trial: 6-year results. Presented at: Association for Research in Vision and Ophthalmology 2021 Annual Meeting; May 1-7, 2021; virtual. Accessed January 7, 2022. https://iovs.arvojournals.org/article.aspx?articleid=2775361
13. Walline JJ, Walker MK, Mutti DO, et al; BLINK Study Group. Effect of high add power, medium add power, or single-vision contact lenses on myopia progression in children: the BLINK randomized clinical trial. JAMA. 2020;324(6):571–580. doi:10.1001/jama.2020.10834
14. Lipson MJ, Brooks MM, Koffler BH. The role of orthokeratology in myopia control: a review. Eye Contact Lens. 2018;44(4):224-230. doi:10.1097/ICL.0000000000000520
15. Vincent SJ, Cho P, Chan KY, et al. CLEAR - Orthokeratology. Cont Lens Anterior Eye. 2021;44(2):240-269. doi:10.1016/j.clae.2021.02.003
16. Chang LC, Li FJ, Sun CC, Liao LL. Trajectories of myopia control and orthokeratology compliance among parents with myopic children. Cont Lens Anterior Eye. 2021;44(4):101360. doi:10.1016/j.clae.2020.08.004
17. Guan M, Zhao W, Geng Y, et al. Changes in axial length after orthokeratology lens treatment for myopia: a meta-analysis. Int Ophthalmol. 2020;40(1):255-265. doi:10.1007/s10792-019-01167-9
18. Lyu Y, Ji N, Fu AC, et al. Comparison of administration of 0.02% atropine and orthokeratology for myopia control. Eye Contact Lens. 2021;47(2):81-85. doi:10.1097/ICL.0000000000000699
19. Lin W, Li N, Gu T, et al. The treatment zone size and its decentration influence axial elongation in children with orthokeratology treatment. BMC Ophthalmol. 2021;21(1):362. doi:10.1186/s12886-021-02123-x
20. Lau JK, Vincent SJ, Cheung SW, Cho P. Higher-order aberrations and axial elongation in myopic children treated with orthokeratology. Invest Ophthalmol Vis Sci. 2020;61(2):22. doi:10.1167/iovs.61.2.22
21. Guo B, Cheung SW, Kojima R, Cho P. One-year results of the Variation of Orthokeratology Lens Treatment Zone (VOLTZ) study: a prospective randomised clinical trial. Ophthalmic Physiol Opt. 2021;41(4):702-714. doi:10.1111/opo.12834
22. Sander BP, Collins MJ, Read SA. Short-term effect of low-dose atropine and hyperopic defocus on choroidal thickness and axial length in young myopic adults. J Ophthalmol. 2019;2019:4782536. doi:10.1155/2019/4782536
23. Chua W, Balakrishnan V, Tan D, Chan Y; ATOM Study Group. Efficacy results from the Atropine in the Treatment of Myopia (ATOM) study. Investig Ophthalmol Vis Sci. 2003;44(13):3119.
24. Chia A, Chua WH, Cheung YB, et al. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2). Ophthalmology. 2012;119(2):347-354. doi:10.1016/j.ophtha.2011.07.031
25. Yam JC, Li FF, Zhang X, et al. Two-year clinical trial of the Low-concentration Atropine for Myopia Progression (LAMP) study: phase 2 report. Ophthalmology. 2020;127(7):910-919. doi:10.1016/j.ophtha.2019.12.011
26. Jones LA, Mitchell GL, Mutti DO, Hayes JR, Moeschberger ML, Zadnik K. Comparison of ocular component growth curves among refractive error groups in children. Invest Ophthalmol Vis Sci. 2005;46(7):2317-2327. doi:10.1167/iovs.04-0945
27. Sanz Diez P, Yang LH, Lu MX, Wahl S, Ohlendorf A.Growth curves of myopia-related parameters to clinically monitor the refractive development in Chinese schoolchildren. Graefes Arch Clin Exp Ophthalmol. 2019;257(5):1045-1053. doi:10.1007/s00417-019-04290-6
28. Tideman JWL, Polling JR, Vingerling JR, et al. Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol. 2018;96(3):301-309. doi:10.1111/aos.13603
29. Tan Q, Ng AL, Cheng GP, Woo VC, Cho P. Combined atropine with orthokeratology for myopia control: study design and preliminary results. Curr Eye Res. 2019;44(6):671-678. doi:10.1080/02713683.2019.1568501
30. Huang J, Mutti DO, Jones-Jordan LA, Walline JJ. Bifocal & Atropine in Myopia study: baseline data and methods. Optom Vis Sci. 2019;96(5):335-344. doi:10.1097/OPX.0000000000001378
31. Wang S, Wang J, Wang N. Combined orthokeratology with atropine for children with myopia: a meta-analysis. Ophthalmic Res. 2021;64(5):723-731. doi:10.1159/000510779
32. Rozema J, Dankert S, Iribarren R, Lanca C, Saw SM. Axial growth and lens power loss at myopia onset in Singaporean children. Invest Ophthalmol Vis Sci. 2019;60(8):3091-3099. doi:10.1167/iovs.18-26247
33. Fang PC, Chung MY, Yu HJ, Wu PC. Prevention of myopia onset with 0.025% atropine in premyopic children. J Ocul Pharmacol Ther. 2010;26(4):341-345. doi:10.1089/jop.2009.0135
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.